Chinese Journal of Tissue Engineering Research ›› 2018, Vol. 22 ›› Issue (18): 2807-2812.doi: 10.3969/j.issn.2095-4344.0865
Previous Articles Next Articles
Early vascularization of calcined antler cancellous bone in repairing bone defects
Peng Hui1, Zhang Xue-hui2
- 1The 3rd Dental Center, Peking University Hospital of Stomatology, Beijing 100191, China; 2Department of Dental Materials, Peking University Hospital of Stomatology, Beijing 100081, China
-
Received:2018-04-21Online:2018-06-28Published:2018-06-28 -
Contact:Zhang Xue-hui, Associate researcher, Department of Dental Materials, Peking University Hospital of Stomatology, Beijing 100081, China -
About author:Peng Hui, Master, Physician, the 3rd Dental Center, Peking University Hospital of Stomatology, Beijing 100191, China -
Supported by:the National High-Technology Research and Development Research of China (863 Program), No. 2015AA033601
CLC Number:
Cite this article
Peng Hui, Zhang Xue-hui. Early vascularization of calcined antler cancellous bone in repairing bone defects[J]. Chinese Journal of Tissue Engineering Research, 2018, 22(18): 2807-2812.
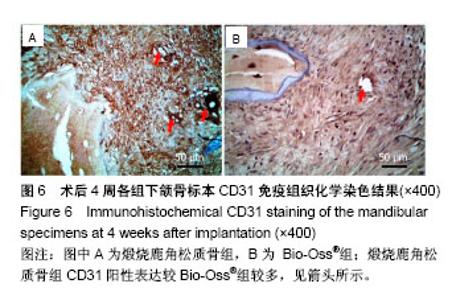
share this article
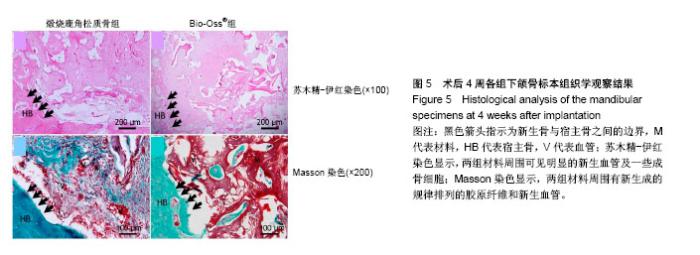
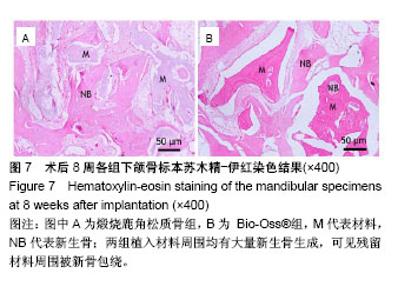
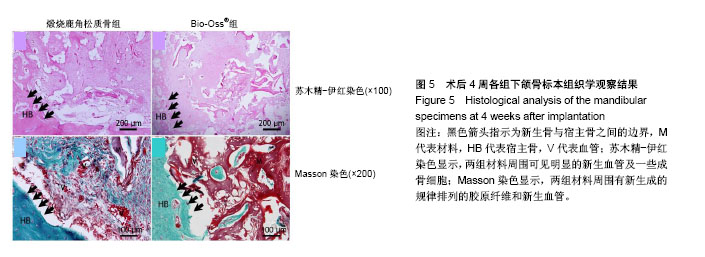
2.3 动物植入实验早期血管化评价 术后4周苏木精-伊红染色显示,在植入的煅烧鹿角松质骨和Bio-Oss®材料周围可见明显的新生血管及一些成骨细胞,表明在骨填充材料植入体内新骨形成阶段伴随新生血管的发生;Masson染色结果显示,在骨缺损区内,填充材料周围有新生成的规律排列的胶原纤维(呈绿色)和新生血管(V),而且煅烧鹿角松质骨组比Bio-Oss®组血管化效果更为明显(图5)。 为了进一步检测骨缺损修复初期新生血管生成的情况,用血管内皮细胞特性的标志物CD31进行免疫组织化学染色,结果显示骨形成初期,煅烧鹿角松质骨组CD31阳性表达(图6)较Bio-Oss®组较多,也就是说植入煅烧鹿角松质骨的骨缺损部位新骨生成中伴随较大量的新生血管生成。"
| [1] Hesse E,Kluge G,Atfi A,et al Repair of a segmental long bone defect in human by implantation of a novel multiple disc graft. Bone.2010;46:1457-1463. [2] Parikh SN.Bone graft substitutes in modern orthopedics. Orthopedics.2002;25(11):1301-1309. [3] Torroni A.Engineered bone grafts and bone flaps for maxillofacial defects: state of the art.J Oral Maxillofac Surg. 2009;67:1121-1127. [4] Muschler GF,Nakamoto C,Griffith LG.Engineering principles of clinical cell-based tissue engineering.J Bone Joint Surg Am. 2004;86-A(7):1541-1558.[5] Liu T,Wu G,Wismeijer D,et al.Deproteinized bovine bone functionalized with the slow delivery of BMP-2 for the repair of critical-sized bone defects in sheep.Bone. 2013;56(1):110-118.[6] Carmagnola D,Adriaens P,Berglundh T.Healing of human extraction sockets filled with Bio-Oss®. Clin Oral Implants Res.2003;14:137-143. [7] Park SA,Shin JW,Yang YI,et al.In vitro study of osteogenic differentiation of bone marrow stromal cells on heat-treated porcine trabecular bone blocks.Biomaterials. 2004;25(3): 527-535. [8] Zitzmann NU,Scharer P,Marinello CP,et al.Alveolar ridge augmentation with Bio-Oss®: a histologic study in humans.Int J Periodontics Restorative Dent.2001;21(3):289-295. [9] Briem D,Linhart WL,Lehmann W,et al.Long-term results after application of a porous hydroxyapatite ceramic (Endobon) in proximal tibia fractures.Unfallchirurg. 