[1] 赵泽华,刘晓琳,范建高.重视非酒精性脂肪性肝病自然史的研究[J].中华肝脏病杂志,2017,25(2):81-84.
[2] WU WKK, ZHANG L, CHAN MTV. Autophagy, NAFLD and NAFLD-Related HCC. Adv Exp Med Biol.2018;1061:127-138.
[3] NAKAHIRA K, CLOONAN SM, MIZUMURA K,et al.Autophagy: a crucial moderator of redox balance, inflammation, and apoptosis in lung disease.Antioxid Redox Signal.2014;20(3): 474-494.
[4] KO GJ, BAE SY, HONG YA, et al.Radiocontrast-induced nephropathy is attenuated by autophagy through regulation of apoptosis and inflammation.Hum ExpToxicol.2016;35(7): 724-736.
[5] BUYUKLU M, KANDEMIR FM, OZKARACA M, et al. Protective effect of curcumin against contrast induced nephropathy in rat kidney: what is happening to oxidative stress, inflammation, autophagy and apoptosis? Eur Rev Med Pharmacol Sci.2014;18(4):461-470.
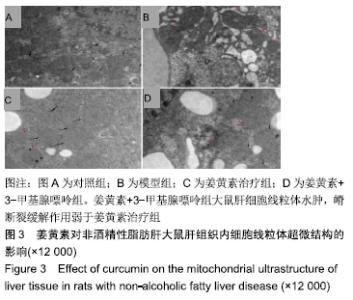
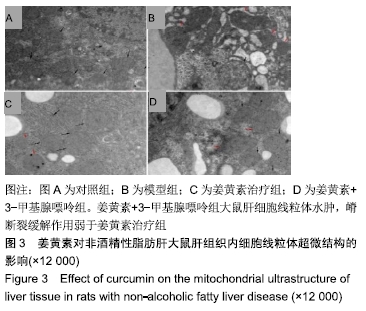
[6] WANG L, LV Y, YAO H, et al. Curcumin prevents the non-alcoholic fattyhepatitis via mitochondria protection and apoptosis reduction.Int J Clin Exp Pathol.2015;;8(9): 11503-11509.
[7] WHITE CM, LEE JY.The impact of turmeric or its curcumin extract on nonalcoholic fatty liver disease: a systematic review of clinical trials. PharmPract (Granada).2019;17(1): 135
[8] FENG W, WANG H, ZHANG P, et al.Modulation of gut microbiota contributes to curcumin-mediated attenuation of hepatic steatosis in rats. Biochim Biophys Acta Gen Subj. 2017;1861(7):1801-1812.
[9] LI C, LI J, CHEN Y, et al.Effect of curcumin on visfatin and zinc-α2-glycoprotein in a rat model of non-alcoholic fatty liver disease. Acta Cir Bras.2016;31(11):706-713.
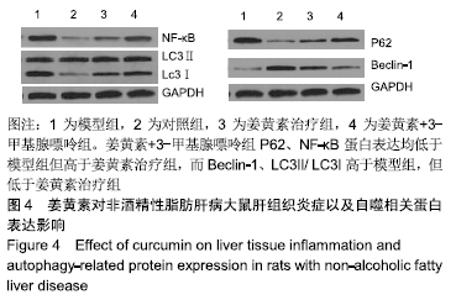
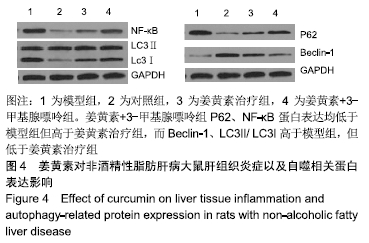
[10] SUN SC.The non-canonical NF-κB pathway in immunity and inflammation.Nat Rev Immunol. 2017;17(9):545-558.
[11] CHEN Z, LIU F, ZHENG N, et al.Wuzhi capsule (Schisandra Sphenanthera extract) attenuates liver steatosis and inflammation during non-alcoholic fatty liver disease development.Biomed Pharmacother. 2019,110:285-293.
