Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (5): 1162-1170.doi: 10.12307/2026.034
Previous Articles Next Articles
Therapeutic efficacy of extracorporeal shock wave therapy in the upper trapezius muscle area combined with exercise control training in patients with chronic non-specific neck pain
Li Haojing, Wang Xin, Song Chenglin, Zhang Shengnan, Chen Yunxin
- Shenyang Sport University, Shenyang 110102, Liaoning Province, China
-
Received:2024-11-19Accepted:2025-01-09Online:2026-02-18Published:2025-06-24 -
Contact:Song Chenglin, PhD, Associate chief physician, Shenyang Sport University, Shenyang 110102, Liaoning Province, China -
About author:Li Haojing, Master candidate, Rehabilitation therapist, Shenyang Sport University, Shenyang 110102, Liaoning Province, China -
Supported by:National Key Research & Development Program Project, No. 2018YFF0300502 (to WX); Key Laboratory Research Project of the Ministry of Education, No. Heng20230008 (to WX)
CLC Number:
Cite this article
Li Haojing, Wang Xin, Song Chenglin, Zhang Shengnan, Chen Yunxin. Therapeutic efficacy of extracorporeal shock wave therapy in the upper trapezius muscle area combined with exercise control training in patients with chronic non-specific neck pain[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1162-1170.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

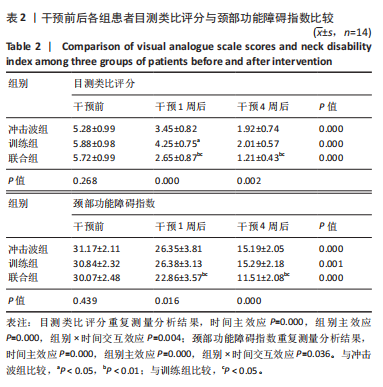
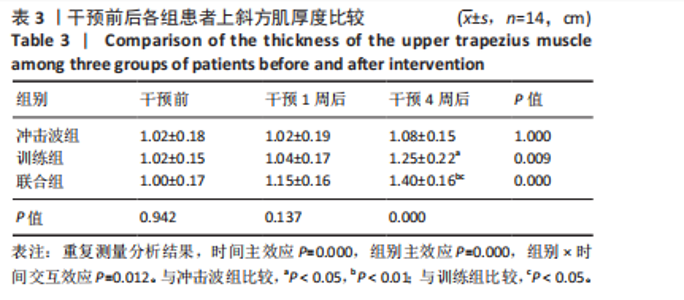
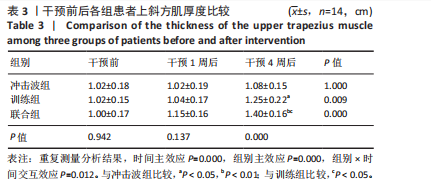
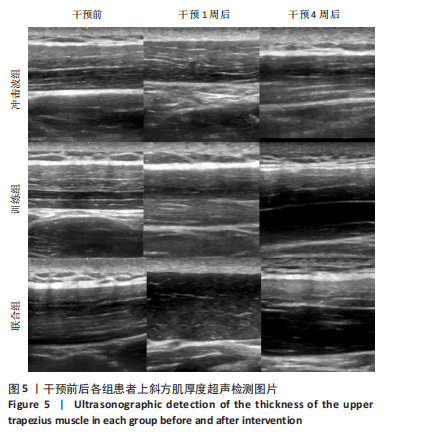
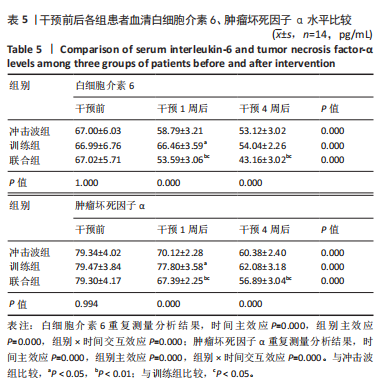
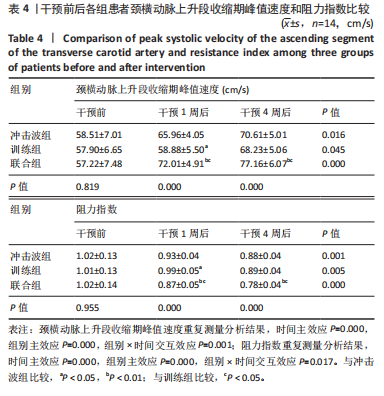
与干预前比较,训练组、联合组干预4周后的上斜方肌厚度增加(P < 0.01)。干预前,3组间上斜方肌厚度比较差异无显著性意义(P > 0.05)。干预4周后,联合组上斜方肌厚度大于冲击波组、训练组(P < 0.05或P < 0.01),训练组上斜方肌厚度大于冲击波组(P < 0.05)。 2.6 各组血流动力学指标比较 见表4。 与干预前比较,冲击波组、联合组干预1,4周后的颈横动脉上升段收缩期峰值速度升高(P < 0.05)、阻力指数降低(P < 0.05),训练组干预4周后的1,4周后的颈横动脉上升段收缩期峰值速度升高(P < 0.05)、阻力指数降低(P < 0.05)。 干预前,3组间颈横动脉上升段收缩期峰值速度与阻力指数比较差异均无显著性意义(P > 0.05)。干预1,4周后,联合组颈横动脉上升段收缩期峰值速度高于冲击波组、训练组(P < 0.05或P < 0.01),阻"
| [1] KAZEMINASAB S, NEJADGHADERI SA, AMIRI P, et al. Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord. 2022;23(1):26. [2] SCHUBINER H, LOWRY WJ, HEULE M, et al. Application of a Clinical Approach to Diagnosing Primary Pain: Prevalence and Correlates of Primary Back and Neck Pain in a Community Physiatry Clinic. J Pain. 2024;25(3):672-681. [3] CASTELLINI G, PILLASTRINI P, VANTI C, et al. Some conservative interventions are more effective than others for people with chronic non-specific neck pain: a systematic review and network meta-analysis. J Physiother. 2022;68(4):244-254. [4] CANKURTARAN D, AYKIN YIĞMAN Z, GÜZEL Ş, et al. The importance of myofascial trigger points in chronic neck pain: An ultrasonography preliminary study. PM R. 2023;15(8):954-964. [5] OPARA M, KOZINC Ž. Which muscles exhibit increased stiffness in people with chronic neck pain? A systematic review with meta-analysis. Front Sports Act Living. 2023;5:1172514. [6] SIMONS DG. New views of myofascial trigger points: etiology and diagnosis. Arch Phys Med Rehabil. 2008;89(1):157-159. [7] JIANG F, YU S, SU H, et al. Assessment of the effects of ischaemia/ hypoxia on angiogenesis in rat myofascial trigger points using colour Doppler flow imaging. PeerJ. 