Chinese Journal of Tissue Engineering Research ›› 2015, Vol. 19 ›› Issue (21): 3302-3308.doi: 10.3969/j.issn.2095-4344.2015.21.005
Previous Articles Next Articles
Collagen sponge as an artificial dura mater combined with ozone to repair brain injury
Qu Hong, Zhao Ming-guang, Liang Ying, Zhao Li-ping, Li Xiao-hong, Wang Ying
- Department of Neurology, General Hospital of Shenyang Military Region, Shenyang 110016, Liaoning Province, China
-
Online:2015-05-21Published:2015-05-21 -
Contact:Corresponding author: Zhao Guang-ming, M.D., Associate chief physician, Department of Neurology, General Hospital of Shenyang Military Region, Shenyang 110016, Liaoning Province, China -
About author:Qu Hong, Master, Department of Neurology, General Hospital of Shenyang Military Region, Shenyang 110016, Liaoning Province, China -
Supported by:Liaoning Science and Technology Project, No. 2012225019
CLC Number:
Cite this article
Qu Hong, Zhao Ming-guang, Liang Ying, Zhao Li-ping, Li Xiao-hong, Wang Ying. Collagen sponge as an artificial dura mater combined with ozone to repair brain injury[J]. Chinese Journal of Tissue Engineering Research, 2015, 19(21): 3302-3308.
share this article

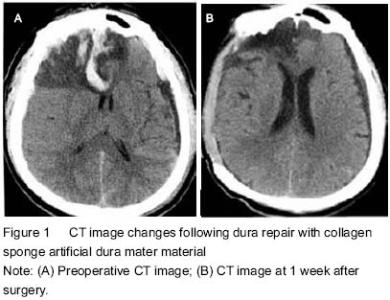
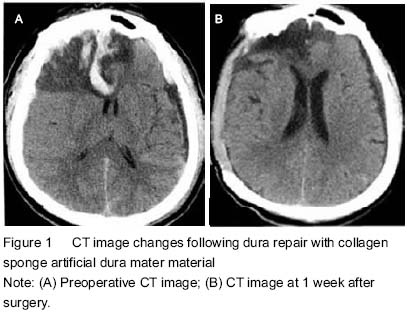
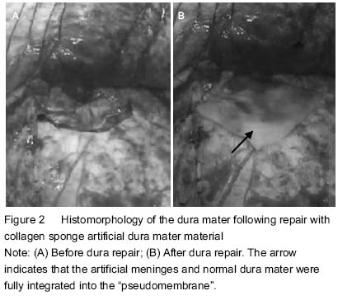
Quantitative analysis of participants Two cases died of severe brain injury after diffuse brain swelling, one died of brain injury with multiple organ failure, and two cases of extensive brain injury accompanied by cerebral herniation were in vegetative state. Patients were followed for 1 year, and the remaining 55 patients were enrolled in the final analysis (Table 1). Meningeal repair with collagen sponge as the artificial dura mater material There were no cerebrospinal fluid leakage from the incision, subcutaneous fluid, intracranial infections, epilepsy and other complications, and skin incision healed well in all patients followed by regular removal of stitches. Before discharge, head CT examinations showed no obvious abnormalities at the repair site. Patients recovered well postoperatively with normal body temperature and normal results of blood and biochemical tests (Table 1). Of the 60 patients, 2 patients died of postoperative diffuse brain swelling, one died of brain injury with multiple organ failures, and two cases of extensive brain injury accompanied by cerebral herniation were in vegetative state after surgery. Another 55 cases showed obvious midline shift on CT images at 1, 7, 14 days after surgery (P < 0.05). There was also a significant difference in the intracranial pressure at 1, 7, 14 days after surgery (P < 0.05; Table 2), indicating the treatment achieved the purpose of decompression. "
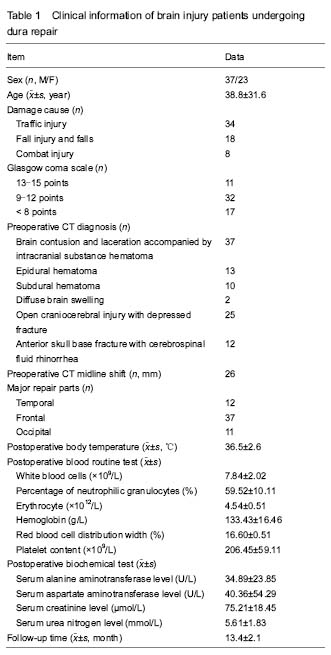
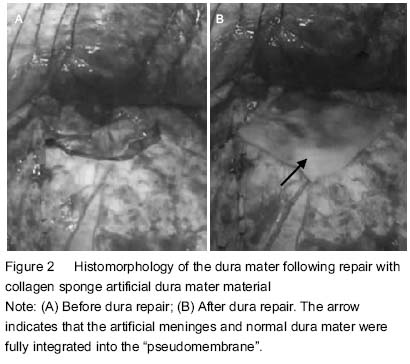
Follow-up results According to Glasgow coma scale score, complete recovery was in 12 cases (20%), mild disability in 16 cases (27%), moderate disability in 21 cases (35%), severe disability in 7 cases (12%), vegetative state in 2 cases (3%), and death in 2 cases (3%). At 3-6 months after dura repair, 28 cases were subject to skull repair, and during the skull repair, the anatomical structures of the dura mater were found basically clear and less wound bleeding. There was shorter operative time. The dura mater separated was intact with no damage to brain tissues, and the artificial meninges and normal dura mater were fully integrated into the “pseudomembrane” that had a complete smooth surface and medial surface. No meningeal adhesions and severe inflammatory reactions in the repair area were found (Figure 2)."
