Chinese Journal of Tissue Engineering Research ›› 2014, Vol. 18 ›› Issue (35): 5577-5582.doi: 10.3969/j.issn.2095-4344.2014.35.001
Blood loss and limb circumference changes in patients undergoing unilateral total knee arthroplasty after intra-articular injection of tranexamic acid: a randomized controlled trial
Ma Jin-hui, Sun Wei, Gao Fu-qiang, Wang Yun-ting, Li Zi-rong.pdf
- Department of Orthopedics, China-Japan Friendship Hospital, Peking University, Beijing 100029, China
-
Revised:2014-06-15Online:2014-08-27Published:2014-08-27 -
Contact:Sun Wei, Chief physician, Associate professor, Master’s supervisor, Department of Orthopedics, China-Japan Friendship Hospital, Peking University, Beijing 100029, China -
About author:Ma Jin-hui, Studying for master’s degree, Department of Orthopedics, China-Japan Friendship Hospital, Peking University, Beijing 100029, China -
Supported by:the National Natural Science Foundation of China (General Program), No. 81372013; the General Program of China-Japan Friendship Hospital, No. 2013-MS-27
CLC Number:
Cite this article
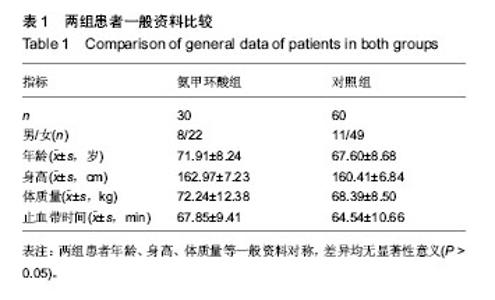
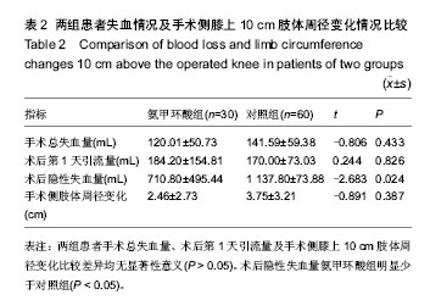
Ma Jin-hui, Sun Wei, Gao Fu-qiang, Wang Yun-ting, Li Zi-rong. Blood loss and limb circumference changes in patients undergoing unilateral total knee arthroplasty after intra-articular injection of tranexamic acid: a randomized controlled trial[J]. Chinese Journal of Tissue Engineering Research, 2014, 18(35): 5577-5582.
share this article
| [1] Ferraris VA, Brown JR, Despotis GJ, et al. 2011 update to the Society of Thoracic Surgeons and the Society of Cardiovascular Anesthesiologists blood conservation clinical practice guidelines. Ann Thorac Surg. 2011;91(3):944-982. [2] Lemaire R. Strategies for blood management in orthopaedic and trauma surgery. J Bone Joint Surg Br. 2008;90(9): 1128-1136. [3] 高福强,李子剑,张克,等.初次全膝关节置换术后隐性失血的影响因素研究[J].中华外科杂志, 2011, 49(5): 419-423. [4] Li B, Wen Y, Wu H, et al. The effect of tourniquet use on hidden blood loss in total knee arthroplasty.Int Orthop. 2009; 33(5):1263-1268. [5] Fahmy NR, Patel DG. Hemostatic changes and postoperative deep-vein thrombosis associated with use of a pneumatic tourniquet. J Bone Joint Surg Am. 1981;63(3):461-465. [6] Nakahara M, Sakahashi H. Effect of application of a tourniquet on bleeding factors in dogs. J Bone Joint Surg Am. 1967;49(7):1345-1351. [7] Madjdpour C, Spahn DR. Allogeneic red blood cell transfusions: efficacy, risks, alternatives and indications. Br J Anaesth. 2005;95(1):33-42. [8] Abrishami A, Chung F, Wong J. Topical application of antifibrinolytic drugs for on-pump cardiac surgery: a systematic review and meta-analysis. Can J Anaesth. 2009; 56(3):202-212. [9] Tobias JD. Strategies for minimizing blood loss in orthopedic surgery. Semin Hematol. 2004;41(1 Suppl 1): S145-156. [10] Sabatini L, Trecci A, Imarisio D, et al. Fibrin tissue dhesive reduces postoperative blood loss in total knee arthroplasty. J OrthopTraumatol. 2012;13(3):145-151. [11] McCormack PL. Tranexamic Acid: a review of its use in the treatment of hyperfibrinolysis. Drugs. 2012;72(5): 585-617. [12] Ahlberg A, Eriksson O, Kjellman H. Diffusion of tranexamic acid to the joint. Acta Orthop Scand. 1976;47(5): 486-488. [13] Ker K, Edwards P, Perel P, et al. Effect of tranexamic acid on surgical bleeding: systematic review and cumulative meta-analysis. BMJ. 2012;344:e3054. [14] Soni A, Saini R, Gulati A, et al. Comparison Between Intravenous and Intra-articular Regimens of Tranexamic Acid in Reducing Blood LossDuring Total Knee Arthroplasty. J Arthroplasty. 2014. [15] Patel JN, Spanyer JM, Smith LS, et al. Comparison of Intravenous versus Topical Tranexamic Acid in Total Knee Arthroplasty: A Prospective Randomized Study. J Arthroplasty. 