[1] LI Y, TENG D, SHI X, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. 2020;369:m997.
[2] 肖凡,周聪,曹淼,等.黄芪桂枝五物汤通过调节内质网应激对MKR小鼠糖尿病周围神经病变的作用[J].中国实验方剂学杂志, 2022,28(16):1-8.
[3] FELDMAN EL, CALLAGHAN BC, POP-BUSUI R, et al. Diabetic neuropathy. Nat Rev Dis Primers. 2019;5(1):42.
[4] SENDI RA, MAHRUS AM, SAEED RM, et al. Diabetic peripheral neuropathy among Saudi diabetic patients: A multicenter cross-sectional study at primary health care setting. J Family Med Prim Care. 2020;9(1):197-201.
[5] 周海平,周君,杨涛,等.糖尿病周围神经病变的发病机制及相关生物学标志物研究进展[J].中华糖尿病杂志,2021,13(2):187-190.
[6] PANG L, LIAN X, LIU H, et al. Understanding Diabetic Neuropathy: Focus on Oxidative Stress. Oxid Med Cell Longev. 2020;2020:9524635.
[7] YE D, FAIRCHILD TJ, VO L, et al. Painful diabetic peripheral neuropathy: Role of oxidative stress and central sensitisation. Diabet Med. 2022; 39(1):e14729.
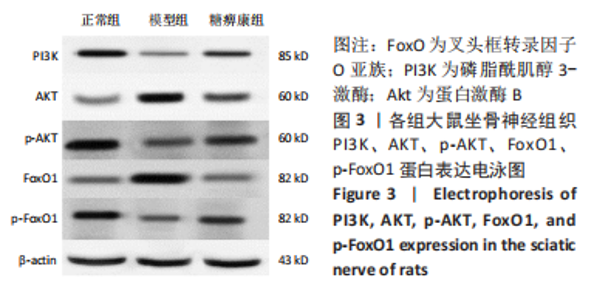
[8] AN J, HE H, YAO W, et al. PI3K/Akt/FoxO pathway mediates glycolytic metabolism in HepG2 cells exposed to triclosan (TCS). Environ Int. 2020;136:105428.
[9] LIU Y, TONG C, TANG Y, et al. Tanshinone IIA alleviates blast-induced inflammation, oxidative stress and apoptosis in mice partly by inhibiting the PI3K/Akt/FoxO1 signaling pathway. Free Radic Biol Med. 2020;152:52-60.
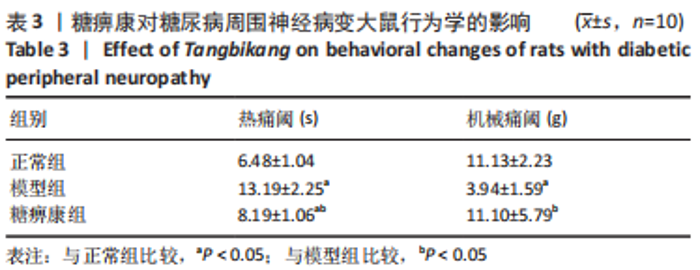
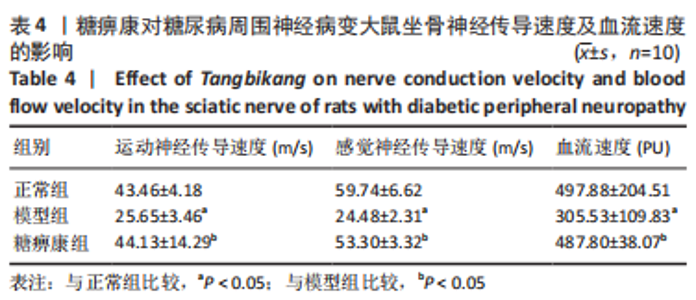
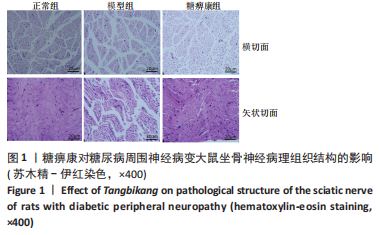
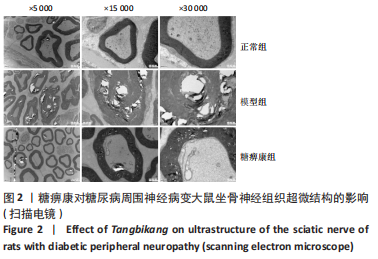
[10] 穆晓红,刘铜华,秦灵灵,等.从血液流变学和坐骨神经传导速度评价中药糖痹康对大鼠糖尿病周围神经病变的影响[J].中华中医药杂志,2012,27(2):378-381.
