Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (12): 2553-2559.doi: 10.12307/2025.377
Previous Articles Next Articles
Blood flow restriction training in the prevention and rehabilitation of foot and ankle injuries
Zhang Dakuan1, Li Yongjie1, Han Libao2, Liu Hongju1, Liu Mengling1, Fu Shenyu1
- 1Beijing Jishuitan Hospital Guizhou Hospital, Guiyang 550014, Guizhou Province, China; 2Sichuan Vocational College of Health and Rehabilitation, Zigong 643000, Sichuan Province, China
-
Received:2024-04-11Accepted:2024-06-15Online:2025-04-28Published:2024-09-10 -
Contact:Fu Shenyu, Rehabilitation therapist, Beijing Jishuitan Hospital Guizhou Hospital, Guiyang 550014, Guizhou Province, China -
About author:Zhang Dakuan, Master, Rehabilitation therapist in charge, Beijing Jishuitan Hospital Guizhou Hospital, Guiyang 550014, Guizhou Province, China -
Supported by:2022 Guizhou Orthopaedic Hospital Science and Technology Innovation Fund Project, No. GZGYCX[2022]14 (to ZDK); 2023 Guizhou Provincial Health and Health Commission Science and Technology Fund Project, No. gzwkj2023-124 (to FSY); 2023 Guizhou Provincial Science and Technology Support Program Project, No. [2023]general 179 (to LHJ)
CLC Number:
Cite this article
Zhang Dakuan, Li Yongjie, Han Libao, Liu Hongju, Liu Mengling, Fu Shenyu . Blood flow restriction training in the prevention and rehabilitation of foot and ankle injuries[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(12): 2553-2559.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
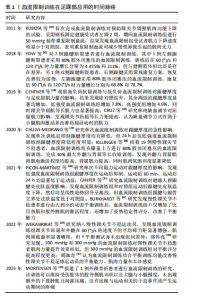
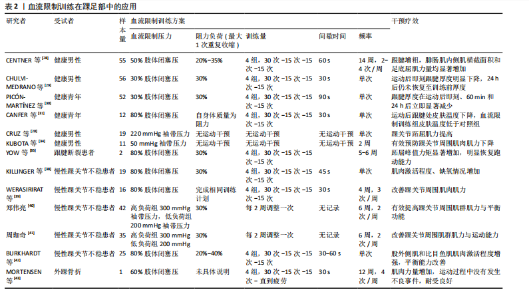
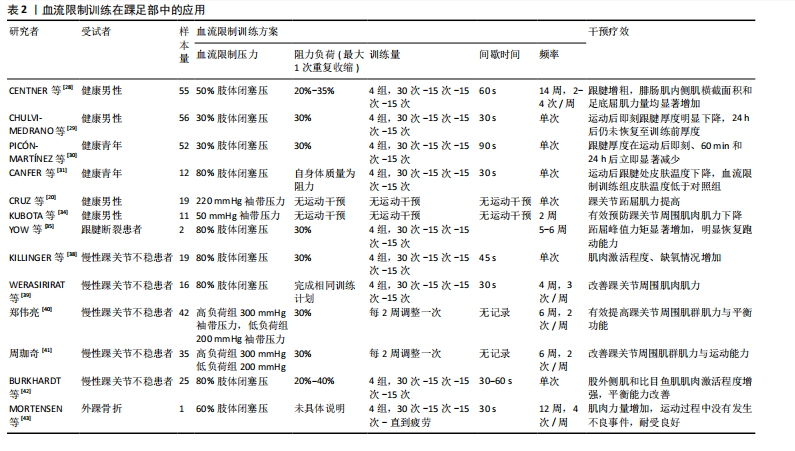
2.1 血流限制训练作用机制 各种生理机制被认为是导致血流限制训练中肌肉大小和力量增加的原因,尽管确切的机制尚不清楚,但普遍的共识认为肌肉变化是缺血缺氧和代谢物积累共同影响的结果,与其他相同强度的运动相比,血流限制训练导致更强的肌肉激活、合成代谢信号,从而加快机体恢复,产生最佳的运动效能[17]。 2.1.1 缺血机制 局部血管的间歇性加压可诱导组织和器官缺血再灌注损伤的内源性保护作用,缺血性调节会减少来自小直径神经纤维(特别是高阈值代谢伤害感受器亚型)的感觉反馈,使肌肉产生更大的神经传出信号并增强收缩力[18]。由于血流限制训练会加大血管壁的压力,使得动脉血液流动减缓、静脉血聚集增多,容易形成缺血缺氧环境[19],引起急性应激反应,然而这一现象背后的潜在机制仍然未知。缺血性机制可以通过增加来自中枢神经系统的运动放电来增强肌纤维的电化学活化和肌力[20]。另一方面,在进行运动时,Ⅰ型肌纤维首先被募集,随着肌肉疲劳程度的增加,Ⅱ型肌纤维再被募集参与活动,而在局部缺血时激活顺序将出现变化[21],当进行血流限制训练时,因运动肢体的血流受限而产生更大的代谢压力,将募集更多的Ⅱ型肌纤维参与运动。因此,缺血机制是通过降低Ⅱ型肌纤维萎缩程度来达到提高肌力的机制之一[22]。 2.1.2 代谢机制 细胞外液中代谢物不断累积,将压力通过液体刺激传导到肌纤维,从而驱动肌肉蛋白质合成哺乳动物雷帕霉素靶蛋白。哺乳动物雷帕霉素靶蛋白信号通路被认为是调控肌纤维生长的主要通路,它可以整合细胞内外信号进而生成性激素,通过改变哺乳动物雷帕霉素靶蛋白活性可以间接调整核醣体与mRNA的结合率。FRY等[23]认为低强度训练联合血流限制可增强哺乳动物雷帕霉素靶蛋白信号,肌肉蛋白合成由哺乳动物雷帕霉素靶蛋白通路通过S6蛋白激酶的磷酸化刺激产生,所以哺乳动物雷帕霉素靶蛋白信号通路的增强有助于解释血流限制训练后肌肉蛋白质合成水平的增强。