| [1] Wild S, Roglic G, Green A, et al. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care.2004;27(5):1047-1053.
[2] Suszynski TM, Avgoustiniatos ES, Papas KK. Intraportal islet oxygenation. J Diabetes Sci Technol. 2014;8(3):575-580.
[3] Cantley J, Walters SN, Jung MH, et al. A preexistent hypoxic gene signature predicts impaired islet graft function and glucose homeostasis. Cell Transplant. 2013;22(11):2147-2159.
[4] Deng S, Markmann JF, Rickels M,et al. Islet alone versus islet after kidney transplantation: metabolic outcomes and islet graft survival. Transplantation. 2009;88(6):820-825.
[5] Menger MD, Jaeger S, Walter P, et al. Angiogenesis and hemodynamics of microvasculature of transplanted islets of Langerhans. Diabetes. 1989;38 Suppl 1:199-201.
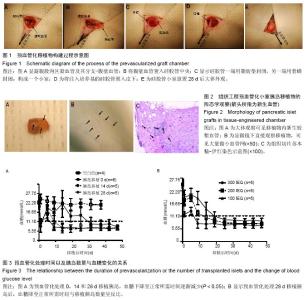
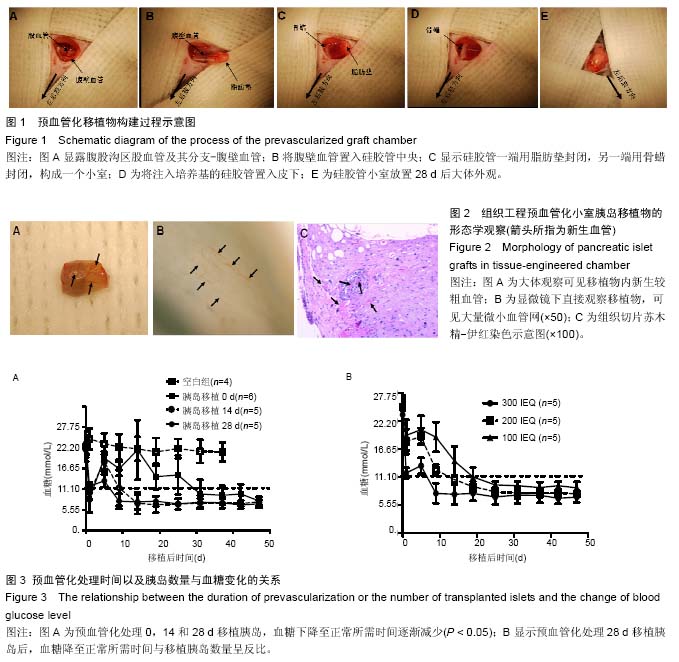
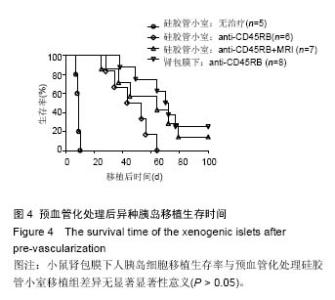
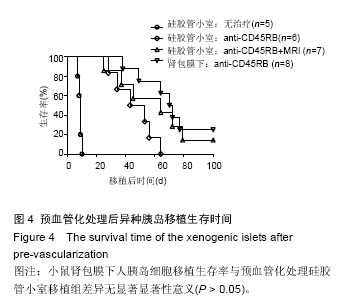
[6] Hussey AJ, Winardi M, Han XL, et al. Seeding of pancreatic islets into prevascularized tissue engineering chambers. Tissue Eng Part A. 2009; 15(12): 3823-3833.
[7] Cronin KJ, Messina A, Knight KR, et al. New murine model of spontaneous autologous tissue engineering, combining an arteriovenous pedicle with matrix materials. Plast Reconstr Surg.2004;113(1):260-269.
[8] Kin T, Korbutt GS, Rajotte RV. Survival and metabolic function of syngeneic rat islet grafts transplanted in the omental pouch. Am J Transplant. 2003;3(3):281-285.
[9] Gustavson SM, Rajotte RV, Hunkeler D, et al. Islet auto-transplantation into an omental or splenic site results in a normal beta cell but abnormal alpha cell response to mild non-insulin-induced hypoglycemia. Am J Transplant. 2005;5(10):2368-2377.
[10] Aoki T, Hui H, Umehara Y,et al.Intrasplenic transplantation of encapsulated genetically engineered mouse insulinoma cells reverses streptozotocin- induced diabetes in rats. Cell Transplant. 2005;14(6): 411-421.
[11] Caiazzo R, Gmyr V, Hubert T, et al. Evaluation of alternative sites for islet transplantation in the minipig: interest and limits of the gastric submucosa. Transplant Proc. 2007;39(8):2620-2623.
[12] Dufour JM, Rajotte RV, Zimmerman M, et al. Development of an ectopic site for islet transplantation, using biodegradable scaffolds. Tissue Eng. 2005; 11(9-10):1323-1331.
[13] Weber CJ, Hardy MA, Pi-Sunyer F, et al. Tissue culture preservation and intramuscular transplantation of pancreatic islets. Surgery. 1978;84(1): 166-174.
[14] Rafael E, Tibell A, Rydén M, et al. Intramuscular autotransplantation of pancreatic islets in a 7-year-old child: a 2-year follow-up. Am J Transplant. 2008;8(2): 458-462.
[15] Speier S, Nyqvist D, Cabrera O, et al.Noninvasive in vivo imaging of pancreatic islet cell biology. Nat Med. 2008;14(5):574-578.
[16] Zhao G, Moore DJ, Kim JI, et al. An immunosufficient murine model for the study of human islets. Xenotransplantation 2014; 21(6): 567-573. |