Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (33): 5332-5338.doi: 10.3969/j.issn.2095-4344.2017.33.014
Previous Articles Next Articles
Multiple imaging evaluation on the therapeutic efficacy of coronary artery bypass graft combined with autologous stem cell transplantation for myocardial infarction
Lu Guo-xiu1, Hao Shan-hu1, Wang Zhi-guo1, Zhang Tong1, Wang Hui-shan2, Zhang Guo-xu1
- 1Department of Nuclear Medicine, 2Department of Cardiac Surgery, the General Hospital of Shenyang Military Command, Shenyang 110016, Liaoning Province, China
-
Revised:2017-06-21Online:2017-11-28Published:2017-12-01 -
Contact:Zhang Guo-xu, Master, Chief physician, Department of Nuclear Medicine, the General Hospital of Shenyang Military Command, Shenyang 110016, Liaoning Province, China -
About author:Luo Guo-xiu, Master, Attending physician, Department of Nuclear Medicine, the General Hospital of Shenyang Military Command, Shenyang 110016, Liaoning Province, China -
Supported by:the First-Batch Scientific and Technological Projects in Liaoning Province in 2012, No. 2012225019
CLC Number:
Cite this article
Lu Guo-xiu, Hao Shan-hu, Wang Zhi-guo, Zhang Tong, Wang Hui-shan, Zhang Guo-xu. Multiple imaging evaluation on the therapeutic efficacy of coronary artery bypass graft combined with autologous stem cell transplantation for myocardial infarction[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(33): 5332-5338.
share this article
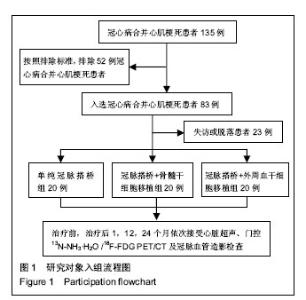
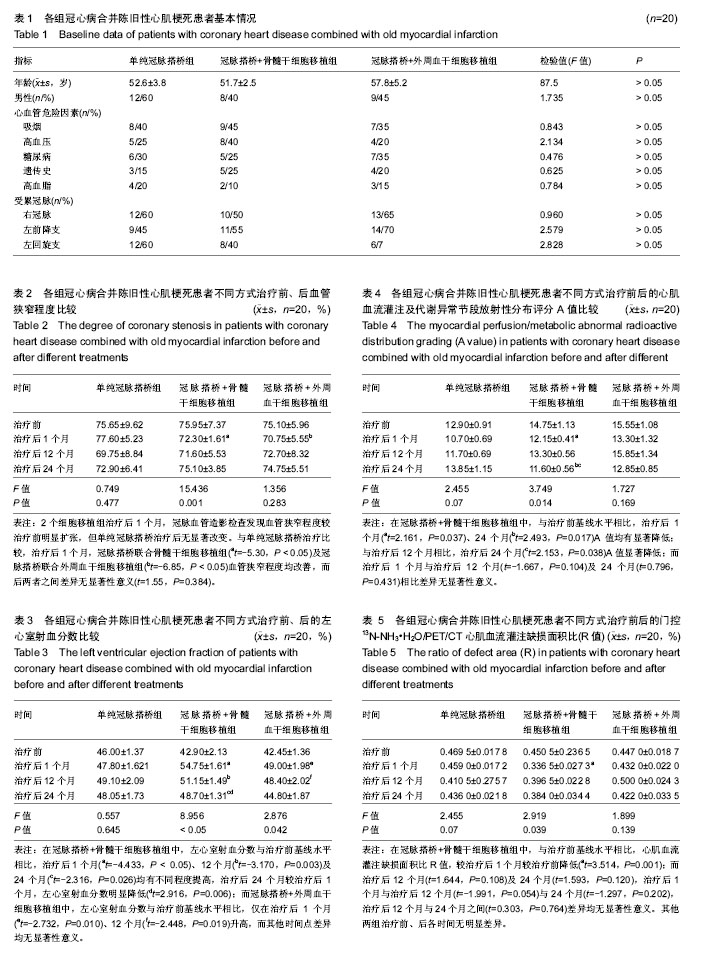
2.1 参与者数量分析 60例患者在治疗后成功随访2年,无严重并发症发生,全部进入结果分析。 2.2 各组患者基本临床信息 见表1。3组患者年龄、性别、心血管危险因素、受累冠脉比较差异无显著性意义(P > 0.05),具有可比性。 2.3 研究对象入组流程图 见图1。 2.4 冠脉血管造影及超声图像结果 60例患者术前检查发现30%存在冠状动脉中度狭窄(18/60),70%为重度狭窄(42/60);总计95支冠状动脉不同程度受累。针对相应病灶血管进行冠脉搭桥手术(平均1.58段/人)及联合干细胞移植治疗。3组患者治疗后血管狭窄程度均较治疗前改善(t=13.648,P < 0.05),以治疗后1个月效果显著(F=15.436,P < 0.05)。3组间差异无显著性意义(F=1.356,P > 0.05),见表2。通过心脏超声观察冠脉搭桥+骨髓干细胞移植组、冠脉搭桥+外周血干细胞移植组,治疗后12个月左心室射血分数升高(F=6.254,P=0.004);而其他时间点,3组左心室射血分数治疗前、后变化差异无显著性意义,见表3。 2.5 门控PET/CT显像结果 门控13N-NH•H2O/18F-FDG PET/CT诊断存活心肌的灵敏度、特异度、阳性预测值及阴性预测值分别为92.1%,85.6%,93.4%及78.4%。3组患者中,冠脉搭桥+骨髓干细胞移植组门控13N-NH3•H2O/ 18F-FDG PET/CT心肌血流灌注及代谢异常节段放射性分布评分A值,在治疗前、后不同时间点不同程度减低(F=3.749,P=0.014)。而其他两组门控13N-NH3•H2O/18F-FDG PET/CT心肌血流灌注及代谢异常节段放射性分布评分A值,在治疗前、后不同时间点差异无显著性意义(F=1.484,P=0.226,F=1.899,P=0.139)。冠脉搭桥+骨髓干细胞移植组,治疗前、后心肌13N-NH3•H2O血流灌注及18F-FDG代谢缺损面积比减低(F=2.919,P=0.039),以治疗后1个月较治疗前减低明显(t=3.514,P=0.001),而其他时间点之间差异均无显著性意义;其他两组治疗前、后心肌13N-NH3•H2O血流灌注及18F-FDG代谢缺损面积比减低差异均无显著性意义(F=1.484,P=0.226,F=1.899,P=0.139),见表4,5。 冠脉搭桥联合骨髓干细胞移植组中,治疗前后不同时间点,心肌门控13N-NH3•H2O/ PET/CT心肌血流灌注缺损面积比(R值),差异有显著性意义(F=2.919,P=0.039)。而单独冠脉搭桥组及冠脉搭桥联合外周血干细胞移植治疗组中,治疗前后不同时间点,R值无明显差异(F=2.455,P=0.070;F=1.899,P=0.139)。冠脉搭桥联合骨髓干细胞移植组治疗1个月后心肌血流灌注缺损面积比,较治疗前下降(t=2.161,P=0.037),而治疗后不同时间点间比较差异无显著性意义。 2.6 不良反应 60例患者在动员过程中发生骨痛4例,感觉乏力3例,心绞痛5例。"