Observation and processing results of subcutaneous fluid After surgery, two patients appeared with postoperative subcutaneous fluid and their conditions improved following puncture aspiration and pressure dressing with elastic bandage; another patient showed a small amount of subdural effusion, but with no special treatment, and dynamic head CT showed the effusion was gradually reduced. Adverse reactions and complications During the follow-up, there was no advanced incision leakage of cerebrospinal fluid, brain incarceration and epilepsy. All skin incisions were healed at stage I, with regular removal of stitches. Repair materials had no response to the host in the blood, tissue, and immunological fields."

| [1] Tsuji M, Inoue Y, Sugaya C, et al. Higher toxicity of dibutyltin and poly-L-lactide with a large amount of tin but lower toxicity of poly-L-lactide of synthetic artificial dura mater exhibited on murine astrocyte cell line. Yakugaku Zasshi. 2010;130(6):847-855. [2] Zhang YL, Xin GH, Zeng YL. Pig peritonium as a donor transplant to repair the defect in human cerebral dura mater. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2008;12(23):4489-4492. [3] Chen J, Shi SS, Zhang GL, et al. Bio-artificial dura mater in repair of dural defects. Zhongguo Zuzhi Gongheng Yanjiu. 2013;17(51):8914-8919. [4] Esposito F, Grimod G, Cavallo LM, et al. Collagen-only biomatrix as dural substitute: What happened after a 5-year observational follow-up study. Clin Neurol Neurosurg. 2013;115(9):1735-1737. [5] Parlato C, di Nuzzo G, Luongo M, et al. Use of a collagen biomatrix (TissuDura) for dura repair: a long-term neuroradiological and neuropathological evaluation. Acta Neurochir (Wien). 2011;153(1):142-147. [6] Papakostas JC, Avgos S, Arnaoutoglou E, et al. Use of the vascu-guard bovine pericardium patch for arteriotomy closure in carotid endarterectomy. Early and long-term results. Ann Vasc Surg. 2014;28(5):1213-1218. [7] Coleman S, Kerr H, Krishnamurthi V, et al. The use of bovine pericardium for complex urologic venous reconstruction. Urology. 2014;83(2):495-497. [8] Costa BS, Cavalcanti-Mendes Gde A, Abreu MS, et al. Clinical experience with a novel bovine collagen dura mater substitute. Arq Neuropsiquiatr. 2011;69(2A):217-220. [9] Chen X, Liu J, Yang GY.The clinical application of collagen dressing. Linchuang yu Shiyan Yixue Zazhi. 2010;17(23):1078-1079. [10] Sartori C, Lepori M, Scherrer U. Interaction between nitric oxide and the cholinergic and sympathetic nervous system in cardiovascular control in humans. Pharmacol Ther. 2005;106(2):209-220. [11] Bocci V, Paulesu L. Studies on the biological effects of ozone 1. Induction of interferon gamma on human leucocytes. Haematologica. 1990;75(6):510-515. [12] Larini A, Bocci V. Effects of ozone on isolated peripheral blood mononuclear cells. Toxicol In Vitro. 2005;19(1): 55-61. [13] Zhou NB, Fu ZJ, Sun T. Effects of different concentrations of oxygen-ozone on rats' astrocytes in vitro. Neurosci Lett. 2008;441(2):178-182. [14] Parízek J, Husek Z, M?ricka P, et al. Ovine pericardium: a new material for duraplasty. J Neurosurg. 1996;84(3): 508-513. [15] Chen YG, Zhao MM, Ning TY, et al. The application of artificial dura in emergency craniocerebral surgery. Hebei Yiyao. 2010;16(6):688-689. [16] Roberts I, Sydenham E. Barbiturates for acute traumatic brain injury. Cochrane Database Syst Rev. 2012;12: CD000033. [17] Timofeev I, Carpenter KL, Nortje J, et al. Cerebral extracellular chemistry and outcome following traumatic brain injury: a microdialysis study of 223 patients. Brain. 2011;134(Pt 2):484-494. [18] Wakai A, McCabe A, Roberts I, et al. Mannitol for acute traumatic brain injury. Cochrane Database Syst Rev. 2013;8:CD001049. [19] Tong WS, Zheng P, Xu JF, et al. Early CT signs of progressive hemorrhagic injury following acute traumatic brain injury. Neuroradiology. 