2020;8:e10481. [8] POTENTE M, GERHARDT H, CARMELIET P. Basic and therapeutic aspects of angiogenesis. Cell. 2011;146(6):873-887. [9] 葛云龙,刘亚梅,张金燕,等.放散式冲击波结合针灸治疗对老年慢性颈痛患者颈椎功能和生活质量的影响[J].中国老年学杂志, 2023,43(15):3713-3716. [10] KARTALOGLU IF, KUS AA. Evaluation of Radial Extracorporeal Shock Wave Therapy on Treatment-Resistant Trigger Points Using Sonographic Shear Wave Elastography. J Coll Physicians Surg Pak. 2023;33(10):1159-1164. [11] KIM HA, KWON OY, YI CH, et al. Altered muscle recruitment patterns during isometric shoulder abduction in individuals with chronic upper trapezius pain: a cross sectional study. BMC Musculoskelet Disord. 2022;23(1):1131. [12] DEMIR BENLI M, TATARI H, BALCı A, et al. A comparison between the efficacy of eccentric exercise and extracorporeal shock wave therapy on tendon thickness, vascularity, and elasticity in Achilles tendinopathy: A randomized controlled trial. Turk J Phys Med Rehabil. 2022;68(3): 372-380. [13] YALÇıN Ü. Comparison of the effects of extracorporeal shockwave treatment with kinesiological taping treatments added to exercise treatment in myofascial pain syndrome. J Back Musculoskelet Rehabil. 2021;34(4):623-630. [14] LEE YM, KOO DK, KWON JW. The efficacy of sling exercise combined with extracorporeal shock wave on office workers with chronic neck pain. Medicine (Baltimore). 2023;102(23):e33940. [15] 王雪强, 王于领, 张志杰,等.运动疗法治疗颈痛的中国专家共识[J].上海体育学院学报,2020,44(1):59-69. [16] 王强,孙国栋,马金健,等.基于生物力学及本体感觉分析探讨运动控制训练在颈椎病防治中的应用[J].辽宁中医药大学学报, 2020,22(11):204-209. [17] PRICE J, RUSHTON A, TYROS I, et al. Effectiveness and optimal dosage of exercise training for chronic non-specific neck pain: A systematic review with a narrative synthesis. PLoS One. 2020;15(6):e0234511. [18] GHADERI F, JAFARABADI MA, JAVANSHIR K. The clinical and EMG assessment of the effects of stabilization exercise on nonspecific chronic neck pain: A randomized controlled trial. J Back Musculoskelet Rehabil. 2017;30(2):211-219. [19] BLANPIED PR, GROSS AR, ELLIOTT JM, et al. Neck Pain: Revision 2017. J Orthop Sports Phys Ther. 2017;47(7):A1-a83. [20] SIMONS DG, TRAVELL JG, SIMONS LS. Protecting the ozone layer. Arch Phys Med Rehabil. 1990;71(1):64. [21] 中华医学会物理医学与康复学分会,肌肉骨骼疾病体外冲击波治疗专家共识组.肌肉骨骼疾病体外冲击波治疗专家共识[J].中华物理医学与康复杂志,2019,41(7):481-487. [22] SIKDAR S, SHAH JP, GEBREAB T, et al. Novel applications of ultrasound technology to visualize and characterize myofascial trigger points and surrounding soft tissue. Arch Phys Med Rehabil. 2009;90(11):1829-1838. [23] SIKDAR S, ORTIZ R, GEBREAB T, et al. Understanding the vascular environment of myofascial trigger points using ultrasonic imaging and computational modeling. Annu Int Conf IEEE Eng Med Biol Soc. 2010;2010:5302-5305. [24] GOLLMANN-TEPEKÖYLÜ C, PÖLZL L, GRABER M, et al. miR-19a-3p containing exosomes improve function of ischaemic myocardium upon shock wave therapy. Cardiovasc Res. 2020;116(6):1226-1236. [25] MODENA DAO, SOARES CD, CANDIDO EC, et al. Effect of extracorporeal shock waves on inflammation and angiogenesis of integumentary tissue in obese individuals: stimulating repair and regeneration. Lasers Med Sci. 2022;37(2):1289-1297. [26] SOPEL M, KUBERKA I, SZCZUKA I, et al. Can Shockwave Treatment Elicit a Molecular Response to Enhance Clinical Outcomes in Pressure Ulcers? The SHOck Waves in wouNds Project. Biomedicines. 