中国组织工程研究 ›› 2013, Vol. 17 ›› Issue (4): 639-646.doi: 10.3969/j.issn.2095-4344.2013.04.012
• 骨与关节图像与影像 bone and joint imaging • 上一篇 下一篇
下肢步进摄影获取下肢全长片的精确与可靠性
吴 昊1,石泽锋1,李荣祝1,尹 东1,周艳芳2,董慧萍2,梁 红2,陈 俊2
- 广西壮族自治区人民医院,1骨科,2放射科,广西壮族自治区南宁市 530021
-
收稿日期:2012-04-19修回日期:2012-05-16出版日期:2013-01-22发布日期:2013-03-05 -
作者简介:吴昊,男,1963年生,广西壮族自治区南宁市人,1985年广西医科大学毕业,主任医师,主要从事计算机辅助骨科手术的研究。
Accuracy and reliability of peripheral stepping angiography for full lower extremity alignment measurement
Wu Hao1, Shi Ze-feng1, Li Rong-zhu1, Yin Dong1, Zhou Yan-fang2, Dong Hui-ping2, Liang Hong2, Chen Jun2
- 1 Department of Orthopedics, People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning 530021, Guangxi Zhuang Autonomous Region, China
2 Department of Radiology, People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning 530021, Guangxi Zhuang Autonomous Region, China
-
Received:2012-04-19Revised:2012-05-16Online:2013-01-22Published:2013-03-05 -
About author:Wu Hao, Chief physician, Department of Orthopedics, People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning 530021, Guangxi Zhuang Autonomous Region, China wuhaorthop@yahoo.com.cn
摘要:
背景:精确和可靠的下肢全长片在胫骨高位截骨和膝关节置换前准备和置换后评估中都非常重要。 目的:通过下肢步进摄影一次性曝光成像方法获取下肢全长片,并对其进行测量分析。 方法:对13例膝骨性关节炎伴膝内翻患者进行站立位和平卧位的下肢步进摄影获取下肢全长片,由骨科医师在X射线底片上用量角器测量下肢力线角,由放射科医师在计算机屏幕上进行下肢力线角的测量。对所得数据进行差异对比和相关系数研究。 结果与结论:应用下肢步进摄影法一次曝光所得的X射线下肢全长片具有较高的精确性和可靠性,手工测量和计算机辅助测量有很好的相关性(r=0.638- 0.975)。说明下肢步进摄影获取下肢全长片是一种快捷,简便而有效的检查方法。
中图分类号:
引用本文
吴 昊,石泽锋,李荣祝,尹 东,周艳芳,董慧萍,梁 红,陈 俊. 下肢步进摄影获取下肢全长片的精确与可靠性[J]. 中国组织工程研究, 2013, 17(4): 639-646.
Wu Hao1, Shi Ze-feng, Li Rong-zhu, Yin Dong, Zhou Yan-fang, Dong Hui-ping, Liang Hong, Chen Jun. Accuracy and reliability of peripheral stepping angiography for full lower extremity alignment measurement[J]. Chinese Journal of Tissue Engineering Research, 2013, 17(4): 639-646.
Quantitative analysis of the subjects
Thirteen patients with 26 limbs were included in this study for the final analysis.
Baseline data of the subjects
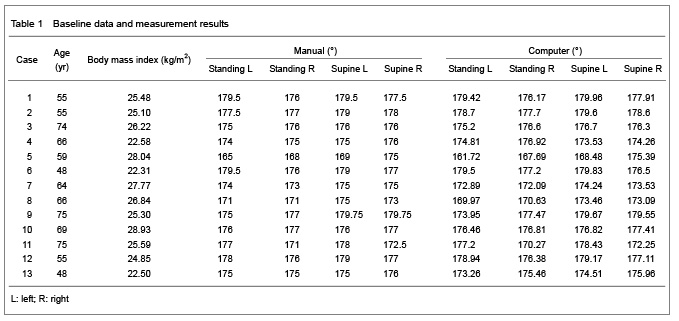
The baseline data of the 13 subjects were shown in Table 1.