YANAGISAWA等[24-25]通过测定腓肠肌内侧高能磷酸盐代谢评估血流限制的代谢应激水平,发现与低负荷无限制性运动相比,低负荷血流限制训练会给肌肉带来更大的代谢压力,使磷酸肌酸的消耗增加,肌肉内磷酸盐代谢产物和氢离子的积累会影响肌肉收缩能力,这也能解释为何血流限制训练能提高机体代谢进而改善肌力。SUGA等[26]研究认为,与低强度训练比较,低强度血流限制训练后肌肉pH值下降更明显,而低强度间歇血流限制训练时肌内pH值、快肌纤维募集程度与高强度训练表现相似。由此可见,血流限制训练可能会诱导较强的代谢应激,从而提高肌肉表现能力。 2.1.3 机械应力 机械应力也是刺激肌肉生长的重要因素,虽然低强度的机械应力不会促使肌力显著增加,但低强度训练联合血流限制却能达到显著增加肌力的效果,这个过程中代谢应激可能起到累加训练效果的作用,其中代谢应激起主导作用[27]。综上所述,机械应力与代谢应激应两者或许是相互协同的作用。虽有诸多研究讨论了血流限制训练的机制作用,但仍未完全阐述明了,今后还需不断深入研究。 2.2 血流限制训练在预防与康复踝足损伤中的应用 通过对国内外的相关文献进行回顾发现,在踝足部位的应用中,血流限制训练主要用于对健康人群的跟腱厚度和踝部肌力的研究,以及慢性踝关节不稳、跟腱断裂后、外踝骨折后[28-43]。血流限制训练在足踝部应用研究历史见表1。血流限制训练在足踝部的具体应用详见表2。"
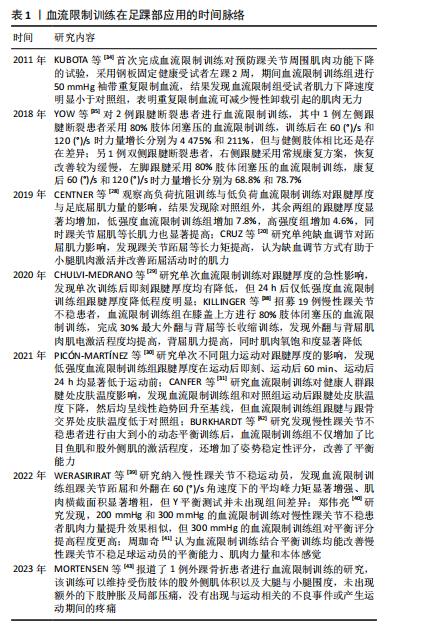

发现除对照组外,高负荷抗阻训练组、低负荷血流限制训练跟腱厚度显著均增加,同时踝关节屈肌等长肌力也显著提高。在急性单次干预中,CHULVI-MEDRANO等[29]研究单次低强度阻力训练与单次低强度血流限制训练对跟腱厚度的急性影响,低强度血流限制训练组在腿部腘窝下方进行30%肢体闭塞压,两组受试者进行3组15次重复的腿部跖屈,发现单次训练后即刻两组跟腱厚度均有降低,但24 h后仅低强度血流限制训练组跟腱厚度降低程度明显;PICóN-MARTíNEZ等[30]研究单次不同阻力运动对跟腱厚度的影响,低强度运动组和低强度血流限制训练组受试者进行4组腿部跖屈(1组×30次+3组×15次)30%最大1次重复收缩,高强度组受试者进行高强度的4 组腿部跖屈(1组×30次30%最大1次重复收缩+3组×10次75%最大1次重复收缩),发现低强度血流限制训练组跟腱厚度在运动后即刻、运动后60 min、运动后24 h均显著低于运动前,低强度组和高强度组跟腱厚度均无明显变化,认为单次低强度血流限制训练可使健康人群的跟腱厚度降低;CANFER等[31]研究血流限制训练对健康人群跟腱处皮肤温度的急性影响,发现运动后血流限制训练组和对照组跟腱处皮肤温度均下降,然后均呈线性趋势回升至基线,但血流限制训练组跟腱与跟骨交界处皮肤温度低于对照组。 综上所述,单次血流限制训练和长期血流限制训练对健康青年人跟腱造成影响不同,单次急性干预后肌腱出现减厚趋势,可能低强度血流限制训练导致肌腱内的液体压力增高,使得液体转移到肌细胞或肌腱周围空间,从而导致其肌腱厚度减小,尽管单次阻力运动对肌腱结构形态变化的作用尚不清楚,但急性运动后降低肌腱厚度的作用已被报道为有益的[32],原因可能归于肌腱对机械应力的积极形态学反应;长期血流限制训练引起的跟腱厚度增加程度与高强度训练类似,可能为长时间缺氧环境可诱导肌腱干细胞的增殖[33],增加胶原蛋白的合成率,促进了肌腱的修复增粗,达到预防跟腱损伤的效果。目前仅从跟腱厚度和肌力方面讨论预防足踝损伤有相应的局限性,建议之后预防踝足损伤的研究内容需要从更多方面进行,以保证充分的合理性。 (2)在健康人群踝足部周围肌肉中的应用:缺血调节也是血流限制训练的形式之一。CRUZ等[20]研究单纯缺血调节对健康男性最大跖屈肌力的影响,发现能使受试者小腿三头肌表面肌电增强、踝关节跖屈等长力矩提高,认为缺血调节方式有助于小腿肌肉激活并改善跖屈活动时的肌力。KUBOTA等[34]使用血流限制训练预防肌肉萎缩,将11名健康男性随机分为2组,血流限制训练组与对照组均用石膏固定左踝在中立位,此期间所有受试者使用拐杖行走不负重,血流限制训练组每天使用2次(1次/5组)止血带,在大腿近端进行压迫与释放血流,2周后,血流限制训练组 60 (°)/s 离心收缩时踝跖屈力矩的降低程度明显小于对照组,膝关节屈曲力矩在不同角速度下[60 (°)/s 和 300 (°)/s]降低程度也均小于对照组,认为在下肢50 mmHg袖带压力下重复限制血流可减少制动所引起的肌肉无力。 2.2.2 在足踝损伤中的康复应用 (1)在跟腱断裂后的应用:血流限制训练在跟腱断裂后的恢复中也有相关应用。YOW等[35]通过研究2例跟腱断裂患者,其中1例左脚跟腱断裂患者跟腱修复6个月后仍然有严重的跖屈背屈关节活动障碍,在步行时表现疼痛步态并需要单拐辅助行走,对该患者采用80%肢体闭塞压的血流限制训练进行恢复,5周后患者在 60 (°)/s 和 120 (°)/s 角速度下的肌力增长分别为 4 475%和211%,但与健侧肢体相比还是存在差异,患者可以在没有辅具的情况下行走并恢复跑步功能;另1例双侧跟腱断裂患者右侧跟腱采用常规康复方案,由于持续疼痛和僵硬,恢复改善较为缓慢,左侧跟腱采用80%肢体闭塞压的血流限制训练,6周康复后在60 (°)/s 和 120 (°)/s 角速度下的肌力增长分别为68.8%和78.7%,同样也恢复了跑动能力,并且患者对治疗耐受良好,无不良事件产生。综上所述,该文献为病例数量较少的个案研究,从样本量考虑,具有相应的局限性,因此在未来的研究中应扩大样本量,进一步深入探索,保证研究结果的更准确性。 (2)在慢性踝关节不稳中的应用:踝关节扭伤后约有40%的患者会出现肌力、平衡功能下、本体感觉下降等一系列症状,可能会逐渐演变成慢性踝关节不稳[36],慢性踝关节不稳不仅会导致运动能力的降低,而且可能会引起更大的损伤。