2024;12(2):359. [27] PARK KD, LEE WY, PARK MH, et al. High-versus low-energy extracorporeal shock-wave therapy for myofascial pain syndrome of upper trapezius: A prospective randomized single blinded pilot study. Medicine (Baltimore). 2018;97(28):e11432. [28] KIMURA S, KAWAMORITA N, KIKUCHI Y, et al. Author Correction: Low-energy shock wave therapy ameliorates ischemic-induced overactive bladder in a rat model. Sci Rep. 2023;13(1):12001. [29] 程志祥,樊肖冲,冯智英,等.体外冲击波疗法临床应用中国疼痛学专家共识(2023版)[J].中华疼痛学杂志,2023,19(2):220-235. [30] VOSS MW, ERICKSON KI, PRAKASH RS, et al. Neurobiological markers of exercise-related brain plasticity in older adults. Brain Behav Immun. 2013;28:90-99. [31] KIM HB, SEO MW, JUNG HC. Effects of Aerobic vs. Resistance Exercise on Vascular Function and Vascular Endothelial Growth Factor in Older Women. Healthcare (Basel). 2023;11(18):2479. [32] WU T, WANG D, ZHANG X, et al. Comparison of pain relief and limb function improvement after extracorporeal shock wave therapy and thermomagnetic therapy in the treatment of low back pain. Pak J Med Sci. 2023;39(1):268-273. [33] GUZMÁN-PAVÓN MJ, CAVERO-REDONDO I, MARTÍNEZ-VIZCAÍNO V, et al. Effect of Physical Exercise Programs on Myofascial Trigger Points-Related Dysfunctions: A Systematic Review and Meta-analysis. Pain Med. 2020;21(11):2986-2996. [34] KIM KL, PARK GY, MOON YS, et al. The effects of treatment using polydeoxyribonucleotide through extracorporeal shock wave therapy: synergic regeneration effects on atrophied calf muscles in immobilized rabbits. Ann Transl Med. 2022;10(16):853. [35] FARRELL SF, DE ZOETE RMJ, CABOT PJ, et al. Systemic inflammatory markers in neck pain: A systematic review with meta-analysis. Eur J Pain. 2020;24(9):1666-1686. [36] PINTO EM, NEVES JR, LARANJEIRA M, et al. The importance of inflammatory biomarkers in non-specific acute and chronic low back pain: a systematic review. Eur Spine J. 2023;32(9):3230-3244. [37] HSIAO CC, HOU YS, LIU YH, et al. Combined Melatonin and Extracorporeal Shock Wave Therapy Enhances Podocyte Protection and Ameliorates Kidney Function in a Diabetic Nephropathy Rat Model. Antioxidants (Basel). 2021;10(5):733. [38] CHEN L, QING A, ZHU T, et al. Effect and safety of extracorporeal shockwave therapy for postherpetic neuralgia: A randomized single-blind clinical study. Front Neurol. 2022;13: 948024. [39] SCHEFFER DDL, LATINI A. Exercise-induced immune system response: Anti-inflammatory status on peripheral and central organs. Biochim Biophys Acta Mol Basis Dis. 2020;1866(10):165823. [40] BONILLA-BARBA L, FLORENCIO LL, RODRÍGUEZ-JIMÉNEZ J, et al. Women with mechanical neck pain exhibit increased activation of their superficial neck extensors when performing the cranio-cervical flexion test. Musculoskelet Sci Pract. 2020;49:102222. [41] EZZATI K, KHANI S, MOLADOUST H, et al. Comparing muscle thickness and function in healthy people and subjects with upper trapezius myofascial pain syndrome using ultrasonography. J Bodyw Mov Ther. 2021;26:253-256. [42] PARK SH, LEE MM. Effects of Lower Trapezius Strengthening Exercises on Pain, Dysfunction, Posture Alignment, Muscle Thickness and Contraction Rate in Patients with Neck Pain; Randomized Controlled Trial. Med Sci Monit. 