| [1] Beeres SL, Atsma DE, van Ramshorst J, et al. Cell therapy for ischaemic heart disease. Heart. 2008;94(9):1214-1226.[2] Corrêa Ada G, Makdisse M, Katz M, et al. Analysis Treatment Guideline versus Clinical Practice Protocol in Patients Hospitalized due to Heart Failure. Arq Bras Cardiol. 2016; 106(3):210-217.[3] 薛杨,赵江民.干细胞移植治疗急性心肌梗死MRI示踪的研究进展[J].医学研究杂志,2016,45(9):172-179.[4] Boden WE. Management of chronic coronary disease: is the pendulum returning to equipoise. Am J Cardiol. 2008; 101(10A):69D-74D.[5] Kinnaird T, Stabile E, Burnett MS, et al. Marrow-derived stromal cells express genes encoding a broad spectrum of arteriogenic cytokines and promote in vitro and in vivo arteriogenesis through paracrine mechanisms. Circ Res. 2004;94(5):678-685.[6] Ott HC, Davis BH, Taylor DA. Cell therapy for heart failure-muscle, bone marrow, blood, and cardiac-derived stem cells. Semin Thorac Cardiovasc Surg. 2005;17(4): 348-360.[7] 蒙莫珂,杨淑莲.干细胞移植治疗心肌梗死的研究进展[J].中国老年学杂志,2011,31(9):1714-1716.[8] Suresh SC, Selvaraju V, Thirunavukkarasu M, et al. Thioredoxin-1 (Trx1) engineered mesenchymal stem cell therapy increased pro-angiogenic factors, reduced fibrosis and improved heart function in the infarcted rat myocardium. Int J Cardiol. 2015;201:517-528.[9] Hou L, Kim JJ, Woo YJ, et al. Stem cell-based therapies to promote angiogenesis in ischemic cardiovascular disease. Am J Physiol Heart Circ Physiol. 2016;310(4):H455-465.[10] Teng X, Chen L, Chen W, et al. Mesenchymal Stem Cell-Derived Exosomes Improve the Microenvironment of Infarcted Myocardium Contributing to Angiogenesis and Anti-Inflammation. Cell Physiol Biochem. 2015;37(6):2415-2424.[11] Kim SW, Jin HL, Kang SM, et al. Therapeutic effects of late outgrowth endothelial progenitor cells or mesenchymal stem cells derived from human umbilical cord blood on infarct repair. Int J Cardiol. 2016;203:498-507.[12] Kang HJ, Kim HS, Zhang SY, et al. Effects of intracoronary infusion of peripheral blood stem-cells mobilised with granulocyte-colony stimulating factor on left ventricular systolic function and restenosis after coronary stenting in myocardial infarction: the MAGIC cell randomised clinical trial. Lancet. 2004;363(9411):751-756.[13] Zohlnhöfer D, Kastrati A, Schömig A. Stem cell mobilization by granulocyte-colony-stimulating factor in acute myocardial infarction: lessons from the REVIVAL-2 trial. Nat Clin Pract Cardiovasc Med. 2007;4 Suppl 1:S106-109.