[12] SUN B, JIA Y, HONG J, et al. Sodium Butyrate Ameliorates High-Fat-Diet-Induced Non-alcoholic Fatty Liver Disease through Peroxisome Proliferator-Activated Receptor α-Mediated Activation of β Oxidation and Suppression of Inflammation.J Agric Food Chem.2018;66(29):7633-7642.
[13] LI M, XU C, SHI J, et al.Fatty acids promote fatty liver disease via the dysregulation of 3-mercaptopyruvate sulfurtransferase/ hydrogen sulfide pathway.Gut.2018;67(12):2169-2180.
[14] KANG HH, KIM IK, LEE HI, et al.Chronic intermittent hypoxia induces liver fibrosis in mice with diet-induced obesity via TLR4/MyD88/MAPK/NF-kB signaling pathways.Biochem Biophys Res Commun. 2017;490(2):349-355.
[15] OU R, LIU J, LV M, et al.Neutrophil depletion improves diet-induced non-alcoholic fatty liver disease in mice. Endocrine.2017;57(1):72-82.
[16] WANG Y, TANG Q, DUAN P. Curcumin as a therapeutic agent for blocking NF-κB activation in ulcerative colitis. Immunopharmacol Immunotoxicol.2018;15:1-7.
[17] HE H, LUO Y, QIAO Y, et al. Curcumin attenuates doxorubicin-induced cardiotoxicity via suppressing oxidative stress and preventing mitochondrial dysfunction mediated by 14-3-3γ. Food Funct.2018;9(8):4404-4418.
[18] SAMUHASANEETO S, THONG-NGAM D, KULAPUTANA O, et al. Curcumin decreased oxidative stress, inhibited NF-kappaB activation, and improved liver pathology in ethanol-induced liver injury in rats.J Biomed Biotechnol.2009;2009:981963.
[19] 夏亮,刘江伟,沈才福,等.姜黄素预处理通过保护线粒体和抗氧化应激减轻干热环境热射病大鼠肝损伤[J].现代生物医学进展, 2017,17(18):3434-3437.
[20] ZHU L, HAN MB, GAO Y, et al.Curcumin triggers apoptosis via upregulation of Bax/Bcl-2 ratio and caspase activation in SW872 human adipocytes.Mol Med Rep.2015;12(1): 1151-1156.
[21] CHANG CH, CHEN HX, YÜ G, et al. Curcumin-Protected PC12 Cells against Glutamate-Induced Oxidative Toxicity. Food Technol Biotechnol.2014;52(4):468-478.
[22] VESKOVIC M, MLADENOVIC D, MILENKOVIC M, et al. Betaine modulates oxidative stress, inflammation,apoptosis, autophagy, and Akt/mTOR signaling in methionine- cholinedeficiency-induced fatty liver disease.Eur J Pharmacol. 2019;848:39-48.
[23] JI G, WANG Y, DENG Y, et al. Resveratrol ameliorates hepatic steatosis and inflammation in methionine/choline-deficient diet-induced steatohepatitis through regulating autophagy. Lipids Health Dis. 2015;14:134.
[24] CHU Q, ZHANG S, CHEN M, et al. Cherry Anthocyanins Regulate NAFLD by Promoting Autophagy Pathway. Oxid Med Cell Longev.2019;2019:4825949.
[25] TONG L, WANG L, YAO S, et al. PPARδ attenuates hepatic steatosis through autophagy-mediated fatty acid oxidation. Cell Death Dis.2019;10(3):197.
[26] ZHANG L, YAO Z, JI G.Herbal Extracts and Natural Products in Alleviating Non-alcoholic Fatty Liver Disease via Activating Autophagy.Front Pharmacol.2018;9:1459.
[27] NITURE S,GYAMFI MA, KEDIR H, et al.Serotonin induced hepatic steatosis is associated with modulation of autophagy and notch signaling pathway.Cell Commun Signal. 2018; 16(1):78.
[28] KIM H, DUSABIMANA T, KIM SR, et al.Supplementation of Abelmoschus manihot Ameliorates Diabetic Nephropathy andHepatic Steatosis by Activating Autophagy in Mice. Nutrients.2018;10(11). pii: E1703.
|