Chinese Journal of Tissue Engineering Research ›› 2021, Vol. 25 ›› Issue (12): 1951-1958.doi: 10.3969/j.issn.2095-4344.3780
Previous Articles Next Articles
Dexmedetomidine combined with local anesthetic for brachial plexus block: a systematic review and meta-analysis
Wang Shao1, Yuan Dajiang2, Li Yanyan1, Li Xiaoya1
- 1Department of Anesthesiology, Shanxi Medical University, Taiyuan 030000, Shanxi Province, China; 2Department of Critical Medicine, Second Hospital of Shanxi Medical University, Taiyuan 030000, Shanxi Province, China
-
Received:2020-05-09Revised:2020-05-12Accepted:2020-05-27Online:2021-04-28Published:2020-12-26 -
Contact:Yuan Dajiang, MD, Chief physician, Department of Critical Medicine, Second Hospital of Shanxi Medical University, Taiyuan 030000, Shanxi Province, China -
About author:Wang Shao, Master candidate, Department of Anesthesiology, Shanxi Medical University, Taiyuan 030000, Shanxi Province, China
CLC Number:
Cite this article
Wang Shao, Yuan Dajiang, Li Yanyan, Li Xiaoya. Dexmedetomidine combined with local anesthetic for brachial plexus block: a systematic review and meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1951-1958.
share this article
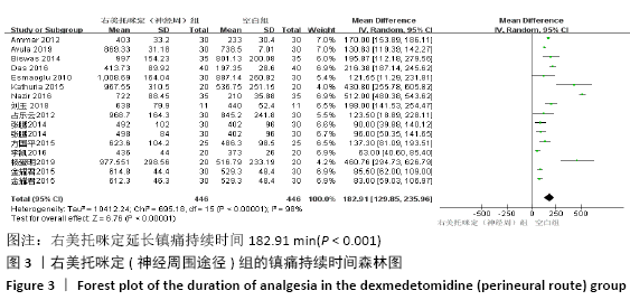
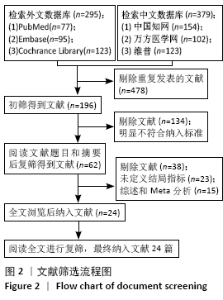
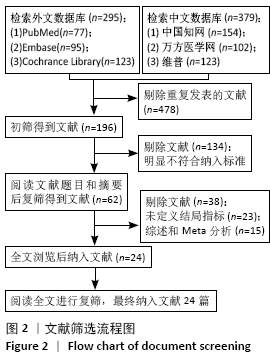
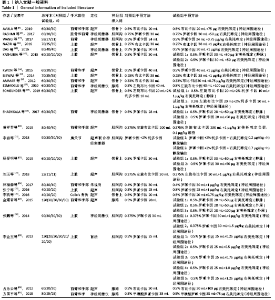
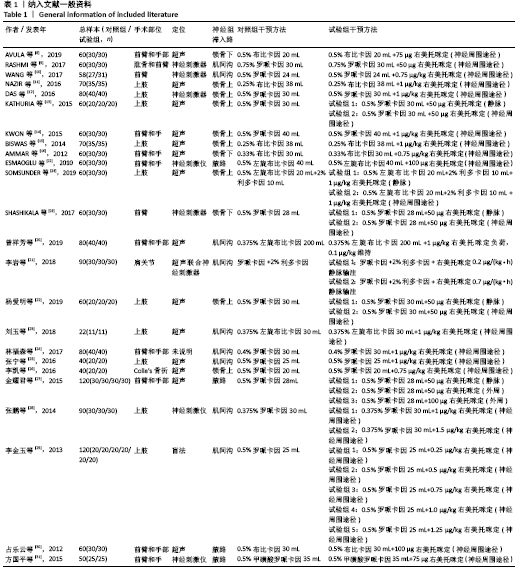
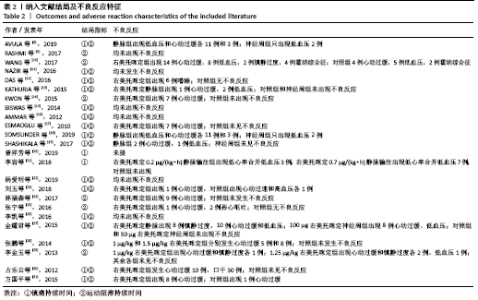
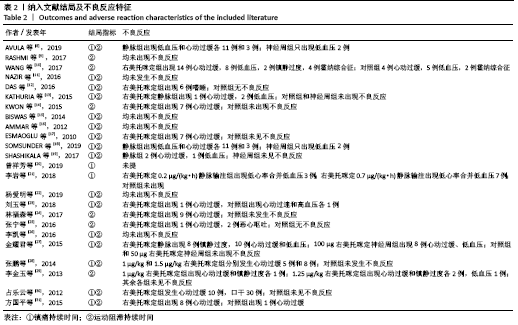
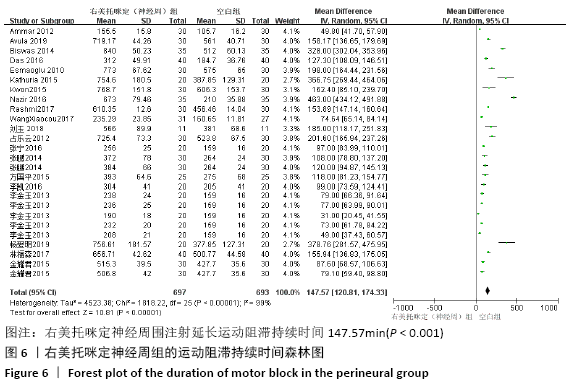
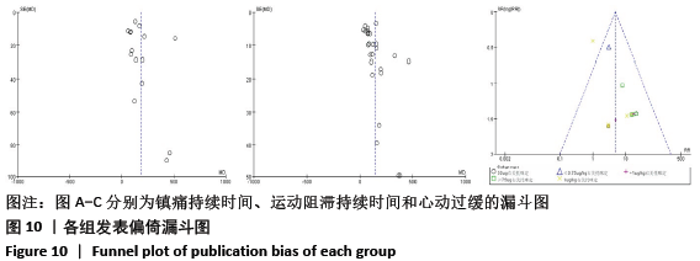
2.3 纳入文献的质量评估结果 纳入的24篇文献中5篇采用计算机随机分 组[8-10,13,15],有4篇采用密封信封随机分组[11,14,17,19],有6篇采用随机数字表法分组[20-21,24,26,29-30],有2篇由统计学专家进行分组[12,16],有1篇未提及随机方法[18],有6篇只提及随机未具体说明[22-23,25,27-28,31];有11篇未提及分配隐藏说明[14,18-20,23-25,27-28,30,31];6篇未提及盲法[18-19,23-24,27,30];所有研究结局报告数据没有缺失。所有研究均未说明是否存在其他偏倚。 2.4 Meta分析结果 2.4.1 镇痛持续时间 共18篇研究报告了镇痛持续时间[8,11-13,15-23,26-28,30-31],其中14篇比较了局部麻醉药联合右美托咪定(神经周围途径)与单独应用局部麻醉药[8,11-13,15-17,22-23,26-28,30-31],森林图结果显示,神经周围途径应用右美托咪定延长镇痛持续时间182.91 min (WMD=182.91,95%CI:129.85-235.96,P < 0.001),I2=98%,各研究间具有异质性,采用随机效应模型。采用逐篇剔除法进行敏感性分析后结果显示I2值和效应尺度无明显改变,表明研究结果稳健,见图3。 "