[11] 穆晓红,刘铜华,孙文,等.糖痹康对高糖培养雪旺细胞自噬相关蛋白的影响[J].中国实验方剂学杂志,2018,24(10):90-94.
[12] 穆晓红,刘铜华,秦灵灵,等.糖痹康对糖尿病周围神经病变大鼠氧化应激的影响[J].河南中医,2017,37(11):1928-1930.
[13] YANG XW, LIU FQ, GUO JJ, et al. Antioxidation and anti-inflammatory activity of Tang Bi Kang in mices with diabetic peripheral neuropathy. BMC Complement Altern Med. 2015;15:66.
[14] YANG X, YAO W, LI Q, et al. Mechanism of Tang Luo Ning effect on attenuating of oxidative stress in sciatic nerve of STZ-induced diabetic mices. J Ethnopharmacol. 2015;174:1-10.
[15] DEWANJEE S, DAS S, DAS AK, et al. Molecular mechanism of diabetic neuropathy and its pharmacotherapeutic targets. Eur J Pharmacol. 2018;833:472-523.
[16] FELDMAN EL, NAVE KA, JENSEN TS, et al. New Horizons in Diabetic Neuropathy: Mechanisms, Bioenergetics, and Pain. Neuron. 2017; 93(6):1296-1313.
[17] BROWNLEE M. Biochemistry and molecular cell biology of diabetic complications. Nature. 2001;414(6865):813-820.
[18] CHOWDHURY SK, SMITH DR, FERNYHOUGH P. The role of aberrant mitochondrial bioenergetics in diabetic neuropathy. Neurobiol Dis. 2013;51:56-65.
[19] FERNYHOUGH P. Mitochondrial dysfunction in diabetic neuropathy: a series of unfortunate metabolic events. Curr Diab Rep. 2015;15(11):89.
[20] LI H, TANG Z, CHU P, et al. Neuroprotective effect of phosphocreatine on oxidative stress and mitochondrial dysfunction induced apoptosis in vitro and in vivo: Involvement of dual PI3K/Akt and Nrf2/HO-1 pathways. Free Radic Biol Med. 2018;120:228-238.
[21] LIU YP, SHAO SJ, GUO HD. Schwann cells apoptosis is induced by high glucose in diabetic peripheral neuropathy. Life Sci. 2020;248:117459.
[22] 魏爽,李冀,韩东卫,等.基于网络药理学探讨黄芪-葛根药对对T2DM模型大鼠PI3K/Akt/FoxO1信号通路的调节作用[J].中国实验方剂学杂志,2022,28(5):157-168.
[23] REN BC, ZHANG YF, LIU SS, et al. Curcumin alleviates oxidative stress and inhibits apoptosis in diabetic cardiomyopathy via Sirt1-Foxo1 and PI3K-Akt signalling pathways. J Cell Mol Med. 2020;24(21):12355-12367.
[24] 郇昕,王素美.中医特色疗法治疗糖尿病周围神经病变的研究进展[J].中国中医药现代远程教育,2022,20(14):206-208.
[25] 张宏,刘铜华.论“毒”与糖尿病周围神经病变[J].吉林中医药, 2011,31(9):817-819.
[26] 张露. 糖痹康对糖尿病小鼠周围神经PTEN介导DNA氧化损伤的作用与机制研究[D].北京:北京中医药大学,2018.
[27] 吕翠岩,张胜容,赵文景,等.糖痹康治疗糖尿病周围神经病变的临床研究[J].天津中医药,2016,33(1):5-9.
[28] XUE T, ZHANG X, XING Y, et al. Advances About Immunoinflammatory Pathogenesis and Treatment in Diabetic Peripheral Neuropathy. Front Pharmacol. 2021;12:748193.
[29] CHU PM, YU CC, TSAI KL, et al. Regulation of Oxidative Stress by Long Non-Coding RNAs in Vascular Complications of Diabetes. Life (Basel). 2022;12(2):274.
[30] XING YQ, LI A, YANG Y, et al. The regulation of FOXO1 and its role in disease progression. Life Sci. 2018;193:124-131.
|