[14] Lunde K, Solheim S, Aakhus S, et al. Intracoronary injection of mononuclear bone marrow cells in acute myocardial infarction. N Engl J Med. 2006;355(12):1199-1209.[15] Das P, Clavijo LC, Nanjundappa A, et al. Revascularization of carotid stenosis before cardiac surgery. Expert Rev Cardiovasc Ther. 2008;6(10):1393-1396.[16] 汪娇,李剑明. 18F-FDG PET 心肌代谢显像在心肌存活诊断中的应用进展[J].国际放射医学核医学杂志,2015,39(3):252-256.[17] Cremer P, Hachamovitch R, Tamarappoo B. Clinical decision making with myocardial perfusion imaging in patients with known or suspected coronary artery disease. Semin Nucl Med. 2014;44(4):320-329.[18] Eitzman D, al-Aouar Z, Kanter HL, et al. Clinical outcome of patients with advanced coronary artery disease after viability studies with positron emission tomography. J Am Coll Cardiol. 1992;20(3):559-565.[19] Nekolla SG, Martinez-Moeller A, Saraste A. PET and MRI in cardiac imaging: from validation studies to integrated applications. Eur J Nucl Med Mol Imaging. 2009;36 Suppl 1: S121-130.[20] Mäki MT, Koskenvuo JW, Ukkonen H,et al. Cardiac Function, Perfusion, Metabolism, and Innervation following Autologous Stem Cell Therapy for Acute ST-Elevation Myocardial Infarction. A FINCELL-INSIGHT Sub-Study with PET and MRI. Front Physiol. 2012;3:6.[21] 苏航,王蒨,董微,等.核素心肌灌注显像和CT冠状动脉造影检测冠状动脉心肌桥所致心肌血液供应异常[J].中华核医学与分子影像杂志,2014,34(2):112-115.[22] Beanlands RS, Youssef G. Diagnosis and prognosis of coronary artery disease: PET is superior to SPECT: Pro. J Nucl Cardiol. 2010;17(4):683-695.[23] Cerqueira MD. Diagnosis and prognosis of coronary artery disease: PET is superior to SPECT: Con. J Nucl Cardiol. 2010;17(4):678-682.[24] Rohatgi R, Epstein S, Henriquez J, et al. Utility of positron emission tomography in predicting cardiac events and survival in patients with coronary artery disease and severe left ventricular dysfunction. Am J Cardiol. 2001;87(9): 1096-1099.[25] Herrero P, McGill J, Lesniak DS, et al. PET detection of the impact of dobutamine on myocardial glucose metabolism in women with type 1 diabetes mellitus. J Nucl Cardiol. 2008;15(6):791-799.[26] De Stefano E, Delay D, Horisberger J, et al. Initial clinical experience with the admiral oxygenator combined with separated suction. Perfusion. 2008;23(4):209-213.[27] 高方明,古孜丽,杨小丰. PET/ CT评价冠心病患者存活心肌的价值[J].新疆医学,2008,38(12):117-119.[28] Siminiak T, Kalawski R, Fiszer D, et al. Autologous skeletal myoblast transplantation for the treatment of postinfarction myocardial injury: phase I clinical study with 12 months of follow-up. Am Heart J. 2004;148(3):531-537.[29] Poole JC, Quyyumi AA. Progenitor Cell Therapy to Treat Acute Myocardial Infarction: The Promise of High-Dose Autologous CD34(+) Bone Marrow Mononuclear Cells. Stem Cells Int. 2013;2013:658480.