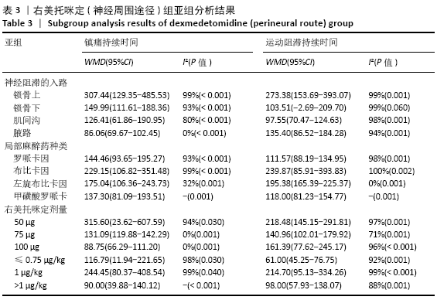
根据神经阻滞入路进行亚组分析,结果显示神经周应用右美托咪定延长镇痛持续时间在锁骨上臂丛神经阻滞最长为307.44 min(P=0.000 7),腋路臂丛神经阻滞延长86.06 min(P < 0.001),肌间沟和锁骨下臂丛神经阻滞分别为126.4 min和149.99 min(P < 0.001)。根据局部麻醉药不同进行亚组分析显示,布比卡因组镇痛持续时间延长最长为229.15 min(P=0.000 2),罗哌卡因组和左旋布比卡因组分别为144.46 min (P < 0.001)和175.04 min(P=0.23)。根据右美托咪定剂量分组,结果显示50 μg组延长镇痛持续时间最长为315.6 min(P=0.03),见表3。 "


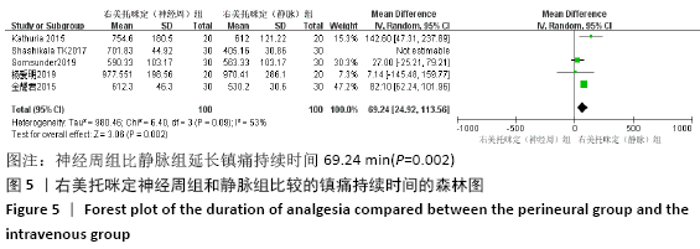
有5篇文献比较了局部麻醉药联合静脉右美托咪定与单独应用局部麻醉药的差异[13,20-22,27],I2=98%,说明各研究间存在异质性,故采用随机效应模型。结果显示静脉应用右美托咪定延长镇痛持续时间180.47 min(WMD=180.47,95%CI:83.01-277.93,I2=98%,P=0.000 3)。有5篇研究比较了神经周应用右美托咪定和静脉应用右美托咪定[13,18-19,22,27],I2=99%,各研究间存在异质性,故采用随机效应模型。进行敏感性分析后1篇文献被剔除,结果显示神经周组比静脉组延长镇痛持续时间69.24 min(WMD=69.24,95%CI:24.92-113.56,I2=53%,P=0.002),结果见图4,5。由于两组研究例数都较少,所以未进行亚组分析。 "
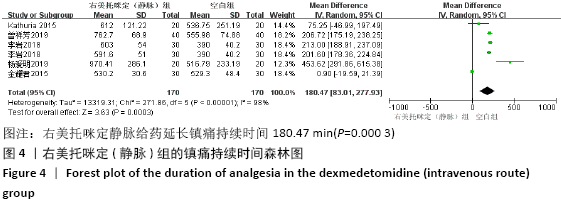
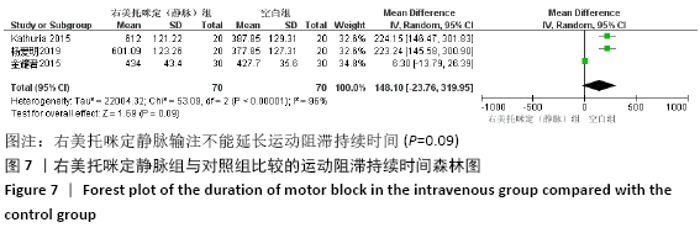
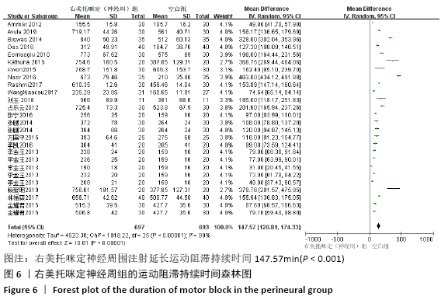
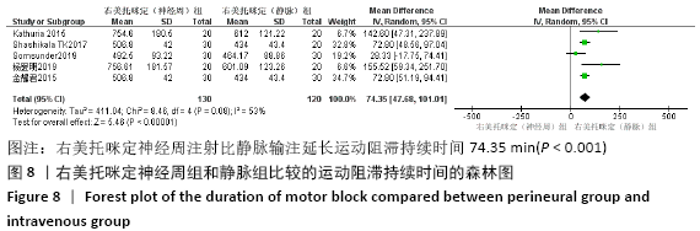
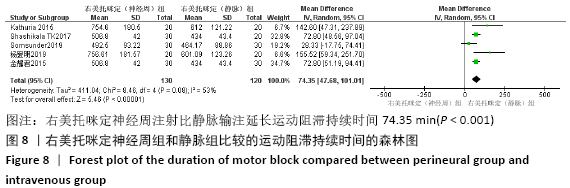
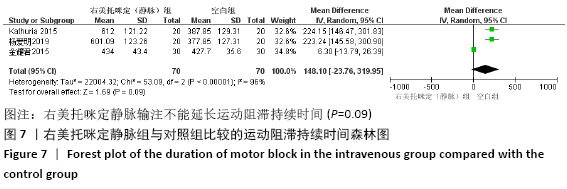
根据神经阻滞入路方式进行亚组分析显示,右美托咪定神经周组延长运动阻滞持续时间在锁骨上臂丛神经阻滞中最长为273.38 min (P < 0.001),而锁骨下臂丛神经阻滞无显著性差异(P=0.06),肌间沟和腋路臂丛神经阻滞分别为97.55 min和135.4 min(P < 0.001)。根据不同局部麻醉药进行亚组分析显示,神经周右美托咪定复合布比卡因延长运动阻滞持续时间最长(P < 0.002)。罗哌卡因组和左旋布比卡因组分别为111.57 min和195.38 min (P < 0.001)。根据右美托咪定剂量进行亚组分析结果,50 μg和1 μg/kg右美托咪定延长阻滞时间最长分别为218.48 min和214.70 min(P < 0.001),见表3。 有3篇文章比较了静脉右美托咪定联合局部麻醉药和单独应用局部麻醉药的差异[13,22,27],各研究间存在异质性(I2=96%),故采用随机效应模型。结果显示,静脉应用右美托咪定在延长运动阻滞持续时间方面没有显著性差异(P=0.09)。有5篇比较了神经周应用右美托咪定和静脉应用右美托咪定[13,18-19,22,27],各研究间存在异质性(I2=53%),故采用随机效应模型。结果显示神经周组比静脉组延长运动阻滞持续时间74.35 min(P < 0.001)。由于这2组研究例数较少,所以未进行亚组分析。见图7,8。 "

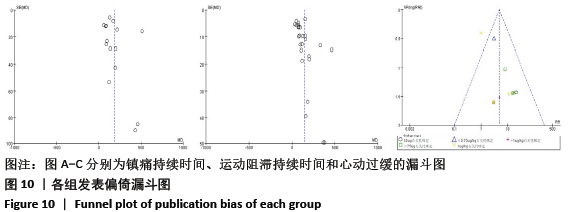
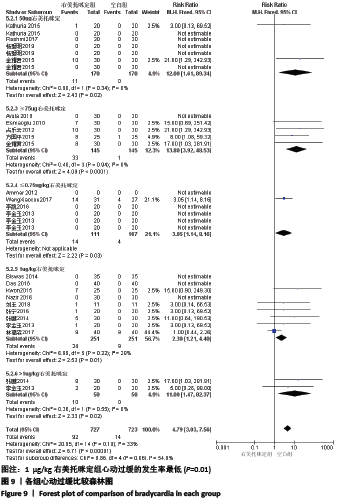
