Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (5): 1184-1195.doi: 10.12307/2026.020
Previous Articles Next Articles
Acute effects of blood flow restriction in low-intensity resistance training on endothelial function-related inflammatory factors
Tao Yunfei1, Peng Li1, 2
- 1School of Physical Education, 2Key Laboratory of Physical Fitness Evaluation and Motor Function Monitoring, Southwest University, Chongqing 400715, China
-
Received:2024-10-28Accepted:2025-01-17Online:2026-02-18Published:2025-06-25 -
Contact:Peng Li, PhD, Professor, School of Physical Education, Southwest University, Chongqing 400715, China; Key Laboratory of Physical Fitness Evaluation and Motor Function Monitoring, Southwest University, Chongqing 400715, China -
About author:Tao Yunfei, Master candidate, School of Physical Education, Southwest University, Chongqing 400715, China -
Supported by:the National Social Science General Foundation, No. 21BTY092 (to PL); Southwest University Graduate Student Research and Innovation Program, No. SWUS23036 (to TYF)
CLC Number:
Cite this article
Tao Yunfei, Peng Li. Acute effects of blood flow restriction in low-intensity resistance training on endothelial function-related inflammatory factors[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1184-1195.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
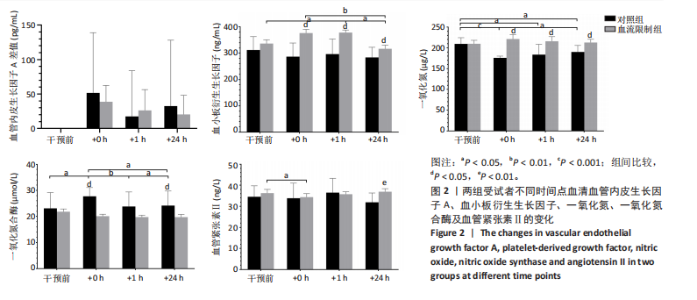
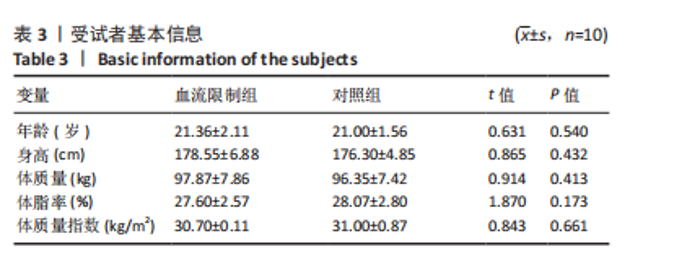
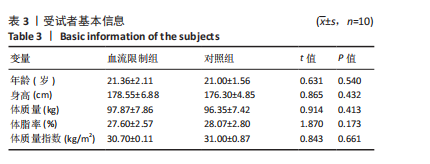
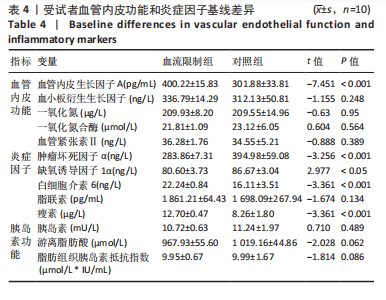
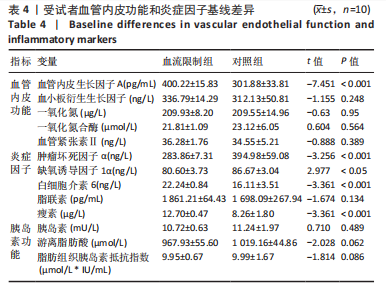
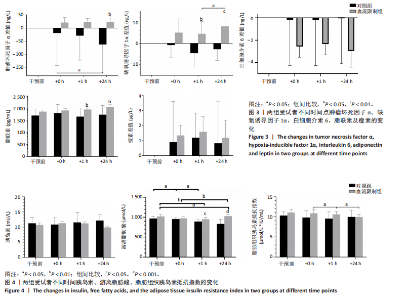
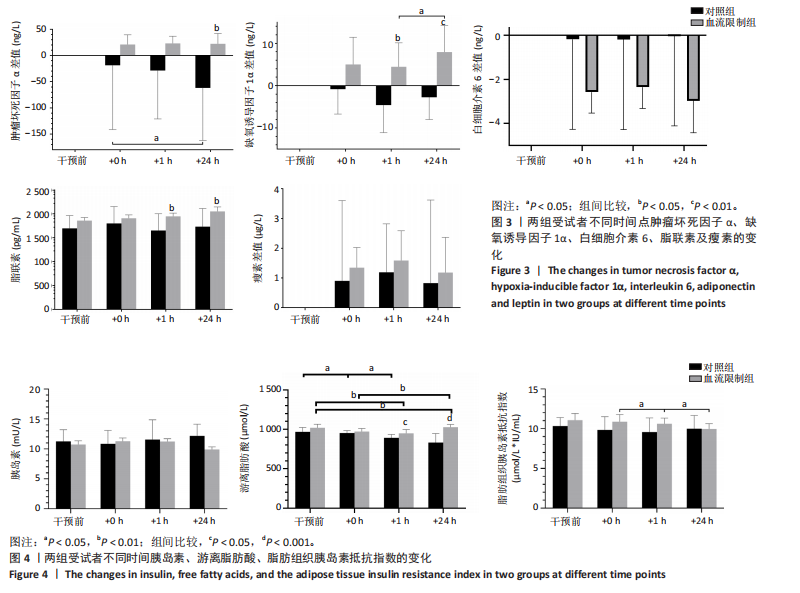
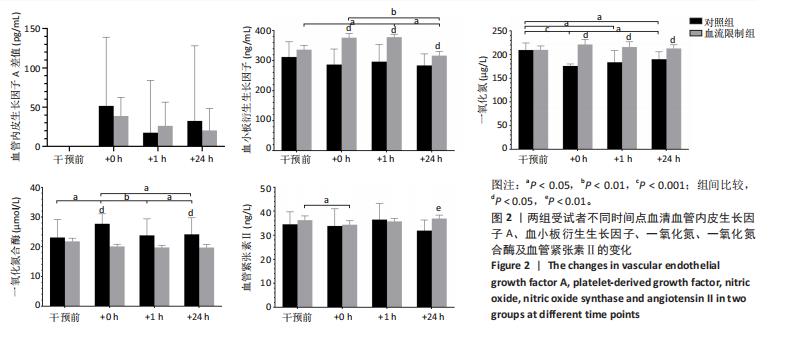
2.4.1 血管内皮生长因子A 经过双因素重复测量方差分析发现,组间因素(血流限制组和对照组)(F=0.062,P > 0.05,η2P=0.004)与组内因素(不同时点)(F=0.814,P > 0.05,η2P=0.055)及其两种因素的交互作用(F=0.201,P > 0.05,η2P=0.014)对血液血管内皮生长因子A质量浓度的影响不存在统计学意义。 2.4.2 血小板衍生生长因子 经过双因素重复测量方差分析发现,组间因素(F=32.42,P < 0.001,η2P=0.698)与组内因素(F=3.415,P < 0.05,η2P=0.196)及其两种因素的交互作用(F=3.519,P < 0.05,η2P=0.201)对血液血小板衍生生长因子质量浓度的影响均存在统计学意义,因此进行简单效应分析。与运动前相比,血流限制组血小板衍生生长因子质量浓度在运动后1 h显著增加(P < 0.05),与运动后即刻和运动后1 h相比,运动后24 h均显著下降(P < 0.05)。相较于对照组,血流限制组运动后血小板衍生生长因子的质量浓度显著增高[运动后即刻(P < 0.001)、运动后1 h(P < 0.01)和运动后24 h(P < 0.05)]。 2.4.3 一氧化氮 经过双因素重复测量方差分析发现,组内因素对血液一氧化氮质量浓度的影响不存在统计学差异(F=2.174,P > 0.05,η2P=0.352),组间因素(F=55.729,P < 0.001,η2P=0.799)与组间和组内因素的交互作用(F=9.787,P < 0.01,η2P=0.710)对一氧化氮质量浓度的影响均存在统计学意义,因此进行简单效应分析。血流限制组一氧化氮质量浓度变化在各时点不存在显著变化,但对照组在运动干预后各时间点均显著下降(P < 0.05),且运动后24 h相较于运动后即刻显著增加(P < 0.05)。