Comparison of the results under different positions and with different measurement methods
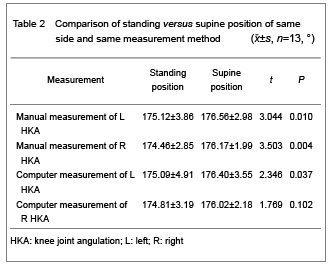
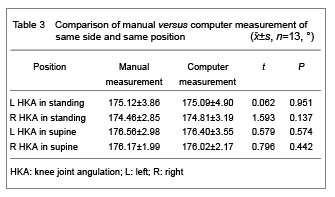
There was a difference of the angle of left and right limb alignment between standing and supine position when measured with manual measurement and computer-assisted measurement method (P < 0.05 or P < 0.01), showed in Table 2; there was no difference under different positions and sides between manual and computer-assisted measurement methods (P > 0.05), as shown in Table 3.
Correlation between the measurement results under different positions and different measurement methods
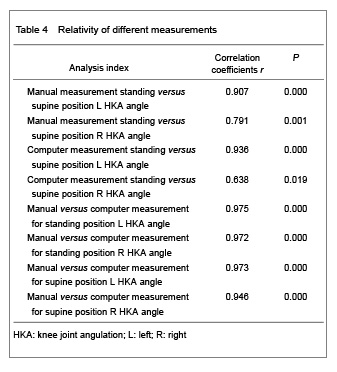
All correlation coefficients of this study were ranged from good to excellent (r=0.638-0.975) (Table 4). For mechanical axis data, the correlation coefficients of hard copy radiograph compared to PACS ranged from 0.638 to 0.975. The correlation coefficients of hard copy radiograph in standing position compared to supine position ranged from 0.638 to 0.938. The correlation coefficients of PACS in standing position compared to supine position ranged from 0.638 to 0.936. The value of the difference between standing and supine position was below two degrees.
| [1] Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69(5):745-749.[2] Cooke TD, Scudamore RA, Bryant JT, et al. A quantitative approach to radiography of the lower limb. Principles and applications.J Bone Joint Surg Br. 1991;73(5):715-720.[3] Tang WM, Zhu YH, Chiu KY. Axial alignment of the lower extremity in Chinese adults. J Bone Joint Surg Am. 2000; 82-A(11):1603-1608.[4] Lohman M, Tallroth K, Kettunen JA, et al. Changing from analog to digital images: does it affect the accuracy of alignment measurements of the lower extremity? Acta Orthop. 2011;82(3):351-355.[5] Skyttä ET, Haapamäki V, Koivikko M, et al. Reliability of the hip-to-ankle radiograph in determining the knee and implant alignment after total knee arthroplasty.Acta Orthop Belg. 2011;77(3):329-335.[6] Segev E, Hemo Y, Wientroub S, et al. Intra- and interobserver reliability analysis of digital radiographic measurements for pediatric orthopedic parameters using a novel PACS integrated computer software program. J Child Orthop. 2010;4(4):331-341. [7] Khakharia S, Bigman D, Fragomen AT, et al. Comparison of PACS and hard-copy 51-inch radiographs for measuring leg length and deformity. Clin Orthop Relat Res. 2011;469(1): 244-250.[8] Gordon JE, Chen RC, Dobbs MB, et al. Interobserver and intraobserver reliability in the evaluation of mechanical axis deviation. J Pediatr Orthop. 2009;29(3):281-284. [9] Marx RG, Grimm P, Lillemoe KA, et al. Reliability of lower extremity alignment measurement using radiographs and PACS. Knee Surg Sports Traumatol Arthrosc. 2011;19(10): 1693-1698. [10] Amendola A, Bonasia DE. Results of high tibial osteotomy: review of the literature. Int Orthop. 2010;34(2):155-160.[11] Fu Y, Wang M, Liu Y, et al. Alignment outcomes in navigated total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. In press.