2.4.3 不良反应 24篇文献中只有1篇未报告不良反应[20],7篇文献未发生不良反应[8-9,11,15-16,22,26]。文献共报告心动过缓112例;低血压53例;镇静过度13例,口干30例,恶心呕吐2例,霍纳综合征和嗜睡各6例。文章只对报告最多的心动过缓进行了meta分析,结果显示应用右美托咪定后心动过缓的发生具有显著性差异(RR=5.08,95%CI:3.25-7.93,P < 0.001)。各研究间无明显异质性(I2=29%),采用固定效应模型。文章根据右美托咪定剂量进行亚组分析显示固定剂量中50 μg右美托咪定组心动过缓的发生率是对照组的12倍(RR=12.00,95%CI:1.61-89.34,I2=0%,P=0.02),而≥75 μg右美托咪定组是13.8倍(RR=13.80,95%CI:3.92-48.53,I2=0%,P < 0.001);按照千克体质量计算中1 μg/kg右美托咪定组心动过缓的发生率是对照组的2.3倍(RR=2.30,95%CI:1.21-4.40, I2=28%,P=0.01),其他2组分别为3.05倍(RR=3.05,95%CI:1.14-8.16,P=0.03)和11倍(RR=11.00,95%CI:1.47-82.37,I2=0%,P=0.02)。见图9。 "
| [1] BRUMMETT CM, HONG EK, JANDA AM, et al. Perineural dexmedetomidine added to ropivacaine for sciatic nerve block in rats prolongs the duration of analgesia by blocking the hyperpolarization-activated cation current. Anesthesiology. 2011; 115(4):836-843. [2] KAUR M, KAUR R, KAUR S, et al. A study to compare the analgesic efficacy of dexmedetomidine and fentanyl as adjuvants to levobupivacaine in ultrasound-guided supraclavicular brachial plexus block. Anesth Essays Res. 2018;12(3):669-673. [3] ALISTE J, LAYERA S, LAYERA S, et al. Randomized comparison between perineural dexamethasone and dexmedetomidine for ultrasound-guided infraclavicular block. Reg Anesth Pain Med. 2019. doi:10.1136/rapm-2019-100680. [4] LIU Z, JIANG M, XU T, et al. Analgesic effect of ropivacaine combined with dexmedetomidine on brachial plexus block. BMC Anesthesiol. 2018; 18(1):107. [5] KANG R, JEONG JS, YOO JC, et al. Effective dose of intravenous dexmedetomidine to prolong the analgesic duration of interscalene brachial plexus block: a single-center, prospective, double-blind, randomized controlled trial. Reg Anesth Pain Med. 2018;43(5):488-495. [6] ABDALLAH FW, BRULL R. Facilitatory effects of perineural dexmedetomidine on neuraxial and peripheral nerve block: a systematic review and meta-analysis. Br J Anaesth. 2013;110(6):915-925. [7] 代坤吾,莫均,王念念.