血流限制组一氧化氮质量浓度在运动后即刻(P < 0.001)、运动后1 h (P < 0.01)、运动后24 h(P < 0.05)均显著高于对照组。 2.4.4 一氧化氮合酶 经过双因素重复测量方差分析发现,组内因素对血液一氧化氮合酶浓度的影响不存在统计学差异(F=2.418,P > 0.05,η2P=0.377),组间因素(F=16.574,P < 0.01,η2P=0.542)与组间和组内因素的交互作用(F=3.394 7,P < 0.05,η2P=0.459)对一氧化氮合酶浓度的影响均存在统计学意义,因此进行简单效应分析。血流限制组一氧化氮合酶浓度变化在各时点不存在显著变化,但对照组相较于运动前,一氧化氮合酶浓度在运动后即刻显著增加(P < 0.05),且相较于运动后即刻,运动后1 h(P < 0.01)和运动后24 h(P < 0.05)均显著降低,相较于运动后1 h,运动后24 h显著增加(P < 0.05)。对照组一氧化氮合酶浓度在运动后即刻和运动后24 h均显著高于血流限制组(P < 0.05)。 2.4.5 血管紧张素Ⅱ 经过双因素重复测量方差分析发现,组间因素对血液血管紧张素Ⅱ质量浓度的影响存在统计学差异(F=6.046,P < 0.05,η2P=0.302),组内因素(F=0.582,P > 0.05,η2P=0.040)与组间和组内因素的交互作用(F=1.061,P > 0.05,η2P=0.070)对血管紧张素Ⅱ质量浓度的影响均不存在统计学意义,因此进行事后检验分析。运动后24 h血流限制组血管紧张素Ⅱ质量浓度显著高于对照组(P < 0.01),相较于运动前,血流限制组在运动后即刻显著降低(P < 0.05)。 2.5 血流限制对受试者炎症标志物水平的急性影响 见图3。 2.5.1 肿瘤坏死因子α 经过双因素重复测量方差分析发现,组间因素(F=2.945,P > 0.05,η2P=0.174),组内因素(F=1.218,P > 0.05,η2P=0.080)及其交互作用(F=1.303,P > 0.05,η2P=0.085)对血液肿瘤坏死因子α质量浓度的影响均不存在统计学意义,因此进行事后检验分析。血流限制组肿瘤坏死因子α质量浓度在各时点不存在显著变化,在运动后24 h显著高于对照组(P < 0.05)。相较于运动后即刻,对照组在运动后24 h肿瘤坏死因子α质量浓度显著下降(P < 0.05)。 2.5.2 缺氧诱导因子1α 经过双因素重复测量方差分析发现,组间(F=11.953,P < 0.001,η2P=0.461)和组内因素(F=4.735,P < 0.05,η2P=0.421)对血液缺氧诱导因子1α质量浓度的影响存在统计学差异,但组间和组内因素的交互作用(F=0.971,P > 0.05,η2P=0.130)对缺氧诱导因子1α质量浓度的影响均不存在统计学意义,因此进行事后检验分析。相较于运动后1 h,血流限制组缺氧诱导因子1α质量浓度在运动后24 h显著增加(P < 0.05),相较于对照组,血流限制组在运动后1 h(P < 0.05)和运动后24 h(P < 0.01)缺氧诱导因子1α质量浓度显著增加。 2.5.3 白细胞介素6 经过双因素重复测量方差分析发现,组间因素(F=2.401,P > 0.05,η2P=0.146),组内因素(F=0.005,P > 0.05,η2P=0.000)及其交互作用(F=0.002,P > 0.05,η2P=0.000)对血液白细胞介素6质量浓度的影响均不存在统计学意义。 2.5.4 脂联素 经过双因素重复测量方差分析发现,组间因素(F=17.706,P < 0.001,η2P=0.558)对血液脂联素质量浓度的影响存在统计学意义,组内因素(F=0.652,P > 0.05,η2P=0.044)及其交互作用(F=0.629,P > 0.05,η2P=0.043)对脂联素质量浓度的影响均不存在统计学意义,因此进行事后检验分析。相较于对照组,血流限制组在运动后1 h和24 h脂联素质量浓度显著增加(P < 0.05)。 2.5.5 瘦素 经过双因素重复测量方差分析发现,组间因素(F=0.277,P > 0.05,η2P=0.019),组内因素(F=0.419,P > 0.05,η2P=0.029)及其交互作用(F=0.006,P > 0.05,η2P=0.000)对血液瘦素浓度的影响均不存在统计学意义。 2.6 血流限制对胰岛素浓度和胰岛素抵抗指数的急性影响 见图4。 2.6.1 胰岛素 经过双因素重复测量方差分析发现,组间因素(F=1.853,P > 0.05,η2P=0.117),组内因素(F=0.201,P > 0.05,η2P=0.014)及其交互作用(F=1.874,P > 0.05,η2P=0.118)对血液胰岛素水平的影响均不存在统计学意义,因此进行事后检验分析。相较于对照组,血流限制组在运动干预后24 h血液胰岛素水平显著降低(P < 0.05)。 2.6.2 游离脂肪酸 经过双因素重复测量方差分析发现,组间因素(F=22.02,P < 0.05,η2P=0.611),组内因素(F=6.308,P < 0.05,η2P=0.311)及其交互作用(F=8.725,P < 0.05,η2P=0.384)对血液游离脂肪酸浓度的影响均存在统计学意义,因此进行简单效应分析。血流限制组在运动后对游离脂肪酸血液浓度的影响并无显著差异;相较于运动前和运动后即刻,对照组在运动后1h(P < 0.05)和运动后24 h显著降低(P < 0.01)。 2.6.3 脂肪组织胰岛素抵抗指数 经过双因素重复测量方差分析发现,组间因素(F=4.885,P < 0.05,η2P=0.196)对脂肪组织胰岛素抵抗指数的影响均存在统计学意义;组内因素(F=1.983,P > 0.05,η2P=0.248)及其交互作用(F=2.028,P > 0.05,η2P=0.253)对脂肪组织胰岛素抵抗指数的影响均不存在统计学意义,因此进行事后检验分析。相较于运动后即刻和运动后1 h,血流限制组脂肪组织胰岛素抵抗指数在运动后24 h显著降低(P < 0.05)。 2.7 不良事件 所有受试者运动测试过程均未发生运动损伤,动脉闭塞压组受试者运动过程也未发生组织受压损伤等不良事件。"