2002; 105:128-133. [10] Figueiredo M,Henriques J,Martins G,et al.Physicochemical characterization of biomaterials commonly used in dentistry as bone substitutes—comparison with human bone.J Biomed Mater Res B.2010; 92(B):409-419. [11] Chen PY,Stokes AG,Mckittrick J.Comparison of the structure and mechanical properties of bovine femur bone and antler of the North American elk(Cervus elaphus canadensis).Acta Biomater.2009;5(2):693-706.[12] Zhang X,Cai Q,Liu H,et al.Osteoconductive effectiveness of bone graft derived from antler cancellous bone: an experimental study in the rabbit mandible defect model.Int J Oral Maxillofac Surg. 2012;41(11):1330-1337.[13] Zhang X,Xu M,Song L,et al.Effects of compatibility of deproteinized antler cancellous bone with various bioactive factors on their osteogenic potential.Biomaterials. 2013; 34(36):9103-9114.[14] Wei J,Xu M,Zhang X,et al.Enhanced Osteogenic Behavior of ADSCs Produced by Deproteinized Antler Cancellous Bone and Evidence for Involvement of ERK Signaling Pathway. Tissue Eng Part A.2015; 21:1810-1821.[15] Grellier M,Bordenave L,Amédée J.Cell-to-cell communication between osteogenic and endothelial lineages: implications for tissue engineering.Trends Biotechnol.2009;27(10):562-571.[16] Griffith LG,Naughton G.Tissue engineering--current challenges and expanding opportunities. Science. 2002;295 (5557):1009-1014.[17] Otfinowski J.Heterotopic Indution of osteogenesis in the course of neural injury.J Patol Pol.1993;44(3):133-168.[18] Hara-Irie F,Amizuka N,Ozawa H.Immunohistoehemieal and ultrastructural localization of CGRP-Positive nerve fibers at the epiphyseal trabeeules facing the growth Plate of rat femurs. Bone.1996;18(1):29-39.[19] Develioglu H,Saraydin SU,Kartal U.The bone-healing effect of a xenograft in a rat calvarial defect model.Dent Mater J. 2009,28(4):396-400. [20] Develioglu H,Saraydin SU,Kartal U,et al.Evaluation of the long-term results of rat cranial bone repair using a particular xenograft.J Oral Implantol.2010;36(3):167-173. [21] Landete-Castillejos T,Estevez JA,Martínez A,et al.Does chemical composition of antler bone reflect the physiological effort made to grow it?Bone.2007;40(4):1095-1102.[22] Wu F,Li H,Jin L,et al.Deer antler base as a traditional Chinese medicine: A review of its traditional uses, chemistry and pharmacology.J Ethnopharmacol.2013;145(2):403-415. [23] Ooi CY,Hamdi M,Ramesh S.Properties of hydroxyapatite produced by annealing of bovine bon.Ceramic Int. 2007; 33(7):1171-1177.[24] Figueiredo M,Fernando A,Martins G,et al.Effect of the calcination temperature on the composition and microstructure of hydroxyapatite derived from human and animal bone.Ceramic Int.2010;36(8): 2383-2393.[25] Meng S,Zhang X,Xu M,et al.Effects of deer age on the physicochemical properties of deproteinized antler cancellous bone: an approach to optimize osteoconductivity of bone graft.Biomed Mater.2015;10(3):035006.[26] Kasten P,Beyen I,Niemeyer P,et al.Porosity and pore size of beta-tricalcium phosphate scaffold can influence protein production and osteogenic differentiation of human mesenchymal stem cells: an in vitro and in vivo study.Acta Biomater.2008;4(6):1904-1915.