FALTUS等[37]通过前期的研究证据提出理论假设:血流限制训练对慢性踝关节不稳患者可能有特别的帮助。KILLINGER等[38]招募19例慢性踝关节不稳患者,采用随机交叉研究分成血流限制训练组与对照组,血流限制训练组在膝盖上方进行80%肢体闭塞压的血流限制训练,完成30%最大外翻与背屈等长收缩训练,纪录运动过程中小腿肌群的表面肌电、氧饱和度变化,发现血流限制训练组外翻与背屈肌肉肌电激活程度均提高,背屈肌力提高,同时肌肉氧饱和度显著降低32%-44%。WERASIRIRAT等[39]将16例慢性踝关节不稳运动员随机分为血流限制训练组和对照组,每组8例,两组均接受传统的康复治疗,血流限制训练组在大腿近端采用80%肢体闭塞压的血流限制训练,干预4周后,与训练前和对照组相比,血流限制训练组踝关节跖屈和外翻在60 (°)/s角速度下的平均峰力矩显著增强、肌肉横截面积显著增粗,但Y平衡测试并未出现组间差异。郑伟亮[40]、周珈奇[41]对患慢性踝关节不稳运动员进行相似研究,发现较高程度闭塞压力(300 mmHg)血流限制训练对受试者健侧踝关节不稳评分有明显改善,认为血流限制训练对增加肌肉力量有显著效果。 研究报道,对慢性踝关节不稳患者进行血流限制训练抗阻运动或动态运动后,肌肉会有不同程度改善[38-39,42]。 BURKHARDT等[42]采用随机交叉研究设计,共纳入25例18-30岁慢性踝关节不稳患者,随机分为血流限制训练组与对照组,血流限制训练组在大腿近端进行80%肢体闭塞压的血流限制训练,完成2次测试的时间相隔为24-48 h,发现血流限制训练组不仅增加了比目鱼肌和股外侧肌的激活程度,同时增加了姿势稳定性评分,改善了平衡能力,这与WERASIRIRAT等[39]研究认为的Y平衡测试并未改善结论不同,造成该不同的原因:一方面,虽然血流限制训练组都是在大腿近端采取80%肢体闭塞压,但造成这种结果的差异可能是由于训练方案和训练时长不同,另一方面可能是由于选择的试验对象不同。 (3)在踝部骨折中的应用:MORTENSEN等[43]报道了1例外踝骨折患者进行血流限制训练康复治疗,该患者为1名年轻女性,在家中进行为期12周、每周4次的血流限制训练,发现血流限制训练可维持受伤肢体的股外侧肌体积、大腿与小腿围度,并且并未出现额外的下肢肿胀及局部压痛,没有出现与运动相关的不良事件或产生运动期间的疼痛。综上,虽该文章样本量较少,有部分局限性,但考虑到严谨,此文纳入了该类文献,虽然个案研究证明了血流限制训练有效,但未来的研究应该考虑到样本量问题,对于该类研究应进一步探索以提高研究内容可靠性。 (4)足踝损伤后的康复小结:综上所述,在足踝损伤康复中以较低的运动强度(20%-30% 1次最大收缩) 进行每周两三次、 每次三四组重复的力竭血流限制(30%-80%肢体闭塞压)抗阻运动,就可以有效促进肌肉力量增长和肌肉肥大,并且血流限制单独使用便可以防止由于无运动状态导致的失用性肌萎缩,有利于加速踝关节损伤后的康复进程。 2.3 血流限制训练的安全性 虽然血流限制训练已应用至肌肉骨骼康复中多年,但其安全性仍存在一定的争议。日本一项对进行血流限制训练受试者的全国调查显示,深静脉血栓形成、肺栓塞和横纹肌溶解症的不良事件发生率分别为0.055%,0.008%和0.008%[44]。当人体进行任何不习惯的剧烈活动时均存在劳力性横纹肌溶解症的风险,血流限制训练的安全性和不良事件报道较少,与常规训练比较损伤风险并无明显差异。HUGHES等[45]强调了血流限制训练作为临床肌肉骨骼损伤后的康复手段具有实用性和有效性,主要适应证包括韧带损伤、髌股疼痛综合征、半月板撕裂、以及肌肉骨骼疾病等。MINNITI等[46]概述了血流限制训练的潜在问题,包括脑出血、横纹肌溶解、持续性麻木、静脉血栓形成、静脉损伤等,得出结论:在生理水平上与常规疗法相比,低强度血流限制训练在外周血流、凝血、中枢心血管反应、氧化应激、肌肉损伤和神经传导速度方面没有显著变化。膝关节炎患者进行血流限制训练的研究发现,高强度运动组中4例患者因膝盖疼痛而退出试验,其余所有患者全部顺利完成试验,均未出现任何不良事件;并且血流限制训练组和高强度训练组在增加膝关节炎患者肌肉力量和肌肉功能方面有相同的效果,血流限制训练还能够改善疼痛、减轻关节应力[47]。ZHANG等[48]通过系统分析血流限制训练对老年人血流动力学反应和血管功能的影响,发现长期低强度血流限制训练可显著改善老年人群血流介导的血管扩张功能、心踝血管指数和踝臂指数。BEAK等[49]将低强度有氧训练联合血流限制训练后发现,血流限制训练并不降低健康男性血管功能。但使用该技术需对患者进行风险评估后选取适当的肢体闭塞压,在能达到治疗效果的同时很大程度减少练期间可能出现的心血管风险[50]。血流限制训练目前被认为是一种安全的干预措施,应用于肌肉骨骼疾病中较多。然而,鉴于研究数量有限、合并样本量小以及研究的患者群体缺乏异质性,需要谨慎解释这些结果。"

