Chinese Journal of Tissue Engineering Research ›› 2018, Vol. 22 ›› Issue (23): 3621-3627.doi: 10.3969/j.issn.2095-4344.0329
Previous Articles Next Articles
Microsurgery anterior cervical discectomy and fusion for cervical degenerative diseases with bony compression
Wo Jin1, Yuan Feng2
- 1Graduate School of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China; 2Department of Orthopedics, the Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China
-
Online:2018-08-18Published:2018-08-18 -
Contact:Yuan Feng, Professor, Chief physician, Master’s supervisor, Department of Orthopedics, the Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China -
About author:Wo Jin, Master candidate, Graduate School of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China -
Supported by:the Project of Health Department of Jiangsu Province, No. H200927; the “Six Talent Peaks” Project of Jiangsu Province, No. 53031106; the Scientific Research Project of Health Department of Jiangsu Province, No. H201630; the Important Research and Development Program (Social Development) of Jiangsu Province, No. BE2016647
CLC Number:
Cite this article
Wo Jin, Yuan Feng. Microsurgery anterior cervical discectomy and fusion for cervical degenerative diseases with bony compression[J]. Chinese Journal of Tissue Engineering Research, 2018, 22(23): 3621-3627.
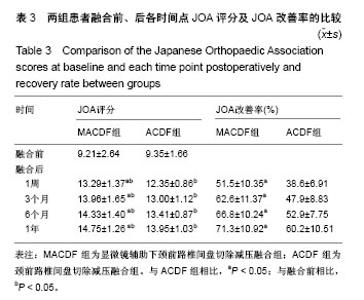
share this article
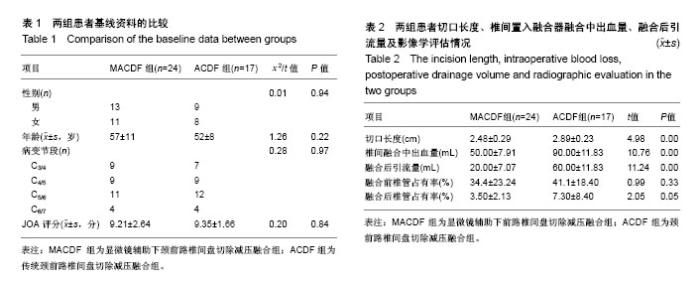
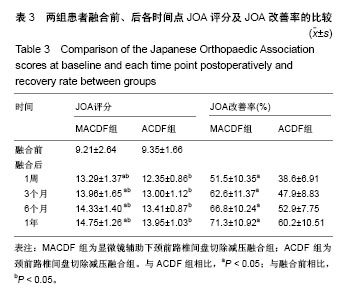
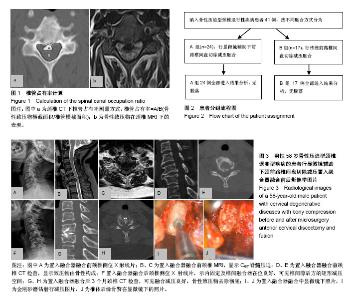
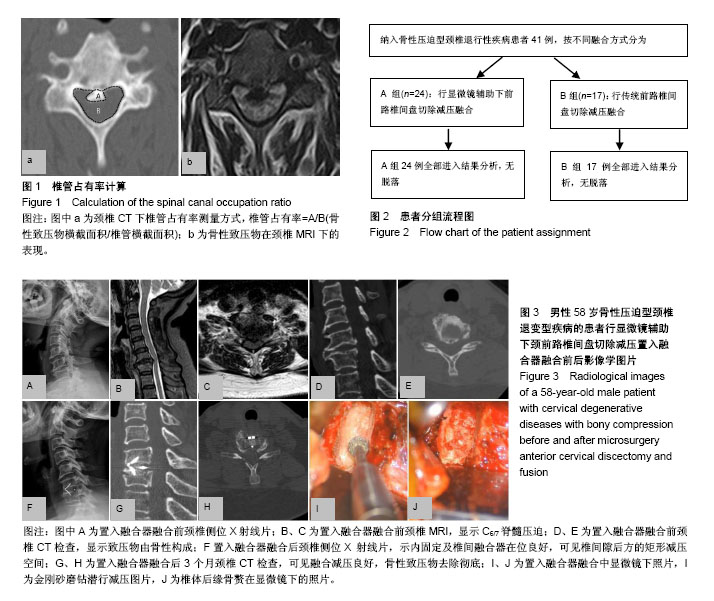
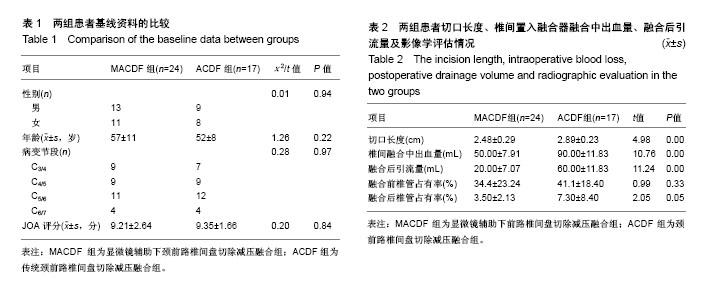
2.1 参与者数量分析 按照纳入与排除标准,纳入41例骨性压迫型颈椎退行性疾病的患者,按融合方式分为2组,全部进入结果分析,试验流程图见图2。 2.2 一般临床资料 基线资料包括性别、年龄、病变节段见表1,2组患者比较差异无显著性意义(P > 0.05)。MACDF组椎间融合切口长度,椎间融合中平均出血量,融合后平均引流量均显著低于ACDF组(P < 0.05),见表2。 2.3 影像学指标 两组患者融合前椎管占有率相比,差异无显著性意义。置入融合器融合后椎管占有率相比,MACDF组显著低于ACDF组(P < 0.05),表2。 2.4 神经功能评估 两组患者融合前JOA评分,比较差异无显著性意义(P > 0.05)。两组患者融合各时间点JOA评分,均较术前显著改善(P < 0.05),且MACDF组融合后各时间点JOA评分及改善率均显著高于ACDF组(P < 0.05),表3。"
| [1] 马学晓,陈伯华,张岩,等.经关节突入路治疗前方骨性压迫型胸椎退行性疾病[J].中华骨科杂志, 2010, 30(11):1068-1072.[2] Gu Y, Shi J, Cao P, et al. Clinical and imaging predictors of surgical outcome in multilevel cervical ossification of posterior longitudinal ligament: An analysis of 184 patients. PLoS One. 2015;10(9):e0136042.[3] Rao K, Sahu BP, Purohit AK. Surgical outcome in patients with cervical ossified posterior longitudinal ligament: A single institutional experience. Asian J Neurosurg. 2014; 9(4):196-202. [4] An HS, AlShihabi L, Kurd M. Surgical treatment for ossification of the posterior longitudinal ligament in the cervical spine. J Am Acad Orthop Surg. 2014;22(7):420-429.[5] 潘冬生,宋振全,赵明光,等. 术中CT辅助下颈椎前路手术骨减压效果的评估[J].中华神经外科杂志, 2017, 33(2):124-127.[6] Chen Y, Yang L, Liu Y, et al. Surgical results and prognostic factors of anterior cervical corpectomy and fusion for ossification of the posterior longitudinal ligament . PLoS One.2014; 9(7):e102008.[7] 汪文龙,海涌,关立,等.前路或后路手术治疗颈椎后纵韧带骨化症的中期疗效观察[J].中国脊柱脊髓杂志,2016, 26(7):577-584.