2020;26:e920208. [43] DE LA CORTE-RODRIGUEZ H, ROMAN-BELMONTE JM, RESINO-LUIS C, et al. The Role of Physical Exercise in Chronic Musculoskeletal Pain: Best Medicine-A Narrative Review. Healthcare (Basel). 2024;12(2):242. [44] LEE YJ, MOON YS, KWON DR, et al. Polydeoxyribonucleotide and Shock Wave Therapy Sequence Efficacy in Regenerating Immobilized Rabbit Calf Muscles. Int J Mol Sci. 2023;24(16):12820. [45] ZISSLER A, STEINBACHER P, ZIMMERMANN R, et al. Extracorporeal Shock Wave Therapy Accelerates Regeneration After Acute Skeletal Muscle Injury. Am J Sports Med. 2017;45(3):676-684. [46] MANAFNEZHAD J, SALAHZADEH Z, SALIMI M, et al. The effects of shock wave and dry needling on active trigger points of upper trapezius muscle in patients with non-specific neck pain: A randomized clinical trial. J Back Musculoskelet Rehabil. 2019;32(5):811-818. [47] RAHBAR M, SAMANDARIAN M, SALEKZAMANI Y, et al. Effectiveness of extracorporeal shock wave therapy versus standard care in the treatment of neck and upper back myofascial pain: a single blinded randomised clinical trial. Clin Rehabil. 2021;35(1):102-113. [48] KHOSROKIANI Z, LETAFATKAR A, GLADIN A. Lumbar motor control training as a complementary treatment for chronic neck pain: A randomized controlled trial. Clin Rehabil. 2022;36(1): 99-112. [49] LAFRANCE S, OUELLET P, ALAOUI R, et al. Motor Control Exercises Compared to Strengthening Exercises for Upper- and Lower-Extremity Musculoskeletal Disorders: A Systematic Review With Meta-Analyses of Randomized Controlled Trials. Phys Ther. 2021; 101(7):pzab072. [50] HIRAOKA Y, OCHIAI N, NARITA M, et al. Efficacy of radial shock wave therapy on rat models of adjuvant arthritis. J Orthop Sci. 2023;29(6): 1513-1520. [51] YOON SY, KIM YW, SHIN IS, et al. Does the Type of Extracorporeal Shock Therapy Influence Treatment Effectiveness in Lateral Epicondylitis? A Systematic Review and Meta-analysis. Clin Orthop Relat Res. 2020; 478(10):2324-2339. [52] MINGWANG Z, ZHUANLI D, CHANGHAO W, et al. Efficacy and safety of extracorporeal shock wave therapy combined with sodium hyaluronate in treatment of knee osteoarthritis: a systematic review and Meta-analysis. J Tradit Chin Med. 2024;44(2):243-250. [53] SIMPLICIO CL, PURITA J, MURRELL W, et al. Extracorporeal shock wave therapy mechanisms in musculoskeletal regenerative medicine. J Clin Orthop Trauma. 2020;11(Suppl 3):S309-s318. [54] KAMI K, TAJIMA F, SENBA E. Brain Mechanisms of Exercise-Induced Hypoalgesia: To Find a Way Out from “Fear-Avoidance Belief”. Int J Mol Sci. 2022;23(5):2886. [55] MIDDLEBROOK N, RUSHTON AB, HENEGHAN NR, et al. Measures of central sensitisation and their measurement properties in the adult musculoskeletal trauma population: a protocol for a systematic review and data synthesis. BMJ Open. 2019;9(3):e023204. [56] NIJS J, LEYSEN L, VANLAUWE J, et al. Treatment of central sensitization in patients with chronic pain: time for change? Expert Opin Pharmacother. 2019;20(16):1961-1970. |
| [1] | Zhang Di, Zhao Jun, Ma Guangyue, Sun Hui, Jiang Rong. Mechanism of depression-like behavior in chronic social defeat stress mice based on high-throughput sequencing [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1139-1146. |