| [1] ABDELAAL M, LE ROUX CW, DOCHERTY NG. Morbidity and mortality associated with obesity. Ann Transl Med. 2017;5(7):161. [2] CHEN K, SHEN Z, GU W, et al. Prevalence of obesity and associated complications in China: A cross-sectional, real-world study in 15.8 million adults. Diabetes Obes Metab. 2023;25(11):3390-3399. [3] RODRÍGUEZ-HERNÁNDEZ H, SIMENTAL-MENDÍA LE, RODRÍGUEZ-RAMÍREZ G, et al. Obesity and inflammation: epidemiology, risk factors, and markers of inflammation. Int J Endocrinol. 2013;2013:678159. [4] GIANOPOULOS I, MANTZOROS CS, DASKALOPOULOU SS. Adiponectin and Adiponectin Receptors in Atherosclerosis. Endocr Rev. 2025;46(1): 1-25. [5] BRAGA TIBAES JR, BARRETO SILVA MI, WOLLIN B, et al. Sex differences in systemic inflammation and immune function in diet-induced obesity rodent models: A systematic review. Obes Rev. 2024;25(3):e13665. [6] GESTA S, TSENG YH, KAHN CR. Developmental origin of fat: tracking obesity to its source. Cell. 2007;131(2):242-256. [7] GREENBERG AS, OBIN MS. Obesity and the role of adipose tissue in inflammation and metabolism. Am J Clin Nutr. 2006;83(2):461S-465S. [8] DUDLEY AC, GRIFFIOEN AW. Pathological angiogenesis: mechanisms and therapeutic strategies. Angiogenesis. 2023;26(3):313-347. [9] DHANANJAYAN R, KOUNDINYA KSS, MALATI T, et al. Endothelial Dysfunction in Type 2 Diabetes Mellitus. Indian J Clin Biochem. 2016; 31(4):372-379. [10] BULLÓ M, GARCÍA-LORDA P, MEGIAS I, et al. Systemic inflammation, adipose tissue tumor necrosis factor, and leptin expression. Obes Res. 2003;11(4):525-531. [11] HOTAMISLIGIL GS, SHARGILL NS, SPIEGELMAN BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science. 1993;259(5091):87-91. [12] AGHAMOHAMMADZADEH R, GREENSTEIN AS, YADAV R, et al. J Am Coll Cardiol. 2013;62(2):128-135. [13] ANTONIADES C, TOUSOULIS D, VAVLUKIS M, et al. Perivascular adipose tissue as a source of therapeutic targets and clinical biomarkers. Eur Heart J. 2023;44(38):3827-3844. [14] STRASSER B, ARVANDI M, SIEBERT U. Resistance training, visceral obesity and inflammatory response: a review of the evidence.Obes Rev. 2012;13(7):578-591. [15] STRASSER B, SIEBERT U, SCHOBERSBERGER W. Resistance Training in the Treatment of the Metabolic Syndrome. Sports Med. 2010;40(5): 397-415. [16] DIAS I, FARINATTI P, DE SOUZA MG, et al. Effects of Resistance Training on Obese Adolescents. Med Sci Sports Exerc. 