[12] Sabharwal S, Zhao C. Assessment of lower limb alignment: supine fluoroscopy compared with a standing full-length radiograph.J Bone Joint Surg Am. 2008;90(1):43-51.[13] Sabharwal S, Kumar A. Methods for assessing leg length discrepancy. Clin Orthop Relat Res. 2008;466(12):2910- 2922.[14] Sabharwal S, Zhao C. The hip-knee-ankle angle in children: reference values based on a full-length standing radiograph. J Bone Joint Surg Am. 2009;91(10):2461-2468.[15] Sabharwal S, Zhao C, Edgar M. Lower limb alignment in children: reference values based on a full-length standing radiograph. J Pediatr Orthop. 2008;28(7):740-746.[16] Sabharwal S, Zhao C, McKeon JJ, et al. Computed radiographic measurement of limb-length discrepancy. Full-length standing anteroposterior radiograph compared with scanogram. J Bone Joint Surg Am. 2006;88(10): 2243-2251. [17] Schmitt H, Kappel H, Moser MT, et al. Determining knee joint alignment using digital photographs. Knee Surg Sports Traumatol Arthrosc. 2008;16(8):776-780. [18] Khakharia S, Bigman D, Fragomen AT, et al. Comparison of PACS and hard-copy 51-inch radiographs for measuring leg length and deformity. Clin Orthop Relat Res. 2011;469(1): 244-250.[19] Sled EA, Sheehy LM, Felson DT, et al. Reliability of lower limb alignment measures using an established landmark-based method with a customized computer software program. Rheumatol Int. 2011;31(1):71-77.[20] Brouwer RW, Jakma TS, Brouwer KH, et al. Pitfalls in determining knee alignment: a radiographic cadaver study. J Knee Surg. 2007;20(3):210-215.[21] Hinman RS, May RL, Crossley KM. Is there an alternative to the full-leg radiograph for determining knee joint alignment in osteoarthritis? Arthritis Rheum. 2006;55(2): 306-313.[22] Liodakis E, Kenawey M, Doxastaki I, et al. Upright MRI measurement of mechanical axis and frontal plane alignment as a new technique: a comparative study with weight bearing full length radiographs. Skeletal Radiol. 2011;40(7):885-889.[23] Kendoff D, Citak M, Pearle A, et al. Influence of lower limb rotation in navigated alignment analysis: implications for high tibial osteotomies. Knee Surg Sports Traumatol Arthrosc. 2007;15(8):1003-1008.[24] Saragaglia D, Blaysat M, Mercier N, et al. Results of forty two computer-assisted double level osteotomies for severe genu varum deformity. Int Orthop. In press.[25] Brouwer RW, Jakma TS, Bierma-Zeinstra SM, et al. The whole leg radiograph: standing versus supine for determining axial alignment. Acta Orthop Scand. 2003;74(5):565-568.[26] Ariumi A, Sato T, Kobayashi K, et al. Three-dimensional lower extremity alignment in the weight-bearing standing position in healthy elderly subjects. J Orthop Sci. 2010; 15(1):64-70. |
| [1] | 李晓敏, 田向东, 王朝鲁. 单平面胫骨高位截骨:股腓角作为力线矫正的参考标志[J]. 中国组织工程研究, 2026, 30(3): 570-576. |
| [2] | 章安琪, 化昊天, 蔡恬媛, 王子成, 孟 卓, 占效谦, 陈国茜. 全膝关节置换后疼痛:研究现状及趋势分析[J]. 中国组织工程研究, 2026, 30(3): 795-804. |
| [3] | 马 驰, 王 宁, 陈 拥, 魏志晗, 刘逢纪, 朴成哲. 3D打印个体化截骨导板结合定制钢板在开放楔形胫骨高位截骨中的应用[J]. 中国组织工程研究, 2025, 29(9): 1863-1869. |