[8] Oppenheimer JH, Decastro I, Mcdonnel DE. Minimally invasive spine technology and minimally invasive spine surgery: a historical review. Neurosurg Focus. 2009;27(3): E9.[9] Kwon YJ. Long-term clinical and radiologic outcomes of minimally invasive posterior cervical foraminotomy . J Korean Neurosurg Soc.2014;56(3):224-229.[10] Sohn S, Chung CK, Yun TJ, et al. Epidemiological survey of ossification of the posterior longitudinal ligament in an adult korean population: Three-dimensional computed tomographic observation of 3240 cases. Calcif Tissue Int. 2014;94(6): 613-620.[11] Fujimori T, Watabe T, Iwamoto Y, et al. Prevalence, concomitance, and distribution of ossification of the spinal ligaments: Results of whole spine CT scans in 1500 Japanese patients. Spine. 2016; 41(21):1668-1676.[12] Mazur M D, White A, Mcevoy S, et al. Transcranial magnetic stimulation of the motor cortex correlates with objective clinical measures in patients with cervical spondylotic myelopathy. Spine.2014;39(14):1113-1120.[13] Yukawa Y, Kato F, Yoshihara H, et al. MR T2 image classification in cervical compression myelopathy: predictor of surgical outcomes. Spine. 2007;32(15):1675.[14] Hayashi H, Okada K, Hamada M, et al. Etiologic factors of myelopathy. A radiographic evaluation of the aging changes in the cervical spine. Clin Orthop Relat Res. 1987; 214(214): 200-209.[15] Toledano M, Bartleson JD. Cervical spondylotic myelopathy. Neurol Clin. 2013; 31(1):287-305. [16] Shen HX, Li L, Yang ZG, et a1. Position of increased signal intensity in the spinal cord on MR images: does it predict the outcome of cervical spondylotic myelopathy. Chin Med J. 2009;122(12):1418-1422. [17] Hacker RJ, Cauthen JC, Gilbert TJ, et al. A prospective randomized multicenter clinical evaluation of an anterior cervical fusion cage. Spine. 2000;25(20):2646.[18] Nicholson JA, Bhatt P. Ensuring adequate epidural decompression during the anterior approach to cervical spine for multi-level spondylotic myelopathy. Br J Neurosurg. 2012; 26(4):570-571.[19] Chen Y, Gun Y, La X. et a1. Surgical strategy for multilevel severe ossification of posterior longitudinal ligament in the cervical spine. Spinal Disord Tech. 2011. 24:24-30. [20] Jiang SD, Jiang LS, Dai LY. Anterior cervical discectomy and fusion versus anterior cervical corpectomy and fusion for multilevel cervical spondylosis: a systematic review. Arch Orthop Trauma Surg. 2012;132(2): 155-161.[21] Zhang JT, Wang LF, Liu YJ, et al. Relationship between developmental canal stenosis and surgical results of anterior decompression and fusion in patients with cervical spondylotic myelopathy. BMC Musculoskelet Disord.2015; 16(1):267.[22] Eubanks JD, Belding J, Schnaser E, et al. Congenital stenosis and adjacent segment disease in the cervical spine. Orthopedics. 2013;36(10):1251-1255.[23] Moussellard HP, Meyer A, Biot D, et al. Early neurological recovery course after surgical treatment of cervical spondylotic myelopathy: a prospective study with 2-year follow-up using three different functional assessment tests. Eur Spine J.2014;23(7):1508-1514.