Chinese Journal of Tissue Engineering Research ›› 2013, Vol. 17 ›› Issue (23): 4216-4233.doi: 10.3969/j.issn.2095-4344.2013.23.006
Previous Articles Next Articles
Human placental mesenchymal stem cells promote angiogenesis
Zhao Ji-dong, Miao Zong-ning, Qian Han-guang, Peng Wei, Si Zhi-ping
- Department of Orthopedics (Department of Reconstructive Sciences), Wuxi Third People’s Hospital, Wuxi 214041, Jiangsu Province, China
-
Online:2013-06-04Published:2013-06-04 -
Contact:Miao Zong-ning, Ph.D., Associate chief physician, Department of Orthopedics (Department of Reconstructive Sciences), Wuxi Third People’s Hospital, Wuxi 214041, Jiangsu Province, China zongningm@yahoo.com.cn -
About author:Zhao Ji-dong, Associate chief physician, Department of Orthopedics (Department of Reconstructive Sciences), Wuxi Third People’s Hospital, Wuxi 214041, Jiangsu Province, China zid66@hotmail.com
CLC Number:
Cite this article
Zhao Ji-dong, Miao Zong-ning, Qian Han-guang, Peng Wei, Si Zhi-ping. Human placental mesenchymal stem cells promote angiogenesis[J]. Chinese Journal of Tissue Engineering Research, 2013, 17(23): 4216-4233.
share this article

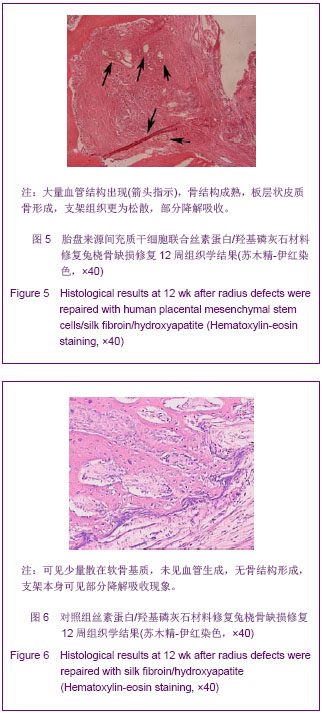
2.3 胎盘来源间充质干细胞联合丝素蛋白/羟基磷灰石材料修复兔桡骨缺损结果 实验动物大体形态观察:所有实验兔子全部进入结果分析。造模后3 d内,有轻微跛行,活动明显减少,但情况逐渐好转,10 d左右饮食和精神正常化,伤口一期愈合,无感染、渗液。 组织学检测:实验组造模后4周时支架内可见部分松散骨基质形成,骨细胞包埋其中,支架吸收降解不明显;12周时可见骨小梁排列规则,骨细胞深埋于骨基质中,大量血管结构出现,骨结构成熟,板层状皮质骨形成,支架组织更为松散,部分降解吸收,见图5。对照组造模后4周时支架内可见大量纤维性软组织充填其中,未见软骨基质及类骨质,支架无明显降解改变;12周时支架组织孔隙内可见少量散在软骨基质,无骨结构形成,支架本身可见部分降解吸收现象,见图6。 2.4 不良反应 实验组造模后2周时支架材料孔隙内有少量纤维结缔组织、血管和炎性细胞聚集,材料与骨端未有连接,4周时支架材料部分吸收。对照组造模后2周,可见少量纤维组织长入支架空隙内,未发现明显炎症细胞浸润;4周时支架材料少量吸收,所有实验动物未见明显炎症反应,材料与组织相容性良好。"
| [1]Rose FR,Oreffo RO. Bone tissue engineering: hope vs hype. Biochem Biophys Res Commun. 2002;292(1):1-7.[2]Bhumiratana S, Vunjak-Novakovic G. Concise review: personalized human bone grafts for reconstructing head and face. Stem Cells Transl Med. 2012;1(1):64-69.[3]Ogawa M, Tohma Y, Ohgushi H, et al. Early Fixation of Cobalt-Chromium Based Alloy Surgical Implants to Bone Using a Tissue-engineering Approach. Int J Mol Sci. 2012; 13(5):5528-5541.[4]Panseri S, Cunha C, D'Alessandro T et al. Magnetic hydroxyapatite bone substitutes to enhance tissue regeneration: evaluation in vitro using osteoblast-like cells and in vivo in a bone defect. PLoS One. 2012;7(6):e38710.[5]Marolt D, Campos IM, Bhumiratana S et al. Engineering bone tissue from human embryonic stem cells. Proc Natl Acad Sci U S A. 2012; 109(22):8705-8709.[6]Zhou J, Lin H, Fang T, et al. The repair of large segmental bone defects in the rabbit with vascularized tissue engineered bone. Biomaterials. 2010;31(6):1171-1179.[7]Laschke MW, Strohe A, Menger MD, et al. In vitro and in vivo evaluation of a novel nanosize hydroxyapatite particles/poly (ester-urethane) composite scaffold for bone tissue engineering. Acta Biomater. 2010;6(6):2020-2027.[8]Semenov OV, Koestenbauer S, Riegel M, et al. Multipotent mesenchymal stem cells from human placenta: critical parameters for isolation and maintenance of stemness after isolation. Am J Obstet Gynecol. 