2015;47(12):2636-2644. [17] GONZALES JU,THOMPSON BC, THISTLETHWAITE JR, et al.Association between exercise hemodynamics and changes in local vascular function following acute exercise. Appl Physiol Nutr Metab. 2011;36(1):137-144. [18] GOTO K, ISHII N, KIZUKA T, et al. Hormonal and metabolic responses to slow movement resistance exercise with different durations of concentric and eccentric actions. Eur J Appl Physiol. 2009;106(5):731-739. [19] TANIMOTO M, ISHII N. Effects of low-intensity resistance exercise with slow movement and tonic force generation on muscular function in young men. J Appl Physiol (1985). 2006;100(4):1150-1157. [20] AU JS, OIKAWA SY, MORTON RW, et al. Arterial Stiffness Is Reduced Regardless of Resistance Training Load in Young Men. Med Sci Sports Exerc. 2017;49(2):342-348. [21] SHIMIZU R, HOTTA K, YAMAMOTO S, et al. Low-intensity resistance training with blood flow restriction improves vascular endothelial function and peripheral blood circulation in healthy elderly people. Eur J Appl Physiol. 2016;116(4):749-757. [22] LARKIN KA, MACNEIL RG, DIRAIN M, et al. Blood Flow Restriction Enhances Post–Resistance Exercise Angiogenic Gene Expression.Med Sci Sports Exerc. 2012;44(11):2077-2083. [23] YANG Y, WANG D, ZHANG C, et al. Piezo1 mediates endothelial atherogenic inflammatory responses via regulation of YAP/TAZ activation. Hum Cell. 2022;35(1):51-62. [24] ALBARRÁN-JUÁREZ J, IRING A, WANG S, et al. Piezo1 and Gq/G11 promote endothelial inflammation depending on flow pattern and integrin activation. J Exp Med. 2018;215(10):2655-2672. [25] 时文霞, 谢军, 何玉凤, 等. 血管内皮功能障碍运动干预的血流剪切力作用机制研究进展[J]. 中国体育科技,2024,60(3):51-64. [26] LV Y, KIM K, SHENG Y, et al. YAP Controls Endothelial Activation and Vascular Inflammation Through TRAF6. Circ Res. 2018;123(1):43-56. [27] [No authors listed]. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995;854:1-452. [28] BOK D, RAKOVAC M, FOSTER C. An Examination and Critique of Subjective Methods to Determine Exercise Intensity: The Talk Test, Feeling Scale, and Rating of Perceived Exertion. Sports Med. 2022; 52(9):2085-2109. [29] GARBER CE, BLISSMER B, DESCHENES MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise]. Med Sci Sports Exerc. 2011;43(7):1334-1359. [30] HASS CJ, FEIGENBAUM MS, FRANKLIN BA.Prescription of resistance training for healthy populations. Sports Med. 2001;31(14):953-964. [31] GRAY SM, CUOMO AM, PROPPE CE, et al. Effects of Sex and Cuff Pressure on Physiological Responses during Blood Flow Restriction Resistance Exercise in Young Adults. Med Sci Sports Exerc. 