[24] Pavlov H, Torg JS, Robie B, et al. Cervical spinal stenosis: determination with vertebral body ratio method. Radiology. 1987; 164(3):771-775.[25] Hori T, Kawaguchi Y, Kimura T. How does the ossification area of the posterior longitudinal ligament thicken following cervical laminoplasty. Spine. 2007;32(19):551-556. [26] Kawaguchi Y, Nakano M, Yasuda T, et al. Anterior decompressive surgery after cervical laminoplasty in patients with ossification of the posterior longitudinal ligament. Spine J. 2014;14(6):955-963.[27] Chen TY, Crawford NR, Sonntag VK, et al. Biomechanical effects of progressive anterior cervical decompression. Spine. 2001;26(1):6-13.[28] Tetreault L, Ibrahim A, Côté P, et al. A systematic review of clinical and surgical predictors of complications following surgery for degenerative cervical myelopathy. J Neurosurg Spine.2016;24(1):77-99.[29] 王新伟,陈德玉,赵定麟,等.切除与不切除后纵韧带颈椎减压术后的MRI观察[J].中国脊柱脊髓杂志, 2003, 13(10):597-599.[30] 马航展,蔡东岭,李伟宽,等.颈椎前路手术中后纵韧带切除与否的临床探讨[J].实用医学杂志,2016, 32(5):786-789.[31] Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the Intervertebral disc and interbody fusion. J Bone Joint Surg Am.1958; 40(3):607.[32] Cooper PR. Cervical spondylotic myeolopathy: management with anterior operation. Neurosurg Spine.1992;3: 73-89.[33] ]Mcafee PC, Cunningham B, Dmitriev A, et al. Cervical disc replacement-porous coated motion prosthesis: a comparative biomechanical analysis showing the key role of the posterior longitudinal ligament. Spine.2003;28(20):176-185.[34] Kadoya S, Iizuka H, Nakamura T. Long-term outcome for surgically treated cervical spondylotic radiculopathy and myelopathy. Neurol Med Chir (Tokyo).2003;43(5):228.[35] Daentzer D. Microsurgical anterior cervical approach and the immediate impact of mechanical retractors. A case-control study. J Neurosci Rural Pract. 2015; 6(3):297.[36] Sun YF, Li L, Zhao JH, et al. Comparison between anterior approaches and posterior approaches for the treatment of multilevel cervical spondylotic myelopathy: A meta-analysis. Clin Neurol Neurosurg. 2015;134:28-36.[37] 李程,王冰,王一宇,等.两种前路手术治疗邻近双节段脊髓型颈椎病的临床效果[J].中国脊柱脊髓杂志,2015,25(5):433-437.[38] Eicker SO, Steiger HJ, Elkathib M. Transtubular microsurgical approach to treat lateral cervical disc herniation. World Neurosurg.2016;88:503-509.[39] Kim B, Yoon DH, Shin HC, et al. Surgical outcome and prognostic factors of anterior decompression and fusion for cervical compressive myelopathy due to ossification of the posterior longitudinal ligament. Spine J.2015;15(5):875-884. |
| [1] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [2] | Yao Rubin, Wang Shiyong, Yang Kaishun. Minimally invasive transforaminal lumbar interbody fusion for treatment of single-segment lumbar spinal stenosis improves lumbar-pelvic balance [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1387-1392. |