| [4] | 周金海, 李江伟, 王序全, 庄 颖, 赵 瑛, 杨渝勇, 王嘉嘉, 杨 阳, 周仕炼. 不同骨强度下全膝置换过程中发生股骨前皮质切迹的三维有限元分析[J]. 中国组织工程研究, 2025, 29(9): 1775-1782. |
| [5] | 蒋 涛, 张传开, 郝 亮, 刘 勇. MAKO机器人与导航辅助膝关节置换:下肢力线及假体位置准确性比较[J]. 中国组织工程研究, 2025, 29(33): 7150-7157. |
| [6] | 石 雷, 施 松, 陆 跃, 陶 然, 马洪冬. 膝关节单髁置换与胫骨高位截骨治疗内翻性膝骨关节炎的比较[J]. 中国组织工程研究, 2025, 29(3): 503-509. |
| [7] | 苏德君, 董万鹏, 董跃福, 张吉超, 张 震. 非对称型假体设计及全膝关节置换后的力学分析[J]. 中国组织工程研究, 2025, 29(3): 510-516. |
| [8] | 王熠军, 郑 恺, 张连方, 朱 锋, 张韦成, 李荣群, 周 军, 徐耀增. 导航辅助全膝关节置换应用功能学对线恢复患者固有生理力线和关节线倾角[J]. 中国组织工程研究, 2025, 29(27): 5810-5818. |
| [9] | 张一龙, 吴婉玲, 杨文武, 吴鸿涛, 刘文刚, 何敏仪, 赵传喜. 全膝关节置换前膝关节伸屈肌肌肉力量与置换后步态功能的关系[J]. 中国组织工程研究, 2025, 29(27): 5819-5825. |
| [10] | 丁 源, 巩建宝, 张 杰, 乔 原, 徐文龙. 单髁关节置换后患者膝关节等速肌力的特征分析[J]. 中国组织工程研究, 2025, 29(27): 5833-5838. |
| [11] | 王 俊, 张 辉, 李正远, 郝 琳, 陈圣洪, 尹宗生. 新型局部浸润麻醉应用于人工全膝关节置换的早期效果评估[J]. 中国组织工程研究, 2025, 29(27): 5839-5844. |
| [12] | 位长强, 于洪建, 刘宁宁, 张寅啸. 下肢力线调整区域对胫骨高位截骨后膝关节功能及运动学的影响[J]. 中国组织工程研究, 2025, 29(27): 5743-5749. |
| [13] | 朱哲越, 张 晨, 葛 莹, 薛 晗, 李若尘, 吴光伟, 马 瑞. 新型关节韧带数字体查仪量化评估前交叉韧带部分损伤后的膝关节松弛度[J]. 中国组织工程研究, 2025, 29(27): 5795-5801. |
| [14] | 许明岚, 胡小雪, 沈 军, 向 峥, 张成波, 肖涟波. 巨刺电针联合超前镇痛治疗初次单膝人工关节置换后疼痛[J]. 中国组织工程研究, 2025, 29(21): 4529-4536. |
| [15] | 王宇宁, 朱浩天, 刘 康, 丁焕文, 严 瀚. 数字化精准全膝关节置换与传统置换方法的短期效果对比[J]. 中国组织工程研究, 2025, 29(21): 4521-4528. |
Design
A clinical application study.
Time and setting
This study was realized from October 2011 to January 2012 in People’s Hospital of Guangxi Zhuang Autonomous Region.
Subjects
Thirteen osteoarthritis patients were included in this study from October 2011 to January 2012 in People’s Hospital of Guangxi Zhuang Autonomous Region.
Patients were included if they had knee varus on radiograph, experienced knee pain on most days of the past month when consulted in out-patient department.
Patients were excluded if they reported a previous hip or knee joint replacement, hip or lumbar spine arthritis or other joint pathology causing lower-limb pain, a knee injection in preceding 6 months, knee surgery in preceding 6 months, and the knee pain secondary from traumatic decease.
Two male and eleven female patients with 26 limbs were enrolled in this study, aged 48-75 years old (mean 62.23 years). All patients were informed the examination without the ethics problem.
Methods
Standing versus supine position images
Two ways of images, a standing and a supine position were taken with a ZS-100I/ZS-100IR remote-controlled X-ray diagnostic table (made in Japan), the distance between X-ray focus and film was 110 cm, with single expose of 85 kV, 400 mA and 6.3 ms. Peripheral stepping angiography enabled the radiography of entire lower legs with one exposure, the step interval between the exposure starting point (first point) and completing point (second point) was automatically calculated by the system. When positioning the patients, a standing anteroposterior radiograph of both lower extremities was made with the patient facing the radiographic tube and the patellae pointing anteriorly (Figures 1, 2). A supine radiograph was placed the patient in supine on radiolucent table, with the patella pointing toward the ceiling (Figures 3, 4).