[30] Matsumoto K, Takahashi N, Ishikawa T, et al. Evaluation of myocardial glucose metabolism before and after recovery of myocardial function in patients with tachycardia-induced cardiomyopathy Pacing Clin Electrophysiol. 2006;29(2): 175-180.[31] Zhang S, Ma X, Yao K, et al. Combination of CD34-positive cell subsets with infarcted myocardium-like matrix stiffness: a potential solution to cell-based cardiac repair. J Cell Mol Med. 2014;18(6):1236-1238.[32] Kurbonov U, Dustov A, Barotov A, et al. Intracoronary Infusion of Autologous CD133(+) Cells in Myocardial Infarction and Tracing by Tc99m MIBI Scintigraphy of the Heart Areas Involved in Cell Homing. Stem Cells Int. 2013;2013:582527.[33] Mackie AR, Klyachko E, Thorne T, et al. Sonic hedgehog- modified human CD34+ cells preserve cardiac function after acute myocardial infarction. Circ Res. 2012;111(3):312-321.[34] Xue J, Du G, Shi J, et al. Combined treatment with erythropoietin and granulocyte colony-stimulating factor enhances neovascularization and improves cardiac function after myocardial infarction. Chin Med J (Engl). 2014; 127(9): 1677-1683.[35] Wang JS, Shum-Tim D, Galipeau J, et al. Marrow stromal cells for cellular cardiomyoplasty: feasibility and potential clinical advantages. J Thorac Cardiovasc Surg. 2000; 120(5): 999-1005.[36] Schmuck EG, Koch JM, Hacker TA, et al. Intravenous Followed by X-ray Fused with MRI-Guided Transendocardial Mesenchymal Stem Cell Injection Improves Contractility Reserve in a Swine Model of Myocardial Infarction. J Cardiovasc Transl Res. 2015;8(7):438-448.[37] Hua P, Tao J, Liu JY, et al. Cell transplantation into ischemic myocardium using mesenchymal stem cells transfected by vascular endothelial growth factor. Int J Clin Exp Pathol. 2014;7(11):7782-7788.[38] Tong J, Ding J, Shen X, et al. Mesenchymal stem cell transplantation enhancement in myocardial infarction rat model under ultrasound combined with nitric oxide microbubbles. PLoS One. 2013;8(11):e80186.[39] Sedov VM, Nemkov AS, Afanas'ev BV, et al. Effectiveness of using autologous mono-nuclears of the bone marrow in treatment of patients with ischemic heart disease.Vestn Khir Im I I Grek. 2006;165(4):11-14.[40] Mocini D, Colivicchi F, Santini M. Stem cell therapy for cardiac arrhythmias. Ital Heart J. 2005;6(3):267-271.[41] Pannitteri G, Petrucci E, Testa U. Coordinate release of angiogenic growth factors after acute myocardial infarction: evidence of a two-wave production. J Cardiovasc Med (Hagerstown). 2006;7(12):872-879. |