右美托咪定复合局部麻醉药在臂丛神经阻滞中疗效的Meta分析[J].中国疼痛医学杂志,2019,25(11):837-843. [8] AVULA RR, VEMURI NN, PUTHI S, et al. Ultrasound-guided subclavian perivascular brachial plexus block using 0.5% bupivacaine with dexmedetomidine as an adjuvant: a prospective randomized controlled trial. Anesth Essays Res. 2019;13(4):615-619. [9] RASHMI HD, KOMALA HK. Effect of dexmedetomidine as an adjuvant to 0.75% ropivacaine in interscalene brachial plexus block using nerve stimulator: a prospective, randomized double-blind study.Anesth Essays Res. 2017;11(1):134-139. [10] WANG X, YU F, LI K. Which is the better adjuvant to ropivacaine in brachial plexus block: Dexmedetomidine or morphine? A prospective, randomized, double-blinded, comparative study (Article). Int J Clin Exp Med. 2017;10(7): 10813-10819. [11] NAZIR N, JAIN S. A randomized controlled trial study on the effect of adding dexmedetomidine to bupivacaine in supraclavicular block using ultrasound guidance. Ethiop J Health Sci. 2016;26(6):561-566. [12] DAS B, LAKSHMEGOWDA M, SHARMA M, et al. Supraclavicular brachial plexus block using ropivacaine alone or combined with dexmedetomidine for upper limb surgery: a prospective, randomized, double-blinded, comparative study. Rev Esp Anestesiol Reanim. 2016;63(3):135-140. [13] KATHURIA S, GUPTA S, DHAWAN I. Dexmedetomidine as an adjuvant to ropivacaine in supraclavicular brachial plexus block. Saudi J Anaesth. 2015;9(2):148-154. [14] KWON Y, HWANG SM, LEE JJ, et al. The effect of dexmedetomidine as an adjuvant to ropivacaine on the bispectral index for supraclavicular brachial plexus block. Korean J Anesthesiol. 2015;68(1):32-36. [15] BISWAS S, DAS RK, MUKHERJEE G, et al. Dexmedetomidine an adjuvant to levobupivacaine in supraclavicular brachial plexus block: a randomized double blind prospective study. Ethiop J Health Sci. 2014;24(3):203-208. [16] AMMAR AS, MAHMOUD KM. Ultrasound-guided single injection infraclavicular brachial plexus block using bupivacaine alone or combined with dexmedetomidine for pain control in upper limb surgery: a prospective randomized controlled trial. Saudi J Anaesth. 