| [1] 于长隆,敖英芳.中华骨科学运动创伤卷[M]. 北京:人民卫生出版社,2010;418-420. [2] CAIN MS, BAN RJ, CHEN YP, et al. Four-Week Ankle-Rehabilitation Programs in Adolescent Athletes With Chronic Ankle Instability. J Athl Train. 2020;55(8):801-810. [3] KAUWE M. Acute Achilles Tendon Rupture: Clinical Evaluation, Conservative Management, and Early Active Rehabilitation. Clin Podiatr Med Surg. 2017;34(2):229-243. [4] GLAZEBROOK M, RUBINGER D. Functional Rehabilitation for Nonsurgical Treatment of Acute Achilles Tendon Rupture. Foot Ankle Clin. 2019;24(3):387-398. [5] GOULD HP, BANO JM, AKMAN JL, et al. Postoperative Rehabilitation Following Achilles Tendon Repair: A Systematic Review. Sports Med Arthrosc Rev. 2021;29(2):130-145. [6] HALL EA, CHOMISTEK AK, KINGMA JJ, et al. Balance- and Strength-Training Protocols to Improve Chronic Ankle Instability Deficits, Part I: Assessing Clinical Outcome Measures. J Athl Train. 2018;53(6):568-577. [7] 高维广,刘淑惠,马玉宝,等.软式支具对慢性踝关节不稳患者的即时疗效[J].中国康复理论与实践,2022,28(7):783-788. [8] LÓPEZ-GONZÁLEZ L, FALLA D, LÁZARO-NAVAS I, et al. Effects of Dry Needling on Neuromuscular Control of Ankle Stabilizer Muscles and Center of Pressure Displacement in Basketball Players with Chronic Ankle Instability: A Single-Blinded Randomized Controlled Trial. Int J Environ Res Public Health. 2021;18(4):3012-3020. [9] ABE T, KEARNS CF, MANSO FILHO HC, et al. Muscle,ten-don,and somatotropin responses to the restriction of mus-cle blood flow induced by KAATSU- walk training. Equine Vet J Suppl. 2006;38(S36): 345-348. [10] LOENNEKE JP,THIEBAUD RS, FAHS CA, et al. Effect of cuff type on arterial occlusion. Clin Physiol Funct Imaging. 2013;33(4):325-327. [11] WORTMAN RJ, BROWN SM, SAVAGE-ELLIOTT I, et al. Blood Flow Restriction Training for Athletes: A Systematic Review. Am J Sports Med. 2021;49(7):1938-1944. [12] YASUDA T, FUKUMURA K, TOMARU T, et al. Thigh muscle size and vascular function after blood flow-restricted elastic band training in older women. Oncotarge. 2016;7(23):33595-33607. [13] PIGNANELLI C, CHRISTIANSEN D, BURR JF. Blood flow restriction training and the high-performance athlete: science to application. J Appl Physiol (1985). 2021;130(4):1163-1170. [14] MASON JS, CROWELL MS, BRINDLE RA, et al. The Effect of Blood Flow Restriction Training on Muscle Atrophy Following Meniscal Repair or Chondral Restoration Surgery in Active Duty Military: A Randomized Controlled Trial. J Sport Rehabil. 2022;31(1):77-84. [15] HWANG PS, WILLOUGHBY DS. Mechanisms behind blood flowrestricted training and its effect towards muscle growth. J Strength Cond Res. 2017;33(Sup-pl 1):165-169. [16] WATSON R, SULLIVAN B, STONE A, et al. Blood Flow Restriction Therapy: An Evidence-Based Approach to Postoperative Rehabilitation. JBJS Rev. 2022;10(10):2090-2098. [17] 余尾,宋刚,刘译文.血流限制介入低强度阻力训练对肌肉适能的效益及生理机制[J].