2010;202(2):193.[9]Parolini O, Alviano F, Bagnara GP, et al. Isolation and characterization of cells from human term placenta: outcome of the first international workshop on placenta derived stem cells. Stem Cells. 2008;26(1):300-311.[10]Vellasamy S, Sandrasaigaran P, Vidyadaran S, et al. Isolation and characterisation of mesenchymal stem cells derived from human placenta tissue. World J Stem Cells. 2012;4(6):53-61.[11]Zheng L, Zhang D, Chen X, et al. Antitumor activities of human placenta-derived mesenchymal stem cells expressing endostatin on ovarian cancer. PLoS One. 2012;7(7):e39119.[12]Li X, Ling W, Pennisi A et al. Human placenta-derived adherent cells prevent bone loss, stimulate bone formation, and suppress growth of multiple myeloma in bone. Stem Cells. 2011;29(2):263-273.[13]Pasquinelli G, Tazzari P, Ricci F, et al. Ultrastructural characteristics of human mesenchymal stromal (stem) cells derived from bone marrow and term placenta. Ultrastruct Pathol. 2007 ;31(1):23-31.[14]Miao Z, Jin J, Chen L, et al. Isolation of mesenchymal stem cells from human placenta: comparison with human bone marrow mesenchymal stem cells. Cell Biol Int. 2006;30(9): 681-687.[15]Qian HG, Miao ZN, Zhao JD, et al. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2010;14(51):9507-9511. 钱寒光,苗宗宁,赵基栋,等.丝素蛋白/羟基磷灰石材料复合人胎盘间充质干细胞修复桡骨节段性骨缺损[J].中国组织工程研究与临床康复,2010,14(51):9507-9511.[16]Zhang ZY, Teoh SH, Chong MS, et al. Superior osteogenic capacity for bone tissue engineering of fetal compared with perinatal and adult mesenchymal stem cells. Stem Cells. 2009;27(1):126-137.[17]Porter JR, Ruckh TT, Popat KC. Bone tissue engineering: a review in bone biomimetics and drug delivery strategies. Biotechnol Prog. 2009;25(6):1539-1560.[18]Zhong W, Sumita Y, Ohba S, et al. In vivo comparison of the bone regeneration capability of human bone marrow concentrates vs. platelet-rich plasma. PLoS One. 2012; 7(7):e40833.[19]Mandal BB, Grinberg A, Gil ES, et al. High-strength silk protein scaffolds for bone repair. Proc Natl Acad Sci U S A. 2012;109(20):7699-7704.[20]Holzwarth JM, Ma PX. Biomimetic nanofibrous scaffolds for bone tissue engineering. Biomaterials. 2011 Dec;32(36): 9622-9629.[21]Lv J, Wang PJ. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2011;15(21):3929-3933. 吕军,王培吉. 血管内皮生长因子复合人工骨材料修复骨缺损[J]. 中国组织工程研究与临床康复,2011,15(21):3929-3933.[22]Yang XM, Zhang L, Meng XY, et al. Zhongguo Xiufu Chongjian Waike Zazhi. 2011;25(6):729-735.杨新明,张磊,孟宪勇,等. 比较带蒂筋膜瓣包裹接种自体红骨髓的组织工程骨修复骨缺损时促血管化成骨与膜诱导成骨作用[J]. 中国修复重建外科杂志,2011,25(6): 729-735.[23]Duan CG. Disi Junyi Daxue. 2009.段春光.双基因修饰促进组织工程化人工骨血管化的研究[D]. 第四军医大学,2009.[24]Ru J, Li Q. Zhongguo Zuzhi Gongcheng Yanjiu. 2013;17(2): 353-357.茹嘉,李强.最新进展的转基因技术在骨与软骨缺损修复中的应用[J].中国组织工程研究,2013,17(2):353-357.[25]Li DS, Cai B, Liu JG, et al. Zhonghua Guanjie Waike Zazhi (dianziban).2012;6(4):574-580.李冬松,蔡波,刘建国,等. 血管内皮生长因子对脂肪干细胞成骨分化基因转录水平的调节[J]. 中华关节外科杂志(电子版), 2012,6(4):574-580.