2012;6(2):109-114. [17] ESMAOGLU A, YEGENOGLU F, AKINET A, et al. Dexmedetomidine added to levobupivacaine prolongs axillary brachial plexus block. Anesth Analg. 2010;111(6):1548-1551. [18] SOMSUNDER RG, ARCHANA NB, SHIVKUMAR G, et al, Comparing efficacy of perineural dexmedetomidine with intravenous dexmedetomidine as adjuvant to levobupivacaine in supraclavicular brachial plexus block. Anesth Essays Res. 2019;13(3):441-445. [19] SHASHIKALA TK, AND K. MADHYASTHA. A prospective randomized double blinded study to evaluate the efficacy of dexmedetomidine 50 μg intravenously and perineurally as an adjunct to 0.5% ropivacaine for supraclavicular brachial plexus block. Anaesth Crit Care Pain Med. 2017;21(4):413-419. [20] 曾祥芳,肖合元.盐酸右美托咪定应用于超声引导下臂丛神经阻滞的镇痛效果分析[J]. 系统医学,2019,4(12):30-32. [21] 李岩,王辉,邓莹,等.静脉输注右美托咪定对臂丛阻滞效果的随机对照研究[J]. 北京大学学报(医学版),2018,50(5):845-849. [22] 杨爱明,王祥.右美托咪定复合罗哌卡因治疗锁骨上臂丛神经阻滞的效果观察[J]. 医药前沿, 2019,9(22):151-153. [23] 刘玉,刘绍正,王先锋.右美托咪定或舒芬太尼复合左旋布比卡因用于臂丛神经阻滞的效果观察[J].宁夏医科大学学报,2018,40(1):59-61. [24] 林福森,廖锡强,卢贵明,等.罗哌卡因复合右美托咪定应用于臂丛神经阻滞的效果分析[J].内蒙古医学杂志,2017,49(6):645-648. [25] 张宁,孙保民,程燕,等.地塞米松复合右美托咪定对臂丛神经阻滞效果的影响[J].河北医科大学学报,2016,37(8):935-939. [26] 李凯,赵国庆,李旭阳,等.右美托咪定与肾上腺素作为局部麻醉药佐剂对臂丛神经阻滞效果的对比[J].国际麻醉学与复苏杂志,2016,37(8):692-695. [27] 金耀君,赵璇.罗哌卡因复合右美托咪定对超声引导下腋路臂丛神经阻滞麻醉的影响[J].上海医学,2015,38(2):110-114. [28] 张鹏,刘婷,陈俊,等.Narcotrend监测下右美托咪定复合罗哌卡因用于臂丛阻滞麻醉的观察[J].安徽医学,2014,35(4):446-449. [29] 李金玉,葛东建,祁宾,等.不同剂量右美托咪定混合罗哌卡因用于臂丛神经阻滞的效果[J].中华麻醉学杂志,2013,33(6):711-713. [30] 占乐云,周密.右美托咪定对左布比卡因腋路臂丛神经阻滞效果的影响[J]. 中国医师进修杂志,2012,35(24):57-59. [31] 方国平,王华,张兆平,等,右美托咪定增强甲磺酸罗哌卡因臂丛神经阻滞效果的临床观察[J].医学理论与实践,2015,28(12):1568-1570. [32] ABDALLAH FW, DWYER T, CHAN VW, et al. IV and perineural dexmedetomidine similarly prolong the duration of analgesia after interscalene brachial plexus block. Anesthesiology. 