中国组织工程研究,2022,26(17):2768-2774. [18] LIM SY, HAUSENLOY DJ. Remote ischemic conditioning: from bench to bedside. Front Physiol. 2012;3:27. [19] MAGA M, SCHÖNBORN M, WACHSMANN-MAGA A, et al. Stimulation of the Vascular Endothelium and Angiogenesis by Blood-Flow-Restricted Exercise. Int J Environ Res Public Health. 2022;19(23):301-307. [20] CRUZ RSO, PEREIRA KL, DE AGUIAR RA, et al. Effects of ischemic conditioning on maximal voluntary plantar flexion contractions. J Electromyogr Kinesiol. 2019;48:37-43. [21] AFSHARIPOUR B, MANZUR N, DUCHCHERER J, et al. Estimation of self-sustained activity produced by persistent inward currents using firing rate profiles of multiple motor units in humans. J Neurophysiol. 2020;124(1):63-85. [22] HUGHES L, PATTERSON SD. Low intensity blood flow restric tion exercise: Rationalefor a hypoalgesiaeffect. Med Hypotheses. 2019; 132:109-117. [23] FRY CS, GLYNN EL, DRUMMOND MJ, et al. Blood flow re-striction exercise stimulates mTORC1 signaling and muscle protein synthesis in older men. J Appl Physiol. 2010;108(5):1199-1209. [24] YANAGISAWA O, SANOMURA M. Effects of low-load resistance exercise with blood flow restriction on high-energy phosphate metabolism and oxygenation level in skeletal muscle. Interv Med Appl Sci. 2017;9(2): 67-75. [25] YANAGISAWA O, FUKUTANI A. Effects of low-load resistance exercise with blood flow restriction on intramuscular hemodynamics, oxygenation level and water content. J Sports Med Phys Fitness. 2018;58(6):793-801. [26] SUGA T, OKITA K, MORITA N, et al. Dose effect on intramuscular metabolic stress during low-intensity resistance exercise with blood flow restriction. J Appl Physiol (1985). 2010;108(6):1563-1567. [27] WOOTEN SV, STRAY-GUNDERSEN S, TANAKA H. Hemodynamic and Pressor Responses to Combination of Yoga and Blood Flow Restriction. Int J Sports Med. 2020;41(11):759-765. [28] CENTNER C, LAUBER B, SEYNNES OR, et al. Low-load blood flow restriction training induces similar morphological and mechanical Achilles tendon adaptations compared with high-load resistance training. J Appl Physiol (1985). 2019;127(6):1660-1667. [29] CHULVI-MEDRANO I, PICÓN-MARTÍNEZ M, CORTELL-TORMO JM, et al. Different Time Course of Recovery in Achilles Tendon Thickness After Low-Load Resistance Training With and Without Blood Flow Restriction. J Sport Rehabil. 2020;30(2):300-305. [30] PICÓN-MARTÍNEZ M, CHULVI-MEDRANO I, CORTELL-TORMO JM, et al. Acute Effects of Resistance Training with Blood Flow Restriction on Achilles Tendon Thickness. J Hum Kinet. 