2023;55(5): 920-931. [32] 魏佳, 李博, 冯连世, 等. 血流限制训练的方法学因素及潜在安全性问题[J].中国体育科技,2019,55(3):3-12. [33] THEOFILIS P, SAGRIS M, OIKONOMOU E, et al. Inflammatory Mechanisms Contributing to Endothelial Dysfunction. Biomedicines. 2021;9(7):781. [34] ANGELO LS, KURZROCK R.Vascular Endothelial Growth Factor and Its Relationship to Inflammatory Mediators. Clin Cancer Res. 2007; 13(10):2825-2830. [35] ZHOU X, YU D, SUN X, et al. Hypoxia-inducible Factor-1α in Diabetic Foot Ulcers: Plain but Not Simple. Gene Expression. 2023;22(4): 306-320. [36] DEL ROSSO S, BARAQUET ML, BARALE A, et al. Long-term effects of different exercise training modes on cytokines and adipokines in individuals with overweight/obesity and cardiometabolic diseases: A systematic review, meta-analysis, and meta-regression of randomized controlled trials. Obes Rev. 2023;24(6):e13564. [37] 陈巍, 李娟, 陈庆合, 等. 抗阻训练中运动肌血流限制对肥胖者体成分及胰岛素敏感度的影响[J]. 中国运动医学杂志,2010,29(6): 646-649. [38] CHUA MT, SIM A, BURNS SF. Acute and Chronic Effects of Blood Flow Restricted High-Intensity Interval Training: A Systematic Review. Sports Med Open. 2022;8(1):122. [39] MCINTOSH MC, ANGLIN DA, ROBINSON AT, et al. Making the case for resistance training in improving vascular function and skeletal muscle capillarization. Front Physiol. 2024;15:1338507. [40] KÖNIGSTEIN K, DIPLA K, ZAFEIRIDIS A. Training the Vessels: Molecular and Clinical Effects of Exercise on Vascular Health—A Narrative Review.Cells. 2023;12(21):2544. [41] HALBERG N, KHAN T, TRUJILLO ME, et al. Hypoxia-inducible factor 1alpha induces fibrosis and insulin resistance in white adipose tissue.Mol Cell Biol. 2009;29(16):4467-4483. [42] KAPIL V, KHAMBATA RS, JONES DA, et al. The Noncanonical Pathway for In Vivo Nitric Oxide Generation: The Nitrate-Nitrite-Nitric Oxide Pathway. Pharmacol Rev. 2020;72(3):692-766. [43] TEJERO J, SHIVA S, GLADWIN MT. Sources of Vascular Nitric Oxide and Reactive Oxygen Species and Their Regulation. Physiol Rev. 2019; 99(1):311-379. [44] THEOFILIS P, SAGRIS M, OIKONOMOU E, et al. Inflammatory Mechanisms Contributing to Endothelial Dysfunction. Biomedicines. 2021;9(7):781. [45] 陈晓可, 历建宇, 陈超凡, 等. 不同运动类型对超重或肥胖人群炎症因子影响的网状Meta分析[J]. 中国循证医学杂志,2024,24(5): 565-571. [46] MALKOV MI, LEE CT, TAYLOR CT. Regulation of the Hypoxia-Inducible Factor (HIF) by Pro-Inflammatory Cytokines. Cells. 2021;10(9):2340. [47] NIJHAWANS P, BEHL T, BHARDWAJ S.Angiogenesis in obesity. Biomed Pharmacother. 