[1] NIH Consensus Development Panel on Osteoporosis Prevention D, Therapy. Osteoporosis Prevention, Diagnosis, and Therapy. JAMA. 2001;285(6):785-795.
[2] HU B, ZHANG X, YANG Q, et al. Comparison of the efficacy and safety of vertebroplasty with different pedicle approaches for osteoporotic vertebral. Eur Spine J. 2024;33(8):3191-3212.
[3] SUN K, LIU J, ZHU H, et al. Lower psoas mass indicates worse prognosis in percutaneous vertebroplasty-treated osteoporotic vertebral compression fracture. Sci Rep. 2024;14(1):13880.
[4] 石江友.PKP与传统椎弓根螺钉内固定术治疗不同程度后凸畸形的胸腰段椎体骨质疏松性骨折的疗效比较[D].南昌:南昌大学,2024.
[5] 蒋华,刘涛,陈文芳.社区老年人用药安全现状及对策研究[J].中国实用护理杂志,2011,27(28):64-65.
[6] LIANG D, PEI J, PEI R, et al. Clinical efficacy of percutaneous vertebroplasty versus percutaneous kyphoplasty treating osteoporotic vertebral compression fractures with kyphosis. Eur J Trauma Emerg Surg. 2024;50(3):1043-1049.
[7] ZHANG B, LI T, WANG Z. Efficacy and complications of different surgical modalities of treating osteoporotic spinal compression fracture in the elderly. Am J Transl Res. 2022;14(1):364-372.
[8] 邝冠明,高庆鹏,杨震宇,等.经皮椎体成形术/经皮椎体后凸成形术治疗超高龄患者椎体压缩骨折的疗效和安全性初步研究[J].中华骨与关节外科杂志,2020,13(12):982-986.
[9] TAKAHASHI S, HOSHINO M, YASUDA H, et al. Cost-effectiveness of Balloon Kyphoplasty for Patients With Acute/Subacute Osteoporotic Vertebral Fractures in the Super-Aging Japanese Society. Spine (Phila Pa 1976). 2019;44(5):E298-E305.
[10] YANG B, ZHAO Y, ZHAO Y. Is percutaneous kyphoplasty safe and beneficial for patients aged 90 and over? Medicine (Baltimore). 2022; 101(33):e30138.
[11] DESHPANDE N, HADI MS, LILLARD JC, et al. Alternatives to DEXA for the assessment of bone density: a systematic review of the literature and future recommendations. J Neurosurg Spine. 2023;38(4): 436-445.
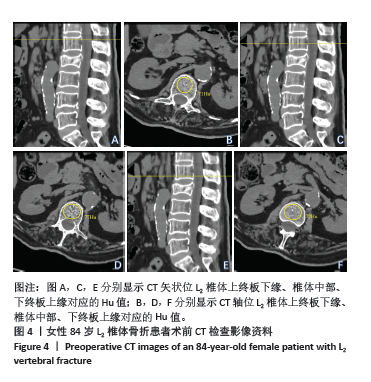
[12] JANG S, GRAFFY PM, ZIEMLEWICZ TJ, et al. Opportunistic Osteoporosis Screening at Routine Abdominal and Thoracic CT: Normative L1 Trabecular Attenuation Values in More than 20 000 Adults. Radiology. 2019;291(2):360-367.
[13] 李龙域,冷子宽,李劲峰,等.超高龄人群脊柱与髋部骨密度差异及其在髋部骨折风险评估中的价值[J].中华实验外科杂志,2023, 40(1):169-172.
[14] CUCCHETTI A, BOCCHINO A, CRIPPA S, et al. Advantages of laparoscopic distal pancreatectomy: Systematic review and meta-analysis of randomized and matched studies. Surgery. 2023;173(4): 1023-1029.
[15] LI C, MENG X, ZHANG J, et al. Associations of metabolic changes and polygenic risk scores with cardiovascular outcomes and all-cause mortality across BMI categories: a prospective cohort study. Cardiovasc Diabetol. 2024;23(1):231.
[16] YU W, ZHANG H, YAO Z, et al. Prediction of subsequent vertebral compression fractures after thoracolumbar kyphoplasty: a multicenter retrospective analysis. Pain Med. 2023;24(8):949-956.
[17] GONG K, SONG M, SHANG C, et al. Risk Factors for New Adjacent and Remote Vertebral Fracture After Percutaneous Vertebroplasty. World Neurosurg. 2024;182:e644-e651.
[18] ZHANG Y, SUN JJ, ZHANG Z, et al. Risk Factors for New Vertebral Compression Fracture After Percutaneous Vertebral Augmentation: A Retrospective Study. Med Sci Monit. 2023;29:e940134.
[19] VISWANATHAN VK, SHETTY AP, RAI N, et al. What is the role of CT-based Hounsfield unit assessment in the evaluation of bone mineral density in patients undergoing 1- or 2-level lumbar spinal fusion for degenerative spinal pathologies? A prospective study. Spine J. 2023;23:1427-1434.
[20] GAO X, DU J, GAO L, et al. Risk factors for bone cement displacement after percutaneous vertebral augmentation for osteoporotic vertebral compression fractures. Front Surg. 2022;9:947212.