| [2] | Sun Yajie, Zhao Xinchen, Bo Shuangling. Spatiotemporal expression of bone morphologic protein 7 in mouse kidney development [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1156-1161. |
| [3] | Liu Yu, Lei Senlin, Zhou Jintao, Liu Hui, Li Xianhui. Mechanisms by which aerobic and resistance exercises improve obesity-related cognitive impairment [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1171-1183. |
| [4] | Yu Huifen, Mo Licun, Cheng Leping. The position and role of 5-hydroxytryptamine in the repair of tissue injury [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1196-1206. |
| [5] | Wang Zhengye, Liu Wanlin, Zhao Zhenqun. Advance in the mechanisms underlying miRNAs in steroid-induced osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1207-1214. |
| [6] | Bu Yangyang, Ning Xinli, Zhao Chen. Intra-articular injections for the treatment of osteoarthritis of the temporomandibular joint: different drugs with multiple combined treatment options [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1215-1224. |
| [7] | Wen Fan, Xiang Yang, Zhu Huan, Tuo Yanfang, Li Feng. Exercise improves microvascular function in patients with type 2 diabetes [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1225-1235. |
| [8] | Liu Xinyue, Li Chunnian, Li Yizhuo, Xu Shifang. Regeneration and repair of oral alveolar bone defects [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1247-1259. |
| [9] | Leng Xiaoxuan, Zhao Yuxin, Liu Xihua. Effects of different neuromodulatory stimulation modalities on non-motor symptoms in Parkinson’s patients: a network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1282-1293. |
| [10] | Wen Xiaolong, Weng Xiquan, Feng Yao, Cao Wenyan, Liu Yuqian, Wang Haitao. Effects of inflammation on serum hepcidin and iron metabolism related parameters in patients with type 2 diabetes mellitus: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1294-1301. |
| [11] | Yang Zeyu, Zhi Liang, Wang Jia, Zhang Jingyi, Zhang Qingfang, Wang Yulong, Long Jianjun. A visualized analysis of research hotspots in high-frequency repetitive transcranial magnetic stimulation from the macroscopic perspective [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1320-1330. |
| [12] | Yang Zhijie, Zhao Rui, Yang Haolin, Li Xiaoyun, Li Yangbo, Huang Jiachun, Lin Yanping, Wan Lei, HuangHongxing. Postmenopausal osteoporosis: predictive values of muscle mass, grip strength, and appendicular skeletal muscle index [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1073-1080. |
| [13] | Yin Yongcheng, Zhao Xiangrui, Yang Zhijie, Li Zheng, Li Fang, Ning Bin. Effect and mechanism of peroxiredoxin 1 in microglial inflammation after spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1106-1113. |
| [14] | Zhang Jiuxuan, Zhang Jinnan, Sui Xiaofan, Pei Xiaxia, Wei Jianhong, Su Qiang, Li Tian. Effects of ammonia poisoning on cognitive behavior and hippocampal synaptic damage in mice [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1122-1128. |
| [15] | Chen Yixian, Chen Chen, Lu Liheng, Tang Jinpeng, Yu Xiaowei. Triptolide in the treatment of osteoarthritis: network pharmacology analysis and animal model validation [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 805-815. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||