[27] Karageorgiou V,Kaplan D.Porosity of 3D biomaterial scaffolds and osteogenesis.Biomaterials.2005; 26(27):5474-5491.[28] van Steenberghe D,Callens A,Geers L,et al.The clinical use of deproteinized bovine bone mineral on bone regeneration in conjunction with immediate implant installation.Clin Oral Implants Res. 2000;11(3):210-216.[29] Laurencin C,Khan Y,Elamin SF.Bone graft substitutes.Expert Rev Med Devices.2006;3(1):49-57.[30] Linsley CS,Wu BM,Tawil B.Mesenchymal stem cell growth on and mechanical properties of fibrin-based biomimetic bone scaffolds.J Biomed Mater Res A.2016;104(12):2945-2953.[31] Goss TP,Cox QG,Jinnah RH.History and current application of bone transplantation. Orthopedics.1993;16(8):895-900.[32] Kirkeby OJ,Nordsletten L,Skjeldal S,et al.Circulation in corticocancelous bone grafts measured with laser Doppler flowmettry. An experimental study in rats.Stand J Plast Reconstr Sury Hand Sury.1994;28(4):249-254.[33] Burder SP,Fox BS.Tissue engineering of bone. Cell based strategies.Clin Orthop Relat Res.1999;(367 Suppl):S68-83.[34] Griller M,Ferreira-Tojais N,Bourget C,et al.Role of vascular endothelial growth factor in the communication between human osteoprogenitors and endothelial cells.J Cell Biochem. 2009;106(3): 390-398. [35] Villars F,Bordenave L,Bareille R,et al.Effect of human endothelial cells on human bone marrow stromal cell phenotype: role of VEGF?J Cell Biochem. 2000;79(4): 672-685. [36] Aguirre A,Planell JA,Engel E.Dynamics of bone marrow-derived endothelial progenitor cell/mesenchymal stem cell interaction in co-culture and its implications in angiogenesis. Biochem Biophys Res Commun. 2010;400(2): 284-291. [37] Stein H,Perren SM,Cordey J,et al.The muscle bed--a crucial factor for fracture healing: a physiological concept. Orthopedics. 2002;25(12):1379-1383.[38] 鲍小刚,许国华.工程骨的快速血管化[J].中国组织工程研究, 2015,19(7):1063-1069.[39] Mastrogiacomo M,Corsi A,Francioso E,et al.Reconstruction of extensive long bone defects in sheep using resorbable bioceramics based on silicon stabilized tricalcium phosphate.Tissue Eng Part A.2006;12(5):1261-1273.[40] Geiger F,Bertram H,Berger I,et al.Vascular endothelial growth factor gene-activatedmatrix (VEGF165-GAM) enhances osteogenesis and angiogenesis in large segmental bone defects.J BoneMiner Res.2005;20(11):2028-2035.[41] 余希杰,杨志明,马骏荣.成骨细胞的细胞社会学特征[J].中国修复重建外科杂志,1998,12(6):350-354.[42] Das A,Botchwey E.Evaluation of angiogenesis and osteogenesis.Tissue Eng Part B Rev.2011; 17(6):403-414.[43] Kaigler D,Krebsbach PH,Polverini PJ,et al.Role of vascular endothelial growth factor in bone marrow stromal cell modulation of endothelial cells.Tissue Eng.2003;9(1):95-103.[44] Chandra VS,Baskar G,Suganthi RV,et al.Blood compatibility of iron-doped nanosize hydroxyapatite and its drug release. ACS Appl Mater Inter.2012;4:1200-1210. |
| [1] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [2] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [3] | Xu Dongzi, Zhang Ting, Ouyang Zhaolian. The global competitive situation of cardiac tissue engineering based on patent analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 807-812. |