[21] JEON I, KIM SW, YU D. Paraspinal muscle fatty degeneration as a predictor of progressive vertebral collapse in osteoporotic vertebral compression fractures. Spine J. 2022;22(2):313-320.
[22] TANG Y, LI H, RUAN X, et al. Percutaneous kyphoplasty with or without posterior pedicle screw fixation for the management of severe osteoporotic vertebral compression fractures with nonunion. J Orthop Surg Res. 2024;19:240.
[23] QI J, HU Y, YANG Z, et al. Incidence, Risk Factors, and Outcomes of Symptomatic Bone Cement Displacement following Percutaneous Kyphoplasty for Osteoporotic Vertebral Compression Fracture: A Single Center Study. J Clin Med. 2022;11(24):7530.
[24] LIU J, TANG J, LIU H, et al. A novel and convenient method to evaluate bone cement distribution following percutaneous vertebral augmentation. Sci Rep. 2020;10:16320.
[25] BLACK DM, CUMMINGS SR, KARPF DB, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996;348(9041):1535-1541.
[26] KLAZEN CA, VENMANS A, DE VRIES J, et al. Percutaneous vertebroplasty is not a risk factor for new osteoporotic compression fractures: results from VERTOS II. AJNR Am J Neuroradiol. 2010;31:1447-1450.
[27] HE D, LOU C, YU W, et al. Cement Distribution Patterns Are Associated with Recompression in Cemented Vertebrae After Percutaneous Vertebroplasty: A Retrospective Study. World Neurosurg 2018;120:e1-e7.
[28] SILVERMAN SL. The clinical consequences of vertebral compression fracture. Bone. 1992;13 Suppl 2:S27-31.
[29] WANG W, LIU Y, WAN H, et al. Effectiveness and prognostic factors of different minimally invasive surgeries for vertebral compression fractures. BMC Musculoskelet Disord. 2023;24(1):11.
[30] CHEN JW, MALDONADO DR, KOWALSKI BL, et al. Best Practice Guidelines for Propensity Score Methods in Medical Research: Consideration on Theory, Implementation, and Reporting. A Review. Arthroscopy. 2022;38(2):632-642.
[31] 李杨,杜怡斌,刘艺明,等.椎体后凸成形注射自固化磷酸钙骨水泥后高龄及应力改变为再发骨折的危险因素[J].中国组织工程研究,2022,26(28):4507-4513.
[32] LING X, CUMMINGS SR, MINGWEI Q, et al. Vertebral fractures in Beijing, China: the Beijing Osteoporosis Project. J Bone Miner Res. 2000;15:2019-2025.
[33] ZHOU C, LIAO Y, CHEN H, et al. Analysis of optimal volume fraction percentage and influencing factors of bone cement distribution in vertebroplasty using digital techniques. J Orthop Surg Res. 2023; 18(1):235.
[34] TANG B, CUI L, CHEN X, et al. Risk Factors for Cement Leakage in Percutaneous Vertebroplasty for Osteoporotic Vertebral Compression Fractures: An Analysis of 1456 Vertebrae Augmented by Low-Viscosity Bone Cement. Spine (Phila Pa 1976). 2021;46(4):216-222.
[35] ROSE LD, BATEMAN G, AHMED A. Clinical significance of cement leakage in kyphoplasty and vertebroplasty: a systematic review. Eur Spine J. 2024;33:1484-1489.
[36] ZHANG A, LIN Y, KONG M, et al. A nomogram for predicting the risk of new vertebral compression fracture after percutaneous kyphoplasty. Eur J Med Res. 2023;28(1):280.
[37] DAI C, LIANG G, ZHANG Y, et al. Risk factors of vertebral re-fracture after PVP or PKP for osteoporotic vertebral compression fractures, especially in Eastern Asia: a systematic review and meta-analysis. J Orthop Surg Res. 2022;17:161.
[38] ZHAO H, HE Y, YANG JS,et al. Can paraspinal muscle degeneration be a reason for refractures after percutaneous kyphoplasty? A magnetic resonance imaging observation. J Orthop Surg Res. 2021;16(1):476.
[39] LI YX, GUO DQ, ZHANG SC, et al. Risk factor analysis for re-collapse of cemented vertebrae after percutaneous vertebroplasty (PVP) or percutaneous kyphoplasty (PKP). Int Orthop. 2018;42:2131-2139.
[40] XIE W, JIN D, MA H, et al. Cement Leakage in Percutaneous Vertebral Augmentation for Osteoporotic Vertebral Compression Fractures: Analysis of Risk Factors. Clin Spine Surg. 2016;29:E171-176.
[41] 罗金金,丁彩田.骨质疏松性椎体压缩骨折经皮椎体后凸成形术后脊柱后凸畸形改善程度的影响因素分析[J].中医正骨,2022,34(8): 8-11.
[42] ZHANG B, ZHOU LP, ZHANG XL, et al. Which Indicator Among Lumbar Vertebral Hounsfield Unit, Vertebral Bone Quality, or Dual-Energy X-Ray Absorptiometry-Measured Bone Mineral Density Is More Efficacious in Predicting Thoracolumbar Fragility Fractures? Neurospine. 2023; 20:1193-1204. |