2021;78:101-109. [31] CANFER RJ, CHAUDRY S, MILLER SC. Thermographic assessment of the immediate and short term-effects of blood flow restriction exercise on Achilles tendon skin temperature. Phys Ther Sport. 2021;49:171-177. [32] GRIGG NL, WEARING SC, SMEATHERS JE. Eccentric calf muscle exercise produces a greater acute reduction in Achilles tendon thickness than concentric exercise. Br J Sports Med. 2009;43(4):280-283. [33] JIANG D, JIANG Z, ZHANG Y, et al. Effect of young extrinsic environment stimulated by hypoxia on the function of aged tendon stem cell. Cell Biochem Biophys. 2014;70(2):967-973. [34] KUBOTA A, SAKURABA K, KOH S, et al. Blood flow restriction by low compressive force prevents disuse muscular weakness. J Sci Med Sport. 2011;14(2):95-99. [35] YOW BG, TENNENT DJ, DOWD TC, et al. Blood Flow Restriction Training After Achilles Tendon Rupture. J Foot Ankle Surg. 2018;57(3):635-638. [36] BLEAKLEY C. Understanding chronic ankle instability: model rich, data poor. Br J Sports Med. 2021;55(9):463-464. [37] FALTUS J, OWENS J, HEDT C. Theoretical applications of blood flow restriction training in managing chronic ankle instability in the basketball athlete. Int J Sports Phys Ther. 2018;13(3):552-560. [38] KILLINGER B, LAUVER JD, DONOVAN L, et al. The Effects of Blood Flow Restriction on Muscle Activation and Hypoxia in Individuals With Chronic Ankle Instability. J Sport Rehabil. 2020;29(5):633-639. [39] WERASIRIRAT P, YIMLAMAI T. Effect of supervised rehabilitation combined with blood flow restriction training in athletes with chronic ankle instability: a randomized placebo-controlled trial. J Exerc Rehabil. 2022;18(2):123-132. [40] 郑伟亮.不同压力血流限制训练对慢性踝关节不稳篮球专项运动员的影响[D].广州:广州体育学院,2022. [41] 周珈奇.不同负荷血流限制训练对慢性踝关节不稳足球运动员下肢功能的影响[D].广州:广州体育学院,2022. [42] BURKHARDT M, BURKHOLDER E, GOETSCHIUS J. Effects of Blood Flow Restriction on Muscle Activation During Dynamic Balance Exercises in Individuals With Chronic Ankle Instability. J Sport Rehabil. 2021;30(6):870-875. [43] MORTENSEN L, MECHLENBURG I, LANGGÅRD JØRGENSEN S. Low-Load Blood-Flow-Restricted Exercise to Prevent Muscle Atrophy and Decline in Functional Performance in a Patient Recovering From a Malleolus Fracture. A Case Report. Clin J Sport Med. 2023;33(1):97-100. [44] YASUDA T, MEGURO M, SATO Y, et al. Use and safety of KAATSU training: Results of a national survey in 2016. Int J KAATSU Train Res. 2017;53(5):32-37. [45] HUGHES L, JEFFRIES O, WALDRON M, et al. Influence and reliability of lower-limb arterial occlusion pressure at different body positions. PeerJ. 