2020;126:110103. [48] PETERSEN MC, SHULMAN GI. Mechanisms of Insulin Action and Insulin Resistance. Physiol Rev. 2018;98(4):2133-2223. [49] ZATTERALE F, LONGO M, NADERI J, et al. Chronic Adipose Tissue Inflammation Linking Obesity to Insulin Resistance and Type 2 Diabetes.Front Physiol. 2020;10:1607. [50] 张小凡,叶新华.抗阻运动对骨骼肌胰岛素抵抗的影响机制[J]. 中华糖尿病杂志,2020,12(7):558-561. [51] SEMNANI-AZAD Z, CONNELLY PW, BAZINET RP, et al. Adipose Tissue Insulin Resistance Is Longitudinally Associated With Adipose Tissue Dysfunction, Circulating Lipids, and Dysglycemia: The PROMISE Cohort. Diabetes Care. 2021;44(7):1682-1691. [52] FERLITO JV, ROLNICK N, FERLITO MV, et al. Acute effect of low-load resistance exercise with blood flow restriction on oxidative stress biomarkers: A systematic review and meta-analysis. PLoS One. 2023; 18(4):e0283237. [53] CHRISTIANSEN D, BISHOP DJ. Aerobic-interval exercise with blood flow restriction potentiates early markers of metabolic health in man. Acta Physiol (Oxf). 2022;234(2):e13769. [54] SU Y, WANG F, WANG M, et al. Effects of blood flow restriction training on muscle fitness and cardiovascular risk of obese college students. Front Physiol. 2024;14:1252052. |
| [1] | Liu Yu, Lei Senlin, Zhou Jintao, Liu Hui, Li Xianhui. Mechanisms by which aerobic and resistance exercises improve obesity-related cognitive impairment [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1171-1183. |
| [2] | Zhou Jian, Zhang Tao, Zhou Weili, Zhao Xingcheng, Wang Jun, Shen Jie, Qian Li, Lu Ming. Effects of resistance training on quadriceps mass and knee joint function in patients with osteoporosis and sarcopenia [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1081-1088. |
| [3] | Zhang Zixian, Xu Youliang, Wu Shaokui, Wang Xiangying. Effects of blood flow restriction training combined with resistance training on muscle indicators in college athletes: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1705-1713. |
| [4] | Zhao Xiaoxuan, Liu Shuaiyi, Li Qi, Xing Zheng, Li Qingwen, Chu Xiaolei. Different exercise modalities promote functional recovery after peripheral nerve injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1248-1256. |
| [5] | Ji Long, Chen Ziyang, , Jin Pan, Kong Xiangkui, Pu Rui, . Lipophagy, exercise intervention and prevention and treatment of nonalcoholic fatty liver disease [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7611-7619. |
