[1] IGLESIAS-RODRÍGUEZ S, DOMÍNGUEZ-PRADO DM, GARCÍA-REZA A, et al. Epidemiology of proximal humerus fractures. J Orthop Surg Res. 2021;16(1):402.
[2] PASSARETTI D, CANDELA V, SESSA P, et al. Epidemiology of proximal humeral fractures: a detailed survey of 711 patients in a metropolitan area. J Shoulder Elbow Surg. 2017;26(12):2117-2124.
[3] SUMREIN BO, HUTTUNEN TT, LAUNONEN AP, et al. Proximal humeral fractures in Sweden-a registry-based study. Osteoporos Int. 2017;28(3):901-907.
[4] VIJAYVARGIYA M, PATHAK A, GAUR S. Outcome Analysis of Locking Plate Fixation in Proximal Humerus Fracture. J Clin Diagn Res. 2016;10(8):RC01-05.
[5] GREGORY TM, VANDENBUSSCHE E, AUGEREAU B. Surgical treatment of three and four-part proximal humeral fractures. Orthop Traumatol Surg Res. 2013;99(1 Suppl):S197-207.
[6] KONRAD G, BAYER J, HEPP P, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Surgical technique. J Bone Joint Surg Am. 2010;92 Suppl 1 Pt 1:85-95.
[7] PAVONE V, VESCIO A, DENARO R, et al. Use of different devices for surgical treatment of proximal humerus fractures in adults: a systematic review. Acta Biomed. 2021;92(4):e2021198.
[8] GARDNER MJ, BORAIAH S, HELFET DL, et al. Indirect medial reduction and strut support of proximal humerus fractures using an endosteal implant. J Orthop Trauma. 2008;22(3):195-200.
[9] CHOW RM, BEGUM F, BEAUPRE LA, et al. Proximal humeral fracture fixation: locking plate construct ± intramedullary fibular allograft. J Shoulder Elbow Surg. 2012;21(7):894-901.
[10] CHEN H, JI X, ZHANG Q, et al. Clinical outcomes of allograft with locking compression plates for elderly four-part proximal humerus fractures. J Orthop Surg Res. 2015;10:114.
[11] 唐迪.锁定钢板结合异体腓骨支撑与单独锁定钢板固定治疗肱骨近端骨折疗效的Meta分析[D].重庆:重庆医科大学,2021.
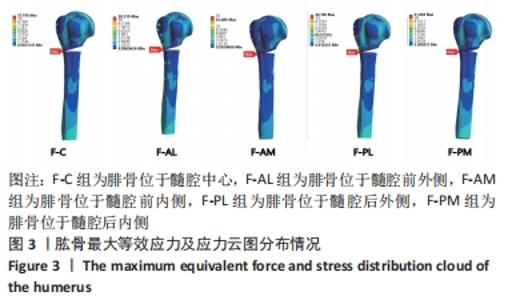
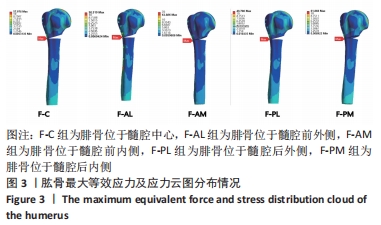
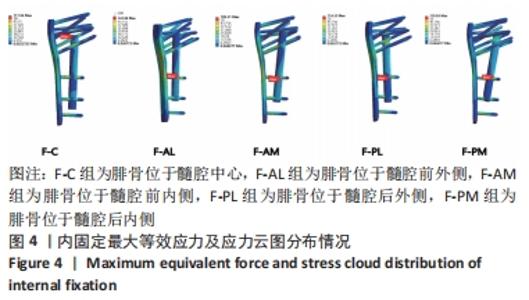
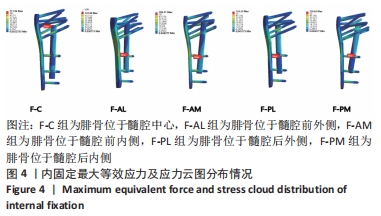
[12] 沈施耘,李雄峰,吴猛,等.锁定钢板结合不同腓骨植骨方式治疗肱骨近端骨折的生物力学稳定性分析[J].中华创伤骨科杂志,2019,21(5):427-431.
[13] CLAVERT P, ZERAH M, KRIER J, et al. Finite element analysis of the strain distribution in the humeral head tubercles during abduction: comparison of young and osteoporotic bone. Surg Radiol Anat. 2006;28(6):581-587.
[14] KENNEDY J, MOLONY D, BURKE NG, et al. Effect of calcium triphosphate cement on proximal humeral fracture osteosynthesis: a cadaveric biomechanical study. J Orthop Surg (Hong Kong). 2013;21(2):173-177.
[15] KANNUS P, PALVANEN M, NIEMI S, et al. Rate of proximal humeral fractures in older Finnish women between 1970 and 2007. Bone. 2009;44(4):656-659.
[16] CRUICKSHANK D, LEFAIVRE KA, JOHAL H, et al. A scoping review of biomechanical testing for proximal humerus fracture implants. BMC Musculoskelet Disord. 2015;16:175.
[17] 章伟.新型肱骨近端锁定钢板的三维有限元模型建立及生物力学研究[D].苏州:苏州大学,2014.
[18] 何仿.人体肩关节三维有限元模型的建立、验证及在肱骨骨折机制研究方面的应用[D].上海:第二军医大学,2006.
[19] MIN KS, SHERIDAN B, WARYASZ GR, et al. Predicting reoperation after operative treatment of proximal humerus fractures. Eur J Orthop Surg Traumatol. 2021; 31(6):1105-1112.
[20] HE Y, HE J, WANG F, et al. Application of Additional Medial Plate in Treatment of Proximal Humeral Fractures With Unstable Medial Column: A Finite Element Study and Clinical Practice. Medicine (Baltimore). 2015;94(41):e1775.
[21] ZHU L, LIU Y, YANG Z, et al. Locking plate fixation combined with iliac crest bone autologous graft for proximal humerus comminuted fracture. Chin Med J (Engl). 2014;127(9):1672-1676.
[22] CHEN H, JI X, ZHANG Q, et al. Clinical outcomes of allograft with locking compression plates for elderly four-part proximal humerus fractures. J Orthop Surg Res. 2015;10:114.
[23] JANG Y, KIM D. Biomechanical study of Proximal humeral fracture fixation: Locking plate with medial support screw vs. locking plate with intramedullary fibular graft. Clin Biomech (Bristol, Avon). 2021;90:105510.
[24] PANCHAL K, JEONG JJ, PARK SE, et al. Clinical and radiological outcomes of unstable proximal humeral fractures treated with a locking plate and fibular strut allograft. Int Orthop. 2016;40(3):569-577.
[25] CUI X, CHEN H, MA B, et al. Fibular strut allograft influences reduction and outcomes after locking plate fixation of comminuted proximal humeral fractures in elderly patients: a retrospective study. BMC Musculoskelet Disord. 2019;20(1):511.
|