2018;6(3):623-629. [46] MINNITI MC, STATKEVICH AP, KELLY RL, et al. The Safety of Blood Flow Restriction Training as a Therapeutic Intervention for Patients With Musculoskeletal Disorders: A Systematic Review. Am J Sports Med. 2020;48(7):1773-1785. [47] FERRAZ RB, GUALANO B, RODRIGUES R, et al. Benefits of Resistance Training with Blood Flow Restriction in Knee Osteoarthritis. Med Sci Sport Exer. 2018;50(5):897-905. [48] ZHANG T, TIAN G, WANG X. Effects of Low-Load Blood Flow Restriction Training on Hemodynamic Responses and Vascular Function in Older Adults: A Meta-Analysis. Int J Environ Res Public Health. 2022; 19(11):771-776. [49] BEAK HJ, PARK W, YANG JH, et al. Effect of Low-Intensity Aerobic Training Combined with Blood Flow Restriction on Body Composition, Physical Fitness, and Vascular Responses in Recreational Runners. Healthcare (Basel). 2022;10(9):88-92. [50] LORENZ DS, BAILEY L, WILK KE, et al. Blood Flow Restriction Training. J Athl Train. 2021;(9):211-216. |
| [1] | Zhang Zixian, Xu Youliang, Wu Shaokui, Wang Xiangying. Effects of blood flow restriction training combined with resistance training on muscle indicators in college athletes: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1705-1713. |
| [2] | Liu Chenchen, Liu Ruize, Bao Mengmeng, Fang Li, Cao Liquan, Wu Jiangbo. Blood flow restriction training intervention in the elderly with sarcopenic obesity [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6963-6970. |
| [3] | Wei Mengli, Zhong Yaping, Gui Huixian, Zhou Yiwen, Guan Yeming, Yu Shaohua. Sports injury prediction model based on machine learning [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(2): 409-418. |
| [4] | Jia Yuexin, Tian Saisai, Qi Xiaohong, Zhang Suqin. Effects of 12 weeks of low-intensity resistance training combined with blood flow restriction training on body composition, muscle strength, and arterial elastic function in young adults [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(12): 2521-2527. |
| [5] | Weng Rui, Lin Dongxin, Guo Haiwei, Zhang Wensheng, Song Yuke, Lin Hongheng, Li Wenchao, Ye Linqiang. Abnormal types of intervertebral disc structure and related mechanical loading with biomechanical factors [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1436-1442. |
