Chinese Journal of Tissue Engineering Research ›› 2013, Vol. 17 ›› Issue (22): 4107-4114.doi: 10.3969/j.issn.2095-4344.2013.22.017
Previous Articles Next Articles
Interlocking intramedullary nail versus minimally invasive percutaneous plate osteosynthesis in the treatment of middle and distal tibial fracture in adults: A meta-analysis
Zhang Xuan-xuan, Long Teng-fei, Zhang Pi-jun, Zhao Hui, Wang Gang
- Department of Orthopedic Trauma, Nanfang Hospital of Southern Medical University, Guangzhou 510515, Guangdong Province, China
-
Online:2013-05-28Published:2013-05-28 -
Contact:Wang Gang, Master, Chief physician, Professor, Department of Orthopedic Trauma, Nanfang Hospital of Southern Medical University, Guangzhou 510515, Guangdong Province, China wgfr@163.com -
About author:Zhang Xuan-xuan★, Studying for master’s degree, Department of Orthopedic Trauma, Nanfang Hospital of Southern Medical University, Guangzhou 510515, Guangdong Province, China ahdszxx@163.com
CLC Number:
Cite this article
Zhang Xuan-xuan, Long Teng-fei, Zhang Pi-jun, Zhao Hui, Wang Gang. Interlocking intramedullary nail versus minimally invasive percutaneous plate osteosynthesis in the treatment of middle and distal tibial fracture in adults: A meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2013, 17(22): 4107-4114.
share this article

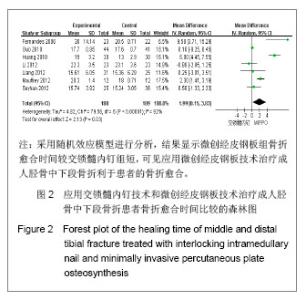
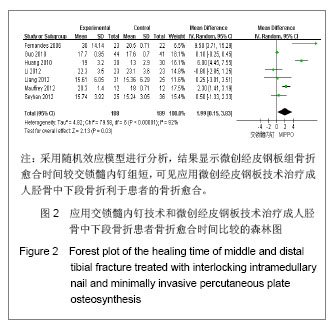
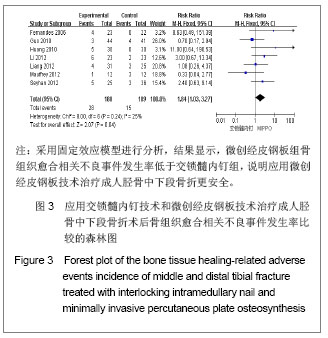
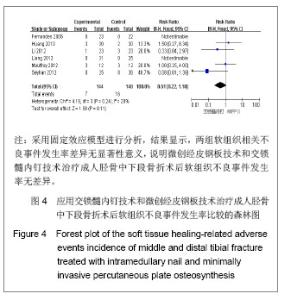
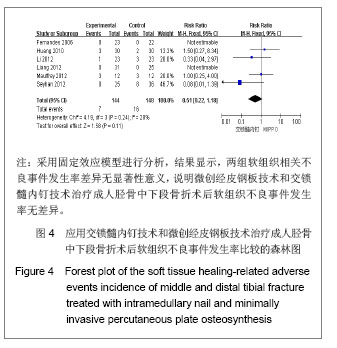
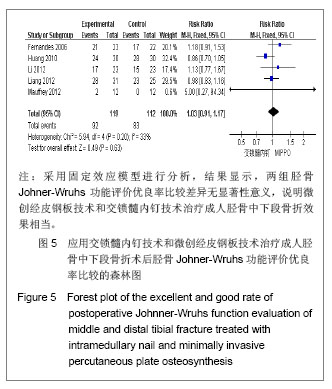
纳入研究中,有6个研究统计了软组织相关不良事件,共纳入292例患者,其中交锁髓内钉组144例,微创经皮钢板组148例。各研究间无异质性(I2=28%,P=0.24),用固定效应模型进行分析。Meta分析结果显示,两组软组织相关不良事件发生率差异无显著性意义[RR=0.51,95%CI(0.22,1.18),P=0.11]。 2.3.5 胫骨Johner-Wruhs功能评价优良率 纳入的研究中,有5个研究统计了术后12个月Johner-Wruhs功能评价优良率,共纳入231例患者,其中交锁髓内钉组119例,微创经皮钢板组112例。各研究间无异质性(I2=33%,P=0.20),用固定效应模型进行分析。Meta分析结果见图5。 由图5可见,两组胫骨Johner-Wruhs功能评价优良率比较差异无显著性意义[RR=1.03,95%CI(0.91,1.17),P=0.63],说明微创经皮钢板技术和交锁髓内钉技术治疗成人胫骨中下段骨折效果相当。"
| [1]Tang X. Dalian: Dalian Yike Daxue. 2006.汤欣.胫骨血运的解剖研究及不同术式对胫骨血运的影响[D]. 大连:大连医科大学,2006.[2]Huang W. Changsha: Zhongnan Daxue. 2010.黄文.经皮微创钢板内固定与交锁髓内钉治疗胫骨干骨折的疗效比较[D].长沙:中南大学,2010.[3]Bedi A, Le TT, Karunakar MA. Surgical treatment of nonarticular distal tibia fractures. J Am Acad Orthop Surg. 2006;14(7):406-416.[4]Wang ZK. Dalian: Dalian Yike Daxue. 2011.王自科.微创经皮钢板与交锁髓内钉固定治疗胫骨下端骨折的疗效比较[D].大连:大连医科大学,2011.[5]Xu ST, Ge BF, Xu YK. Beijing: Renmin Junyi Chubanshe. 2004.胥少汀,葛宝丰,徐印坎.实用骨科学[M].北京:人民军医出版社, 2004.[6]Fan CY, Chiang CC, Chuang TY, et al. Interlocking nails for displaced metaphyseal fractures of the distal tibia. Injury. 2005;36(5):669-674.[7]Xu HB, Zhang PS, Wang HB. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2007;11(32):6481-6483.徐海波,张普晟,王洪兵.微创经皮钢板置入内固定治疗胫腓骨骨折的技术操作特点[J].中国组织工程研究与临床康复,2007, 11(32): 6481-6483.