| [1] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [2] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [3] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [4] | Yin Tingting, Du Dayong, Jiang Zhixin, Liu Yang, Liu Qilin, Li Yuntian. Granulocyte colony-stimulating factors improve myocardial fibrosis in rats with myocardial infarction [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 730-735. |
| [5] | He Yunying, Li Lingjie, Zhang Shuqi, Li Yuzhou, Yang Sheng, Ji Ping. Method of constructing cell spheroids based on agarose and polyacrylic molds [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 553-559. |
| [6] | He Guanyu, Xu Baoshan, Du Lilong, Zhang Tongxing, Huo Zhenxin, Shen Li. Biomimetic orientated microchannel annulus fibrosus scaffold constructed by silk fibroin [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 560-566. |
| [7] | Chen Xiaoxu, Luo Yaxin, Bi Haoran, Yang Kun. Preparation and application of acellular scaffold in tissue engineering and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 591-596. |
| [8] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [9] | Shen Jiahua, Fu Yong. Application of graphene-based nanomaterials in stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 604-609. |
| [10] | Zhang Tong, Cai Jinchi, Yuan Zhifa, Zhao Haiyan, Han Xingwen, Wang Wenji. Hyaluronic acid-based composite hydrogel in cartilage injury caused by osteoarthritis: application and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 617-625. |
| [11] | Li Hui, Chen Lianglong. Application and characteristics of bone graft materials in the treatment of spinal tuberculosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 626-630. |
| [12] | Gao Cangjian, Yang Zhen, Liu Shuyun, Li Hao, Fu Liwei, Zhao Tianyuan, Chen Wei, Liao Zhiyao, Li Pinxue, Sui Xiang, Guo Quanyi. Electrospinning for rotator cuff repair [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 637-642. |
| [13] | Guan Jian, Jia Yanfei, Zhang Baoxin , Zhao Guozhong. Application of 4D bioprinting in tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 446-455. |
| [14] | Liu Jiali, Suo Hairui, Yang Han, Wang Ling, Xu Mingen. Influence of lay-down angles on mechanical properties of three-dimensional printed polycaprolactone scaffolds [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2612-2617. |
| [15] | Huang Bo, Chen Mingxue, Peng Liqing, Luo Xujiang, Li Huo, Wang Hao, Tian Qinyu, Lu Xiaobo, Liu Shuyun, Guo Quanyi . Fabrication and biocompatibility of injectable gelatin-methacryloyl/cartilage-derived matrix particles composite hydrogel scaffold [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2600-2606. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||