| [6] | Kong Jianda, Xie Yingao, Chen Shijuan, Zhu Lei. Blood flow restriction training interventions for sarcopenia in older adults: biological mechanisms and proposed application protocols [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3743-3750. |
| [7] | Dong Kuan, Xu Chengli, Tian Jing, Xu Changchun. Effects of endurance training with blood flow restriction on aerobic capacity, lower limb muscle strength, and sports performance: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3766-3772. |
| [8] | Cui Jiali, Huang Minhui, Liu Donglin, Jia Ruiming, Li Han. Computer aided design of 3D dental segmentation and its application scenarios [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(2): 252-257. |
| [9] | Xie Enli, Tao Huimin. Application trends of blood flow restriction training in clinical rehabilitation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(2): 258-262. |
| [10] | Zhang Yue, Guo Yingjie, Cheng Yang, Yang Tingting. Effect of blood flow restriction training on the fitness benefit of upper limb muscles [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(14): 2248-2253. |
| [11] | Zuo Huiwu, Geng Zhizhong, Chen Peng, Lin Xikai, Chen Jian. Knee function recovery in patients with anterior cruciate ligament reconstruction after blood flow restriction training: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(12): 1962-1968. |
| [12] | Pan Weimin, Wang Bing, Han Yabing, Li Ting, Song Jiaqi, Qin Huasheng, Liu Yang. Effects of blood flow restriction training on muscle strength, muscle mass and physical performance in older adults: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(5): 805-812. |
| [13] | Qin Jing, Zhang Suping, Li Li, Zhang Ran, Peng Yingnan, Gao Siyu, Fan Jinpeng, Bian Zhilei, Wan Dingming. Analysis of risk factors for varicella-zoster virus infection after allogeneic hematopoietic stem cell transplantation [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(33): 5292-5297. |
| [14] | Bai Xing, Wang Guojun, Wang Shaokun. Improvement of cognitive function by blood flow restriction training: mechanisms and applications [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(28): 4577-4585. |
| [15] | Jing Jinpeng, Zhang Yue, Liu Xiaomin, Liu Yi. Traditional Chinese medicine injection for promoting blood circulation in prevention of deep vein thrombosis after orthopedic surgery: network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1467-1476. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||