2016;124(3):683-695. [33] CHEN BS, PENG H, WU SN. Dexmedetomidine, an α 2 -adrenergic agonist, inhibits neuronal delayed-rectifier potassium current and sodium current. Br J Anaesth. 2009;103(2):244-254. [34] TALKE P, LOBO E, BROWN R. Systemically administered alpha2-agonist-induced peripheral vasoconstriction in humans. Anesthesiology. 2003;99(1):65-70. [35] 马波,刘志恒,王显春.右美托咪定镇痛的临床应用进展[J].临床麻醉学杂志,2018,34(11): 1136-1139. [36] 张安生,曾宾,王剑鸣,等.锁骨上臂丛神经阻滞时不同进针方向对起效平面的影响[J] 医学临床研究,2007,24(1):67-68,71. [37] GUPTA K, TIWARI V, GUPTA PK, et al. Prolongation of subarachnoid block by intravenous dexmedetomidine for sub umbilical surgical procedures: a prospective control study. Anesth Essays Res. 2014;8(2):175-178. [38] EBERT TJ, HALL JE, BARNEY JA, et al. The effects of increasing plasma concentrations of dexmedetomidine in humans. Anesthesiology. 2000;93(2):382-394. [39] GERLACH AT, DASTA JF. Dexmedetomidine: An Updated Review. Ann Pharmacother. 2007;41(2):530-531. [40] GERTLER R, BROWN HC, MITCHELL DH, et al. Dexmedetomidine: a novel sedative-analgesic agent. Proc (Bayl Univ Med Cent). 2001;14(1):13-21. |
| [1] | Hu Kai, Qiao Xiaohong, Zhang Yonghong, Wang Dong, Qin Sihe. Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1465-1470. |
| [2] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [3] | Liang Yan, Zhao Yongfei, Xu Shuai, Zhu Zhenqi, Wang Kaifeng, Liu Haiying, Mao Keya. Imaging evaluation of short-segment fixation and fusion for degenerative lumbar scoliosis assisted by highly selective nerve root block [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1423-1427. |
| [4] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [5] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [6] | Wang Yongsheng, Wu Yang, Li Yanchun. Effect of acute high-intensity exercise on appetite hormones in adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1305-1312. |