2014. [16] Zhou XD, Tao LJ, Li J, et al. Do we really need tranexamic acid in total hip arthroplasty? A meta?analysis of nineteen randomized controlled trials. Arch Orthop Trauma Surg. 2013; 133(7):1017-1027. [17] Raviraj A, Anand A, Chakravarthy M, et al. Tranexamic acid reduces blood loss in simultaneous bilateral total knee arthroplasty: a randomized control trial.Eur J Orthop Surg Traumatol. 2013;22:381-386. [18] Gillette BP, DeSimone LJ, Trousdale RT,et al. Low Risk of Thromboembolic Complications With Tranexamic Acid After Primary Total Hip and Knee Arthroplasty. Clin Orthop Relat Res. 2013;471(1):150-154. [19] Alshryda S, Sarda P, Sukeik M, et al. Tranexamic acid in total knee replacement: a systematic review and meta-analysis. J Bone Joint Surg Br. 2011;93(12):1577-1585. [20] Eubanks JD. Antifibrinolytics in major orthopaedic surgery. J Am Acad Orthop Surg. 2010;18(3):132-138. [21] Yang ZG, Chen WP, Wu LD. Effectiveness and safety of tranexamic acid in reducing blood loss in total knee arthroplasty: a meta-analysis. J Bone Joint Surg Am. 2012; 94(13):1153-1159. [22] Roy SP, Tanki UF, Dutta A,et al. Efficacy of intra-articular tranexamic acid in blood loss reduction following primary unilateral totaI knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;20(12):2494-2501. [23] Sa-Ngasoongsong P, Channoom T, Kawinwonggowit V, et al. Postoperative blood loss reduction in computer-assisted surgery total knee replacement by low dose intra-articular tranexamic acid injection together with 2-hour clamp drain:a prospective triple-blinded randomized controlled trial. Orthop Rev (Pavia). 2011;3(2):e12. [24] Mutsuzaki H, Ikeda K.Intra-articular injection of tranexamic acid via drain plus drain-clamping to reduce blood loss in cementless total knee arthroplasty. J Orthop Surg Res. 2012; 29;7:32. [25] 高福强,李子剑,张克,等.人工关节置换术后隐性失血计算方法的初步探析[J].中华外科杂志,2011,49(12):1144-1145. [26] Bong MR, Patel V, Chang E, et al. Risks associated with blood transfusion after total keen arthroplasty. J Arthroplasty. 2004,19(3):281-287. [27] 孙伟,李子荣.人工关节置换术围手术期的血液管理[J].中华外科杂志,2004,42(4):244-247. [28] Spahn DR, Casutt M. Eliminating blood transfusions: new aspects and perspective Anesthesiology. 2000;93(1): 242-255. [29] Etchason J, Petz L, Keeler E, et al. The cost effectiveness of preoperative autologous blood donations. N Engl J Med. 1995; 332(11):719-724. [30] Rama KR, Apsingi S, Poovali S, et al. Timing of tourniquet releasc in knee arthmplasty.Meta-analysis of randomized,controlled trials. J Bone Joint Surg Am. 2007;89(4):699-705. [31] Li B, Wen Y, Wu H, et al. The effect of tourniquet use on hidden blood loss in total knee arthroplasty. Int Orthop. 2009; 33(5):1263-1268. [32] Ishida K, Tsumura N, Kitagawa A, et al. Intra-articular injection of tranexamic acid reduces not only blood loss but also knee joint swelling after total knee arthroplasty. Int Orthop. 2011; 35(11):1639-1645. [33] Craik JD, Ei Shafie SA, Kidd AG,et al. Can local administration of tranexamic acid during total knee arthroplasty reduce blood loss and transfusion requirements in the absence of surgical drains? Eur J Orthop Surg Traumatol. 2014;24(3):379-384. [34] Seo JG, Moon YW, Park SH, et al. The comparative efficacies of intra-articular and IV tranexamic acid for reducing blood loss during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2013;21(8):1869-1874. [35] Alshryda S, Mason J, Vaghela M, et al. Topical (intra-articular) tranexamic acid reduces blood loss and transfusion rates following total kneereplacement: a randomized controlled trial (TRANX-K). J Bone Joint Surg Am. 2013;95(21):1961-1968. [36] Kim TK, Chang CB, Koh IJ. Practical issues for the use of tranexamic acid in total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2013. [37] Wong J, Abrishami A, El Beheiry H, et al. Topical application of tranexamic acid reduces postoperative blood loss in total knee arthroplasty: a randomized, controlled trial. J Bone Joint Surg Am. 2010;92(15):2503-2513. [38] 马云青,张轶超,张洪.