[8]Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med. 2009;3(3):e123-130. [9]Li ZY, Feng HL, Zhang YY, et al. Hebei Yiyao. 2005;27(12): 888-889.李增炎,冯和林,张英泽,等.带锁髓内钉与微创经皮钢板治疗胫腓骨骨折的临床比较研究[J].河北医药,2005,27(12):888- 889.[10]Jüni P, Altman DG, Egger M. Systematic reviews in health care: Assessing the quality of controlled clinical trials. BMJ. 2001;323(7303):42-46.[11]Johner R, Wruhs O. Classification of tibial shaft fractures and correlation with results after rigid internal fixation. Clin Orthop Relat Res. 1983;(178):7-25.[12]Fernandes HJ, Sakaki MH, Silva Jdos S, et al. Comparative multicenter study of treatment of multi-fragmented tibial diaphyseal fractures with nonreamed interlocking nails and with bridging plates. Clinics (Sao Paulo). 2006;61(4):333-338.[13]Guo JJ, Tang N, Yang HL, et al. A prospective, randomised trial comparing closed intramedullary nailing with percutaneous plating in the treatment of distal metaphyseal fractures of the tibia. J Bone Joint Surg Br. 2010;92(7):984-988.[14]Liang BW, Zhao JM, Yin GQ, et al. Zhongguo Zuzhi Gongcheng Yanjiu. 2012;16(17):3116-3120.梁博伟,赵劲民,殷国前,等.经皮微创钢板固定治疗胫骨下段骨折:与交锁髓内钉固定和切开复位钢板内固定的比较[J].中国组织工程研究,2012,16(17):3116-3120.[15]Mauffrey C, McGuinness K, Parsons N, et al. A randomised pilot trial of "locking plate" fixation versus intramedullary nailing for extra-articular fractures of the distal tibia. J Bone Joint Surg Br. 2012;94(5):704-708.[16]Seyhan M, Unay K, Sener N. Intramedullary nailing versus percutaneous locked plating of distal extra-articular tibial fractures: a retrospective study. Eur J Orthop Surg Traumatol. In press.[17]Li Y, Liu L, Tang X, et al. Comparison of low, multidirectional locked nailing and plating in the treatment of distal tibial metadiaphyseal fractures. Int Orthop. 2012;36(7):1457-1462.[18]Dai P, Chen XL, Ma CZ. Dalian: 2006363. Beijing: Zhonghua Yixuehui Jizhen Yixue Fenhui. 2006.代平,陈新来,马灿泽.非扩髓髓内钉与钢板治疗胫骨干开放性骨折的疗效比较[C].大连:2006363.北京:中华医学会急诊医学分会, 2006.[19]Benirschke SK, Melder I, Henley MB, et al. Closed interlocking nailing of femoral shaft fractures: assessment of technical complications and functional outcomes by comparison of a prospective database with retrospective review. J Orthop Trauma. 1993;7(2):118-122.[20]Klein MP, Rahn BA, Frigg R, et al. Reaming versus non-reaming in medullary nailing: interference with cortical circulation of the canine tibia. Arch Orthop Trauma Surg. 1990;109(6):314-316.[21]Lindvall E, Sanders R, Dipasquale T, et al. Intramedullary nailing versus percutaneous locked plating of extra-articular proximal tibial fractures: comparison of 56 cases. J Orthop Trauma. 2009;23(7):485-492.[22]Giannoudis PV, Snowden S, Matthews SJ, et al. Temperature rise during reamed tibial nailing. Clin Orthop Relat Res. 2002; (395):255-261.[23]Wu Y, Wang MY, Rong GW, et al. Zhonghua Waike Zazhi. 1998;36(8):461-463.武勇,王满宜,荣国威,等.非扩髓带锁髓内针治疗胫腓骨骨折[J].中华外科杂志,1998,36(8):461-463.