| [7] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [8] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [9] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Intravenous, topical tranexamic acid alone or their combination in total knee arthroplasty: a meta-analysis of randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 948-956. |
| [10] | Li Yan, Wang Pei, Deng Donghuan, Yan Wei, Li Lei, Jiang Hongjiang. Electroacupuncture for pain control after total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 957-963. |
| [11] | He Xiangzhong, Chen Haiyun, Liu Jun, Lü Yang, Pan Jianke, Yang Wenbin, He Jingwen, Huang Junhan. Platelet-rich plasma combined with microfracture versus microfracture in the treatment of knee cartilage lesions: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 964-969. |
| [12] | Hua Haotian, Zhao Wenyu, Zhang Lei, Bai Wenbo, Wang Xinwei. Meta-analysis of clinical efficacy and safety of antibiotic artificial bone in the treatment of chronic osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 970-976. |
| [13] | Zhan Fangbiao, Cheng Jun, Zou Xinsen, Long Jie, Xie Lizhong, Deng Qianrong. Intraoperative intravenous application of tranexamic acid reduces perioperative bleeding in multilevel posterior spinal surgery: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 977-984. |
| [14] | Zhang Nianjun, Chen Ru. Analgesic effect of cocktail therapy combined with femoral nerve block on total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 866-872. |
| [15] | Zhong Yuanming, Wan Tong, Zhong Xifeng, Wu Zhuotan, He Bingkun, Wu Sixian. Meta-analysis of the efficacy and safety of percutaneous curved vertebroplasty and unilateral pedicle approach percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 456-462. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||