氨甲环酸在单侧全膝关节置换术中局部应用的止血效果分析[J].中华外科杂志, 2013, 51(1): 40-43. [39] Sa-ngasoongsong P, Wongsak S, Chanplakorn P, et al. Efficacy of low-dose intra-articular tranexamic acid in total knee replacement; a prospective triple-blinded randomized controlled trial.BMC Musculoskelet Disord. 2013;14(1): 340. [40] MacDessi S, Chen D. Dose-Dependent Effects of Intra-Articular Injection of Tranexamic Acid on Bleeding in Total Knee Arthroplasty. Bone Joint J Orthop Proceeding. 2013;95(Supp 15): 34-34. |
| [1] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [2] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [3] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [4] | Yuan Jun, Yang Jiafu. Hemostatic effect of topical tranexamic acid infiltration in cementless total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 873-877. |
| [5] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Intravenous, topical tranexamic acid alone or their combination in total knee arthroplasty: a meta-analysis of randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 948-956. |
| [6] | Zhan Fangbiao, Cheng Jun, Zou Xinsen, Long Jie, Xie Lizhong, Deng Qianrong. Intraoperative intravenous application of tranexamic acid reduces perioperative bleeding in multilevel posterior spinal surgery: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 977-984. |
| [7] | Lü Zexiang, Wu Jutai, Jiang Jian, Feng Xiao, Li Tengfei, Wang Yehua. Effect of tranexamic acid combined with carbazochrome sodium sulfonate on blood loss and safety after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 386-390. |
| [8] | Wang Hao, Wang Yitao, Lü Zexiang, Li Tengfei, Wang Shaolong, Wang Yehua. Effect of repeated intravenous tranexamic acid in the perioperative period of proximal femoral nail antirotation for femoral intertrochanteric fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3319-3323. |
| [9] | Liu Jinlei, Yin Li, Zhang Yi, Wang Haitao, Li Zhuangyan, Xia Peige, Qiao Renqiu. Effects of intravenous tranexamic acid combined with periarticular multipoint injection of tranexamic acid cocktail on blood loss and pain after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2833-2839. |
| [10] | Chen Wang, Feng Shuo, Zhang Yu, Chen Xiangyang. Efficacy and safety of tranexamic acid and epsilon-aminocaproic acid in reducing perioperative blood loss during total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(15): 2430-2436. |
| [11] | Gao Fenghe, Chen Tongying, Lin Jiebin, Liang Zujian. Efficacy and safety of tranexamic acid combined with rivaroxaban in primary total knee and hip arthroplasties: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(15): 2453-2460. |
| [12] | Ma Zhen, Liang Da, Wu Xiaolin, Zhong Wei . Safety evaluation of tranexamic acid in reducing perioperative blood loss in high tibial osteotomy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1847-1852. |
| [13] | Zheng Zhihui, Chen Sheng, Guan Keli, Zheng Xun, Chen Haibo, Zeng Qingqiang. Relationship between blood loss of proximal femoral nail anti-rotation fixation and local use combined with intravenous injection of tranexamic acid [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(9): 1359-1364. |
| [14] | Deng Zengfa, He Zhiyong, Liu Kang, Yu Xinping, Liang Jianji, Wang Jinjun, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous combined with topical administration of tranexamic acid on unicompartmental knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(36): 5793-5799. |
| [15] | Zhou Zhi, Xiong Yaqiong. Application of perioperative pulse irrigation combined with tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(36): 5806-5811. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||