2011;53(5):305-309. [20] Walcott BP, Kahle KT, Simard JM. The DECRA trial and decompressive craniectomy in diffuse traumatic brain injury: is decompression really ineffective? World Neurosurg. 2013;79(1):80-81. [21] Bor-Seng-Shu E, Figueiredo EG, Fonoff ET, et al. Decompressive craniectomy and head injury: brain morphometry, ICP, cerebral hemodynamics, cerebral microvascular reactivity, and neurochemistry. Neurosurg Rev. 2013;36(3):361-370. [22] Timofeev I, Santarius T, Kolias AG, et al. Decompressive craniectomy - operative technique and perioperative care. Adv Tech Stand Neurosurg. 2012;38:115-136. [23] Wen L, Li QC, Wang SC, et al. Contralateral haematoma secondary to decompressive craniectomy performed for severe head trauma: a descriptive study of 15 cases. Brain Inj. 2013;27(3):286-292. [24] Sakas DE, Charnvises K, Borges LF, et al. Biologically inert synthetic dural substitutes. Appraisal of a medical-grade aliphatic polyurethane and a polysiloxane-carbonate block copolymer. J Neurosurg. 1990;73(6):936-941. [25] Andreula CF, Simonetti L, De Santis F, et al. Minimally invasive oxygen-ozone therapy for lumbar disk herniation. AJNR Am J Neuroradiol. 2003;24(5):996-1000. [26] Bocci V. Ozone as a bioregulator. Pharmacology and toxicology of ozonetherapy today. J Biol Regul Homeost Agents. 1996;10(2-3):31-53. [27] Leone S, Noera G, Bertolini A. Melanocortins as innovative drugs for ischemic diseases and neurodegenerative disorders: established data and perspectives. Curr Med Chem. 2013;20(6):735-750. [28] Dzieran J, Fabian J, Feng T, et al. Comparative analysis of TGF-β/Smad signaling dependent cytostasis in human hepatocellular carcinoma cell lines. PLoS One. 2013;8(8): e72252. [29] Timmermann J, Hahn M, Krueger K. Short-term follow-up: micro-invasive therapy of the cervical herniated disk by percutaneous nucleotomy. J Back Musculoskelet Rehabil. 2011;24(2):89-93. [30] Steppan J, Meaders T, Muto M, et al. A metaanalysis of the effectiveness and safety of ozone treatments for herniated lumbar discs. J Vasc Interv Radiol. 2010;21(4):534-548. [31] Zhang Y, Ma Y, Jiang J, et al. Treatment of the lumbar disc herniation with intradiscal and intraforaminal injection of oxygen-ozone. J Back Musculoskelet Rehabil. 2013;26(3):317-322. [32] Zhou JQ, Chen H, Chen ZY, et al. Effects of ozone oxidative preconditioning on apoptosis induced by renal ischemia/reperfusion injury in rats. Zhonghua Qiguan Yizhi Zazhi. 2012;33(2):113-117. [33] Xin ZG, Liu B, Gao Y, et al. Small doses of triamcinolone aacetonide for heel pain. Zhongguo Xiandai Yisheng. 2011;49(1):130-131. [34] Zeng Y, Xiong M, Yu HL, et al. Efficacy comparison of medical ozone with sodium hyaluronate in the treatment of knee osteoarthritis. Linchuang Waike Zazhi. 2010;18(8):565-567. [35] Gautam S, Rastogi V, Jain A, et al. Comparative evaluation of oxygen-ozone therapy and combined use of oxygen-ozone therapy with percutaneous intradiscal radiofrequency thermocoagulation for the treatment of lumbar disc herniation. Pain Pract. 2011;11(2):160-166. [36] Zamora ZB, Borrego A, López OY, et al. Effects of ozone oxidative preconditioning on TNF-alpha release and antioxidant-prooxidant intracellular balance in mice during endotoxic shock. Mediators Inflamm. 2005;2005(1):16-22. [37] Lehnert T, Naguib NN, Wutzler S, et al. Analysis of disk volume before and after CT-guided intradiscal and periganglionic ozone-oxygen injection for the treatment of lumbar disk herniation. J Vasc Interv Radiol. 2012;23(11): 1430-1436. [38] Torossian A, Ruehlmann S, Eberhart L, et al. Pre-treatment with ozonized oxygen (O3) aggravates inflammation in septic rats. Inflamm Res. 2004;53 Suppl 2:S122-125. |