| [6] | Liu Chenchen, Liu Ruize, Bao Mengmeng, Fang Li, Cao Liquan, Wu Jiangbo. Blood flow restriction training intervention in the elderly with sarcopenic obesity [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6963-6970. |
| [7] | Liu Haowei, Tian Haodong, Huang Li, Yu Hanglin, Peng Li. Acute effects of blood flow restriction resistance exercise on serum metabolites in obese young men [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6249-6259. |
| [8] | Peng Yong, Hu Jiangping, Zhu Huan. Effects of low-load blood flow restriction exercise and high-intensity resistance exercise on the thigh microcirculation function of athletic young men [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(2): 393-401. |
| [9] | Zhang Dakuan, Li Yongjie, Han Libao, Liu Hongju, Liu Mengling, Fu Shenyu . Blood flow restriction training in the prevention and rehabilitation of foot and ankle injuries [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(12): 2553-2559. |
| [10] | Jia Yuexin, Tian Saisai, Qi Xiaohong, Zhang Suqin. Effects of 12 weeks of low-intensity resistance training combined with blood flow restriction training on body composition, muscle strength, and arterial elastic function in young adults [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(12): 2521-2527. |
| [11] | Yan Hailong, Huo Jiangtao, Zhou Wucheng, Bai Xuehua, Liang Yuanyuan. Application and mechanism of tissue flossing in sports and rehabilitation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 464-471. |
| [12] | Dong Zhaojing, Jiang Dongting, Luo Xinjian, Yan Bing, Wang Yang, Ling Xiaoyu. Research progress on effects of wearable resistance training on lower limb movement ability [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(29): 4677-4684. |
| [13] | Kong Jianda, Xie Yingao, Ma Wen, Liu Youhan, Wang Qinglu. Mitochondrial dysfunction in Parkinson’s disease and the potential ameliorative effects of exercise [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(27): 4413-4420. |
| [14] | Kong Jianda, Xie Yingao, Chen Shijuan, Zhu Lei. Blood flow restriction training interventions for sarcopenia in older adults: biological mechanisms and proposed application protocols [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3743-3750. |
| [15] | Dong Kuan, Xu Chengli, Tian Jing, Xu Changchun. Effects of endurance training with blood flow restriction on aerobic capacity, lower limb muscle strength, and sports performance: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3766-3772. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||