[26]Ferrari G,Cook BD,Terushkin V,et al.Transforming growth factor-beta 1 (TGF-beta1) induces angiogenesis through vascular endothelial growth factor (VEGF)-mediated apoptosis.J Cell Physiol,2009,219(2):449-458.[27]Sun YB, Sun HM, Li JJ, et al. Shengwu Yixue Gongcheng yu Linchuang. 2009;13(1):76-80.孙仰白,孙洪邈,李建军,等. 流体切应力促进组织工程骨成骨和血管化的研究进展[J].生物医学工程与临床,2009,13(1):76-80.[28]Polykandriotis E, Horch RE, Arkudas A, et al.Intrinsic versus extrinsic vascularization in tissue engineering. Advances in experimental medicine and biology.2006;585:311-326.[29]Chamberlain G, Fox J, Ashton B, et al. Concise review: Mesenchymal stem cells: Their phenotype, differentiation capacity, immunological features, and potential for homing. Stem Cells. 2007;25:2739-2749.[30]Aghajanova L, Horcajadas JA, Esteban FJ, et al. The bone marrow-derived human mesenchymal stem cell: potential progenitor of the endometrial stromal fibroblast. Biol Reprod. 2010;82(6):1076-1087.[31]Peichev M, Naiyer AJ, Pereira D, et al. Expression of VEGFR-2 and AC133 by circulating human CD34(+) cells identifies a population of functional endothelial precursors. Blood. 2000 ;95(3):952-958.[32]Hristov M, Erl W, Weber PC. Endothelial progenitor cells: Mobilization, differentiation, and homing. Arterioscler Thromb Vasc Biol. 2003;23(7):1185-1189.[33]Gehling UM, Ergün S, Schumacher U, et al. In vitro differentiation of endothelial cells from AC133-positive progenitor cells. Blood. 2000;95(10):3106-3112.[34]Kim CH, Lee JH, Won JH, et al. Mesenchymal Stem Cells Improve Wound Healing In Vivo via Early Activation of Matrix Metalloproteinase-9 and Vascular Endothelial Growth Factor. J Korean Med Sci. 2011;26(6):726-733.[35]Pilz GA, Ulrich C, Ruh M, et al. Human term placenta-derived mesenchymal stromal cells are less prone to osteogenic differentiation than bone marrow-derived mesenchymal stromal cells. Stem Cells Dev. 2011 ;20(4):635-646.[36]Shafiee A, Seyedjafari E, Soleimani M, et al. A comparison between osteogenic differentiation of human unrestricted somatic stem cells and mesenchymal stem cells from bone marrow and adipose tissue. Biotechnol Lett. 2011;33(6): 1257-1264.[37]Kasper G, Mao L, Geissler S, et al. Insights into mesenchymal stem cell aging: involvement of antioxidant defense and actin cytoskeleton. Stem Cells. 2009;27(6):1288-1297.[38]XU HZ, Su JS. ZHonghua Linchuang Yishi Zazhi(Dianziban). 2010;4(4):76-78.徐红珍,苏俭生. 组织工程骨的血管化研究进展[J].中华临床医师杂志(电子版), 2010,4(4):76-78.[39]Gao H, Wang MY. Gannan Yixueyuan Xuebao. 2011;123(4): 171-172.高辉,王茂源. 血管内皮生长因子在骨缺损修复中的研究进展[J]. 赣南医学院学报,2011,123(4):171-172.[40]Ma XF, Zhu XQ, He YL, et al. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu.2010;14(12):2097-2100.马雪峰,朱肖奇,贺用礼,等. 生物衍生骨体外复合构建组织工程化骨修复兔桡骨-骨膜缺损:血管化进程及其生物力学性能[J]. 中国组织工程研究与临床康复,2010,14(12):2097-2100.[41]Liu W, Aihemaitijiang•Yusufu,Chen YF. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2010;14(7): 146-1151.刘伟,艾合买提江•玉素甫,陈永峰.筋膜包裹的骨髓间充质干细胞/聚己内酯复合体血管化组织工程骨修复比格犬骨缺损[J]. 中国组织工程研究与临床康复,2010,14(7):1146-1151. |