| [4] | Wang Yujiao, Liu Dan, Sun Song, Sun Yong. Biphasic calcium phosphate loaded with advanced platelet rich fibrin can promote the activity of rabbit bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 504-509. |
| [5] | Chen Junyi, Wang Ning, Peng Chengfei, Zhu Lunjing, Duan Jiangtao, Wang Ye, Bei Chaoyong. Decalcified bone matrix and lentivirus-mediated silencing of P75 neurotrophin receptor transfected bone marrow mesenchymal stem cells to construct tissue-engineered bone [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 510-515. |
| [6] | Liu Jiangfeng. Nano-hydroxyapatite/polyamide 66 composite filling combined with locking plate in the treatment of fibrous dysplasia of femoral bone [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 542-547. |
| [7] | Ma Zhijie, Li Jingyu, Cao Fang, Liu Rong, Zhao Dewei. Influencing factors and biological property of novel biomedical materials: porous silicon carbide coated with bioactive tantalum [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 558-563. |
| [8] | Wu Zijian, Hu Zhaoduan, Xie Youqiong, Wang Feng, Li Jia, Li Bocun, Cai Guowei, Peng Rui. Three-dimensional printing technology and bone tissue engineering research: literature metrology and visual analysis of research hotspots [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 564-569. |
| [9] | Shi Xiaoxiu, Mao Shilong, Liu Yang, Ma Xingshuang, Luo Yanfeng. Comparison of tantalum and titanium (alloy) as orthopedic materials: physical and chemical indexes, antibacterial and osteogenic ability [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 593-599. |
| [10] | Chang Wenliao, Zhao Jie, Sun Xiaoliang, Wang Kun, Wu Guofeng, Zhou Jian, Li Shuxiang, Sun Han. Material selection, theoretical design and biomimetic function of artificial periosteum [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 600-606. |
| [11] | Liu Fei, Cui Yutao, Liu He. Advantages and problems of local antibiotic delivery system in the treatment of osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 614-620. |
| [12] | Li Xiaozhuang, Duan Hao, Wang Weizhou, Tang Zhihong, Wang Yanghao, He Fei. Application of bone tissue engineering materials in the treatment of bone defect diseases in vivo [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 626-631. |
| [13] | Zhang Zhenkun, Li Zhe, Li Ya, Wang Yingying, Wang Yaping, Zhou Xinkui, Ma Shanshan, Guan Fangxia. Application of alginate based hydrogels/dressings in wound healing: sustained, dynamic and sequential release [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 638-643. |
| [14] | Chen Jiana, Qiu Yanling, Nie Minhai, Liu Xuqian. Tissue engineering scaffolds in repairing oral and maxillofacial soft tissue defects [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 644-650. |
| [15] | Xing Hao, Zhang Yonghong, Wang Dong. Advantages and disadvantages of repairing large-segment bone defect [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 426-430. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||