.jpg)
.jpg)
.jpg)
.jpg)
Measurement of full-lower extremities alignment
On conventional full-length leg radiographs, line drawing and angle measurement were performed manually with a transparent goniometer and a soft, 0.7 mm diameter and number 2B pencil, and all of the radiographic measurements were performed by senior orthopedic surgeon using the hard copy 51-inch digital radiographs. Angle measurement on digital full-length leg radiographs was performed by a fellowship-trained radiologist on a digital cursor at a Carestream picture archiving and communication system (PACS) workstation using computer-assisted measurement software (IMPAX, AGFA-GEVAERT, Belgium). For the calculation, the center of the femoral head was defined using Mose circle, the midpoint of the knee being defined by the center of condylar notch, and the midpoint of ankle being defined by the center of the superior facet of the talus. Knee joint angulation (HKA) was assessed by measuring the angle between a line drawn from the center of the femoral head to the middle of the femoral condyles and a line drawn from the middle of the tibial condyles to the midpoint of the malleolus. The HKA angle was expressed as degree of deviation from 180 degrees, such that the HKA angle=0 degree in neutral alignment. Varus angles were denoted as negative values and valgus angles as positive[1, 4, 9].
Main outcome measures
The HKA angles from the full-length radiography of all 13 patients were main study issue.
Statistical analysis
Measurement (degree) data were analyzed using the SPSS version 18.0 (SPSS, Chicago, IL, USA), measurement result was shown as mean ± standard deviation; different measurement methods (standing versus supine position) were compared using the pair t-test; different measurement relationship was determined using Pearson’s correlation coefficients, correlation coefficients of 0.5-0.75 were regarded as good, and values > 0.75 were regarded as excellent. A value of P < 0.05 was considered statistically significant.
Accuracy of the measurement
From 80th of the last century, three radiographic exposure was made, one each centered over the ankle, knee and hip joint with the patient lay still, currently, it is made with the lower limbs similarly positioned with both patellae pointing towards the ceiling, three separate AP images are obtained centered over the hip, knee and ankle joint, using three separate cassettes, the film cassette is moved under the patient between exposures while the patient remains motionless, three chest radiographs are employed to present the full-length hip-to-ankle alignment, as recently the use of computed radiography and digital radiography, the precise and reliability ofmeasurement for lower extremity alignment became higher when using PACS[16-19]. Computed radiography uses a plate instead of a cassette and film similar to the card used in some digital cameras and equipment. The plate, as with the card, must be processed to be read. Digital radiography transmits the image directly via cable or wireless to the image display monitor[18]. The technique named peripheral stepping angiography enables the radiography of entire lower legs with one exposure, the digital images can be showed and measured via Carestream PACS workstation using computer-assisted measurement software, the hard copy photography can also be viewed and measured by clinicians. Our result showed the difference of the value between standing and supine position is below 2 degree, the correlation coefficient for the measurement of mechanical axis deviation with the use of standing and supine position, as well as the manual and computer-assisted methods was ranged from good to excellent (0.638-0.975).
Many authors reported their intra-reader and inter-reader reliability and precise for measurement on analog radiographs by hand and digital images by computer assisted technique. Excellent intra-and inter-observer reproducibility of analog mechanical axis measurements has been reported in several studies[16-19]. The intra- and inter-observer variation of orthopedic measurements performed on traditional radiographs has proven not only to be sufficient, but good when performed by experienced radiologists[4].
Manual and computer-assisted measurement
Traditionally, measures have been made by hand, which require the clinician to draw lines on the radiographs to represent the femoral and tibial mechanical or anatomic axes and to manually define the resulting angles. In recent years, with the advent of digital imaging, analog films have been increasingly replaced by digital image. This changed the daily routine work for technicians, clinicians and radiologists and implemented a change not only in the way to obtain the images, but also in the way to archive the images, and all the changes were evaluated. The image transition time in daily clinical practice was decreased. Traditional film evaluation was changed by the image reading on monitor screens, this change not only affects the radiologists, but also affects the orthopedic surgeons. In addition to the change in the visual analysis of images, there has also been a change in how to perform the measurements[4]. As the digital images cannot be evaluated manually, software programs with electronic tools have been developed to aid in the measurements of alignment from digital radiographs[14-20]. Light boxes, rulers and grease pencils have been exchanged for computers using graphics software. Digital image analysis and viewing can be performed from dedicated radiological workstation or from personal computers (PC). More commonly radiologists employ the dedicated high-solution workstations, while clinicians mainly review and analyze their images using PCs. Dedicated workstations are expensive, and usually they have better image resolution and a better supply of functions to facilitate the analysis. The PC programs are usually web-based, and the image quality is largely depend on the combination of PC and screen[4].