| [1] | Pu Rui, Chen Ziyang, Yuan Lingyan. Characteristics and effects of exosomes from different cell sources in cardioprotection [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(在线): 1-. |
| [2] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [3] | Zhang Xiumei, Zhai Yunkai, Zhao Jie, Zhao Meng. Research hotspots of organoid models in recent 10 years: a search in domestic and foreign databases [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1249-1255. |
| [4] | Wang Zhengdong, Huang Na, Chen Jingxian, Zheng Zuobing, Hu Xinyu, Li Mei, Su Xiao, Su Xuesen, Yan Nan. Inhibitory effects of sodium butyrate on microglial activation and expression of inflammatory factors induced by fluorosis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1075-1080. |
| [5] | Wang Xianyao, Guan Yalin, Liu Zhongshan. Strategies for improving the therapeutic efficacy of mesenchymal stem cells in the treatment of nonhealing wounds [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1081-1087. |
| [6] | Liao Chengcheng, An Jiaxing, Tan Zhangxue, Wang Qian, Liu Jianguo. Therapeutic target and application prospects of oral squamous cell carcinoma stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1096-1103. |
| [7] | Xie Wenjia, Xia Tianjiao, Zhou Qingyun, Liu Yujia, Gu Xiaoping. Role of microglia-mediated neuronal injury in neurodegenerative diseases [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1109-1115. |
| [8] | Li Shanshan, Guo Xiaoxiao, You Ran, Yang Xiufen, Zhao Lu, Chen Xi, Wang Yanling. Photoreceptor cell replacement therapy for retinal degeneration diseases [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1116-1121. |
| [9] | Jiao Hui, Zhang Yining, Song Yuqing, Lin Yu, Wang Xiuli. Advances in research and application of breast cancer organoids [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1122-1128. |
| [10] | Wang Shiqi, Zhang Jinsheng. Effects of Chinese medicine on proliferation, differentiation and aging of bone marrow mesenchymal stem cells regulating ischemia-hypoxia microenvironment [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1129-1134. |
| [11] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [12] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [13] | Hou Jingying, Yu Menglei, Guo Tianzhu, Long Huibao, Wu Hao. Hypoxia preconditioning promotes bone marrow mesenchymal stem cells survival and vascularization through the activation of HIF-1α/MALAT1/VEGFA pathway [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 985-990. |
| [14] | Shi Yangyang, Qin Yingfei, Wu Fuling, He Xiao, Zhang Xuejing. Pretreatment of placental mesenchymal stem cells to prevent bronchiolitis in mice [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 991-995. |
| [15] | Liang Xueqi, Guo Lijiao, Chen Hejie, Wu Jie, Sun Yaqi, Xing Zhikun, Zou Hailiang, Chen Xueling, Wu Xiangwei. Alveolar echinococcosis protoscolices inhibits the differentiation of bone marrow mesenchymal stem cells into fibroblasts [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 996-1001. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||