| [3] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [4] | Zhang Lei, Ma Li, Fu Shijie, Zhou Xin, Yu Lin, Guo Xiaoguang. Arthroscopic treatment of greater tuberosity avulsion fractures with anterior shoulder dislocation using the double-row suture anchor technique [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 895-900. |
| [5] | Xu Dongzi, Zhang Ting, Ouyang Zhaolian. The global competitive situation of cardiac tissue engineering based on patent analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 807-812. |
| [6] | Wu Zijian, Hu Zhaoduan, Xie Youqiong, Wang Feng, Li Jia, Li Bocun, Cai Guowei, Peng Rui. Three-dimensional printing technology and bone tissue engineering research: literature metrology and visual analysis of research hotspots [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 564-569. |
| [7] | Chang Wenliao, Zhao Jie, Sun Xiaoliang, Wang Kun, Wu Guofeng, Zhou Jian, Li Shuxiang, Sun Han. Material selection, theoretical design and biomimetic function of artificial periosteum [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 600-606. |
| [8] | Liu Fei, Cui Yutao, Liu He. Advantages and problems of local antibiotic delivery system in the treatment of osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 614-620. |
| [9] | Li Xiaozhuang, Duan Hao, Wang Weizhou, Tang Zhihong, Wang Yanghao, He Fei. Application of bone tissue engineering materials in the treatment of bone defect diseases in vivo [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 626-631. |
| [10] | Zhang Zhenkun, Li Zhe, Li Ya, Wang Yingying, Wang Yaping, Zhou Xinkui, Ma Shanshan, Guan Fangxia. Application of alginate based hydrogels/dressings in wound healing: sustained, dynamic and sequential release [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 638-643. |
| [11] | Chen Jiana, Qiu Yanling, Nie Minhai, Liu Xuqian. Tissue engineering scaffolds in repairing oral and maxillofacial soft tissue defects [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 644-650. |
| [12] | Liang Yan, Zhao Yongfei, Zhu Zhenqi, Liu Haiying, Mao Keya. Minimally invasive transforaminal lumbar interbody fusion in the treatment of sciatic scoliosis caused by lumbar disc herniation: a 2-year follow-up of coronal and sagittal balance [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 409-413. |
| [13] | Xing Hao, Zhang Yonghong, Wang Dong. Advantages and disadvantages of repairing large-segment bone defect [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 426-430. |
| [14] | Meng Lingjie, Qian Hui, Sheng Xiaolei, Lu Jianfeng, Huang Jianping, Qi Liangang, Liu Zongbao. Application of three-dimensional printing technology combined with bone cement in minimally invasive treatment of the collapsed Sanders III type of calcaneal fractures [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3784-3789. |
| [15] | Qian Xuankun, Huang Hefei, Wu Chengcong, Liu Keting, Ou Hua, Zhang Jinpeng, Ren Jing, Wan Jianshan. Computer-assisted navigation combined with minimally invasive transforaminal lumbar interbody fusion for lumbar spondylolisthesis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3790-3795. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||