Comparisons between manual measures and computer-assisted analysis of alignment have indicated good reliability for both methods, with a tendency towards higher reliability using computer-assisted analysis[11-18]. Several of these studies investigated primarily the reliability of mechanical axis or anatomic axis angle measures[11, 15-17]. Other studies have evaluated specific approaches to measure alignment and assessed the reliability of additional angular measures by hand and by computer. The magnitude of these measurements may not only influence the decision to pursue surgical intervention but may also be used to assess the adequacy of surgical correction.
Lohmand et al [4] investigated the accuracy of alignment measurements performed using four techniques: analog true-size film (35×130 cm), reduced-size film (35×43 cm, 41% of true size), high-resolution workstations and web-based PC. Before that, they assessed the intra- and inter-observer of these four techniques, separately for each technique. They concluded that orthopadic angle measurements for the lower extremity alignment showed a high degree of consistency and reproducibility. The measurements performed on a computer screen are as accurate as those performed on traditional true-size films when evaluating alignment changes and planning surgery. The agreement of the alignment measurements across the four different media was good. Orthopadic angle can be measured as accurately from analog films as from digital screen, regardless of film or monitor size. In the study by Sled et al [19], the accuracy of measurements of lower limb alignment performed on analog films and digital images by 14 trained but not further characterized raters (7 for each method) was compared, and finding to be highly reliable, and digitally performed measurement have been considered more reliable than analog measurements. Our study showed that there was no difference between manual and computer-assisted measurement of different positions and left or right sides, and the correlation coefficients were high.
There are many factors that can affect the accuracy of the measurement, so, in order to avoid these influences, we referenced many studies. A study performed by the experienced radiologists who used standardized positioning and standardized technique showed that both analog or digital, originated from the same original hip-to-ankle can make it possible to avoid misinterpretations and miscalculations due to different picture positioning, exposure, knee flexion and lower limb rotation, which might easily influence the results of measurement. Secondly, before the study, both radiologists agreed on the definition of the landmark, and they used the same goniometer for the analog measurements and the same digital software in the digital analysis. These factors certainly contributed to the small variation between the measurements[4].
Brouwer et al [20] evaluated the leg alignments using full-length anteroposterior radiographs and found that flexion of the knee without rotation of the lower extremity had little effect on angles as projected on full-length anteroposterior radiographs, rotation of the lower extremity without flexion of the knee also had little effect, simultaneous flexion of the knee and rotation of the leg, however, caused large changes in projected angles. Full-length radiographs could be taken without fluoroscopic control as long as the knee could be fully extended. In flexion contracture, a full-length anteroposterior radiograph taken under lateral fluoroscopic control is necessary to obtain the accurate determination of the mechanical axis.
As the study of Hinman et al [21], joint malalignment in the frontal plane is frequent manifestation of knee OA, but it is not clear where it precedes disease onset or occurs as a consequence. Varus malalignment appears to be the most comment deformity; this is probably a result of the high prevalence of medial tibiofemoral OA relative to lateral compartment disease, whereby progressive cartilage loss on the medial side may lead to increasing varus deformity of the knee joint. Frontal plane malalignment has important biomechanical consequences because it influenced loading across the knee during weight bearing.
Comparison of the full-length radiographs between the standing and supine position
The mechanical axis, as determined by the full- length standing anteroposterior radiograph of the lower extremity, is regarded as the gold standard for measuring knee joint alignment in frontal plane[22]. What is the difference and correlation between standing and supine full-length radiograph and what is the clinical use? The key point is that during the operation, the patient is in supine position, in which the intra-operative control is performed by the C-arm radiograph or navigation [13, 23-24]. So it is necessary to assess the difference and correlation between the standing and supine positions full-length radiographs.