[24]Robinson CM, O'Donnell J, Will E, et al. Dropped hallux after the intramedullary nailing of tibial fractures. J Bone Joint Surg Br. 1999;81(3):481-484.[25]Court-Brown CM, Gustilo T, Shaw AD. Knee pain after intramedullary tibial nailing: its incidence, etiology, and outcome. J Orthop Trauma. 1997;11(2):103-105.[26]Zelle BA, Bhandari M, Espiritu M, et al. Treatment of distal tibia fractures without articular involvement: a systematic review of 1125 fractures. J Orthop Trauma. 2006;20(1):76-79.[27]Im GI, Tae SK. Distal metaphyseal fractures of tibia: a prospective randomized trial of closed reduction and intramedullary nail versus open reduction and plate and screws fixation. J Trauma. 2005;59(5):1219-1223.[28]Beardi J, Hessmann M, Hansen M, et al. Operative treatment of tibial shaft fractures: a comparison of different methods of primary stabilisation. Arch Orthop Trauma Surg. 2008; 128 (7):709-715.[29]Vallier HA, Le TT, Bedi A. Radiographic and clinical comparisons of distal tibia shaft fractures (4 to 11 cm proximal to the plafond): plating versus intramedullary nailing. J Orthop Trauma. 2008;22(5):307-311.[30]Ozsoy MH, Tuccar E, Demiryurek D, et al. Minimally invasive plating of the distal tibia: do we really sacrifice saphenous vein and nerve? A cadaver study. J Orthop Trauma. 2009; 23(2):132-138.[31]Tyllianakis M, Megas P, Giannikas D, et al. Interlocking intramedullary nailing in distal tibial fractures. Orthopedics. 2000;23(8):805-808.[32]Krettek C, Schandelmaier P, Miclau T, et al. Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in proximal and distal femoral fractures. Injury. 1997; 28 Suppl 1:A20-30.[33]Lau TW, Leung F, Chan CF, et al. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop. 2008;32(5):697-703.[34]Farouk O, Krettek C, Miclau T, et al. Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma. 1999;13(6):401-406.[35]Stoffel K, Klaue K, Perren SM. Functional load of plates in fracture fixation in vivo and its correlate in bone healing. Injury. 2000 May;31 Suppl 2:S-B37-50.[36]El-Zayat BF, Zettl R, Efe T, et al. Minimally invasive treatment of geriatric and osteoporotic femur fractures with polyaxial locking implants (NCB-DF®). Unfallchirurg. 2012;115(2): 134-144.[37]Kao FC, Tu YK, Su JY, et al. Treatment of distal femoral fracture by minimally invasive percutaneous plate osteosynthesis: comparison between the dynamic condylar screw and the less invasive stabilization system. J Trauma. 2009;67(4):719-726.[38]Kolb W, Guhlmann H, Windisch C, et al. Fixation of distal femoral fractures with the Less Invasive Stabilization System: a minimally invasive treatment with locked fixed-angle screws. J Trauma. 2008;65(6):1425-1434.[39]Walz M, Auerbach F, Kolbow B, et al. Minimally invasive treatment of monocondylar tibial plateau fractures. Percutaneous reduction and small fragment osteosynthesis. Unfallchirurg. 2006;109(5):367-376. |