| [1] | Shen Jinbo, Zhang Lin. Micro-injury of the Achilles tendon caused by acute exhaustive exercise in rats: ultrastructural changes and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1190-1195. |
| [2] | Liang Xueqi, Guo Lijiao, Chen Hejie, Wu Jie, Sun Yaqi, Xing Zhikun, Zou Hailiang, Chen Xueling, Wu Xiangwei. Alveolar echinococcosis protoscolices inhibits the differentiation of bone marrow mesenchymal stem cells into fibroblasts [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 996-1001. |
| [3] | Duan Liyun, Cao Xiaocang. Human placenta mesenchymal stem cells-derived extracellular vesicles regulate collagen deposition in intestinal mucosa of mice with colitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1026-1031. |
| [4] | Liu Liu, Zhou Qingzhu, Gong Zhuo, Liu Boyan, Yang Bin, Zhao Xian. Characteristics and manufacturing techniques of collagen/inorganic materials for constructing tissue-engineered bone [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 607-613. |
| [5] | Xu Xiaoming, Chen Yan, Song Qian, Yuan Lu, Gu Jiaming, Zhang Lijuan, Geng Jie, Dong Jian. Human placenta derived mesenchymal stem cell gel promotes the healing of radiation skin damage in SD rats [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3976-3980. |
| [6] | Liu Fang, Shan Zhengming, Tang Yulei, Wu Xiaomin, Tian Weiqun. Effects of hemostasis and promoting wound healing of ozone sustained-release hydrogel [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3445-3449. |
| [7] | Wang Hao, Chen Mingxue, Li Junkang, Luo Xujiang, Peng Liqing, Li Huo, Huang Bo, Tian Guangzhao, Liu Shuyun, Sui Xiang, Huang Jingxiang, Guo Quanyi, Lu Xiaobo. Decellularized porcine skin matrix for tissue-engineered meniscus scaffold [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3473-3478. |
| [8] | Chen Lei, Zheng Rui, Jie Yongsheng, Qi Hui, Sun Lei, Shu Xiong. In vitro evaluation of adipose-derived stromal vascular fraction combined with osteochondral integrated scaffold [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3487-3492. |
| [9] | Yang Li, Li Xueli, Song Jinghui, Yu Huiqian, Wang Weixia. Effect of cryptotanshinone on hypertrophic scar of rabbit ear and its related mechanism [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(20): 3150-3155. |
| [10] | Liu Zhendong, Wang Rui, Li Xiaolei, Wang Jingcheng. Review of interferon alpha-2b inhibiting scar formation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(2): 317-321. |
| [11] | Chen Siyu, Li Yannan, Xie Liying, Liu Siqi, Fan Yurong, Fang Changxing, Zhang Xin, Quan Jiayu, Zuo Lin. Thermosensitive chitosan-collagen composite hydrogel loaded with basic fibroblast growth factor retards ventricular remodeling after myocardial infarction in mice [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(16): 2472-2478. |
| [12] | Chen Liang, Meng Shu, Cheng Guoping, Ding Yi . Effects of fish scale collagen membrane on adhesion, proliferation and osteogenic differentiation of rat bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(16): 2494-2499. |
| [13] | Zhang Hui, Wang Shaohua, Wang Qian, Wang Hui, Gan Hongquan, Cui Yishuang, Li Qijia, Wang Zhiqiang. Porous tantalum coated with RGD polypeptide can activate the integrin/focal adhesion kinase signaling pathway of MG63 cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(16): 2535-2540. |
| [14] | Li Shao, Liang Yongkang, Gao Yi, Peng Qing. Establishment and functional in vitro characteristics of three-dimensional collagen HepaRG microsphere [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(16): 2541-2547. |
| [15] | Liu Yunyi, Wang Bo, Wang Lin. Effects of post-exercise gastrocnemius needling on Achilles tendon degeneration in obese rats [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(14): 2211-2218. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||