The whole leg radiograph, the standard technique for determining axial alignment, is usually taken in a standing position, although some prefer the supine position. In addition to osseous deformities, an abnormal mechanical axis deviation also may be secondary to soft-tissue laxity around the knee. Normally the femoral condyles and tibial plateau are essentially parallel, with a joint line convergence angle of 0-2° media. In patients with collateral ligament laxity or substantial intra-articular bone defect, these two articular surfaces may not remain parallel, with a consequent increase in the joint line convergence angle and mechanical axis deviation. In limbs with excessive ligamentous laxity of the knee, as indicated by a joint line convergence angle of more than three degrees, the reliability of fluoroscopy was found to be less[24]. Brouwer et al [25] performed a standing and a supine whole leg radiograph in 20 patients with a varus alignment and found an average of two degrees more varus deviation in the standing position than in the supine position. Our results showed an average of less than 2 degrees more varus deviation in the standing position than in the supine position. In this study, the value of the difference between standing and supine position is below two degrees.
Sabharwal et al [12] found overall strong (r=0.88) correlation between the use of a standing radiograph and the use of supine fluoroscopy for assessing mechanical axis deviation. They noted a trend for standing radiograph to reveal a greater magnitude of mechanical axis deviation in comparison with fluoroscopy as the severity of varus malalignment of the limb increased.
This makes intuitive sense, as the axial forces across the knee joint are substantially larger during weight-bearing as opposed to the supine position[21]. All correlations for this study were from good to excellent (r=0.638-0.975). In the neutrally aligned knee, the ground reaction force vector passes medially to the joint center, creating an adduction moment that increases medial compartment forces relative to the lateral side. When the knee is malalignment in the varus direction, the moment arm for ground reaction force vector is increased, resulting in higher adduction moment than the observed in the neutral knee. The knee joint is dependent on the integrity of the soft-tissue retrains, including the collateral ligaments, for medial and lateral stability. The lateral collateral ligament complex and iliotibial band provide the primary soft-tissue restraints to lateral joint opening. Knee joint with varus malalignment and a high adduction moment can thus open un-laterally, especially with weight-bearing, creating a larger magnitude of mechanical axis deviation that accounted for the skeletal deformities alone[22, 24, 26]. The limitation of this study is the fact that the sample was not big enough to be sufficient to do statistic analysis. The following study must be done to collect more data to evaluate the accuracy and reliability.
Peripheral stepping angiography for full lower extremity alignement is a fast, easy, convenient and effective examination method. The computer-assisted digital image measurement, as well as manual measurement, seems has high accuracy and reliability for full lower extremity alignment measurement.
作者贡献:第一作者进行实验设计,实验实施为所有作者,第一作者成文并对文章负责。
利益冲突:课题未涉及任何厂家及相关雇主或其他经济组织直接或间接的经济或利益的赞助。
伦理要求:研究取得所有受试者的知情同意。
作者声明:文章为原创作品,数据准确,内容不涉及泄密,无一稿两投,无抄袭,无内容剽窃,无作者署名争议,无与他人课题以及专利技术的争执,内容真实,文责自负。
1 课题主要就下肢步进摄影法一次曝光成像所得的影像学资料进行研究,放射科医生可以进行摄影工作台上的计算机测量,骨科医生可以进行硬胶片上的手工测量,从而比较站立位与平卧位时测量所得的下肢力线角度,再进行它们之间的相关性研究。 2 采用下肢步进摄影法一次曝光成像取得下肢全长影像,通过比较手工测量和计算机辅助测量下肢力线角,结果证实该方法是一种有效的检查方法。
下肢步进摄影技术于1987年被发明,在疾病诊断、手术方案制定及判断疾病预后方面发挥重要作用。随着科技的进步,该技术被不断改进,并被广泛用于临床研究。而精确和可靠的下肢全长片在胫骨高位截骨和膝关节置换术前准备和术后评估中都非常重要。课题主要就下肢步进摄影法一次曝光成像所得的影像学资料进行研究,放射科医生可以进行摄影工作台上的计算机测量,骨科医生可以进行硬胶片上的手工测量,从而比较站立位与平卧位时测量所得的下肢力线角度,再进行它们之间的相关性研究。
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||