| [1] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [2] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [3] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [4] | Hu Kai, Qiao Xiaohong, Zhang Yonghong, Wang Dong, Qin Sihe. Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1465-1470. |
| [5] | Wang Yongsheng, Wu Yang, Li Yanchun. Effect of acute high-intensity exercise on appetite hormones in adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1305-1312. |
| [6] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [7] | Yang Weiqiang, Ding Tong, Yang Weike, Jiang Zhengang. Combined variable stress plate internal fixation affects changes of bone histiocyte function and bone mineral density at the fractured end of goat femur [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 890-894. |
| [8] | Yuan Xinping, Shao Yanbo, Wu Chao, Wang Jianling, Tong Liangcheng, Li Ying. Accuracy of target bone segments in personalized differential modeling and simulation of CT scanning parameters at fracture end [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 912-916. |
| [9] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Intravenous, topical tranexamic acid alone or their combination in total knee arthroplasty: a meta-analysis of randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 948-956. |
| [10] | Li Yan, Wang Pei, Deng Donghuan, Yan Wei, Li Lei, Jiang Hongjiang. Electroacupuncture for pain control after total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 957-963. |
| [11] | He Xiangzhong, Chen Haiyun, Liu Jun, Lü Yang, Pan Jianke, Yang Wenbin, He Jingwen, Huang Junhan. Platelet-rich plasma combined with microfracture versus microfracture in the treatment of knee cartilage lesions: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 964-969. |
| [12] | Hua Haotian, Zhao Wenyu, Zhang Lei, Bai Wenbo, Wang Xinwei. Meta-analysis of clinical efficacy and safety of antibiotic artificial bone in the treatment of chronic osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 970-976. |
| [13] | Zhan Fangbiao, Cheng Jun, Zou Xinsen, Long Jie, Xie Lizhong, Deng Qianrong. Intraoperative intravenous application of tranexamic acid reduces perioperative bleeding in multilevel posterior spinal surgery: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 977-984. |
| [14] | Cheng Shigao, , Wang Wanchun, Jiang Dong, Li Tengfei, Li Xun, Ren Lian. Comparison of the standard and long-stem bone cement prosthesis replacement in the treatment of intertrochanteric fractures in elderly patients [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 362-367. |
| [15] | Zhong Yuanming, Wan Tong, Zhong Xifeng, Wu Zhuotan, He Bingkun, Wu Sixian. Meta-analysis of the efficacy and safety of percutaneous curved vertebroplasty and unilateral pedicle approach percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 456-462. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||