[1] ZHAO D, ZHANG F, WANG B, et al. Guidelines for clinical diagnosis and treatment of osteonecrosis of the femoral head in adults (2019 version). J Orthop Translat. 2020;21:100-110.
[2] HINES JT, JO WL, CUI Q, et al. Osteonecrosis of the Femoral Head: an Updated Review of ARCO on Pathogenesis, Staging and Treatment. J Korean Med Sci. 2021;36(24):e177.
[3] CHEN Y, MIAO Y, LIU K, et al. Evolutionary course of the femoral head osteonecrosis: Histopathological - radiologic characteristics and clinical staging systems. J Orthop Translat. 2022;32:28-40.
[4] 何伟. 如何把握股骨头坏死患者的保髋治疗时机[J]. 中国骨与关节杂志,2016,5(2):82-86.
[5] MONT MA, SALEM HS, PIUZZI NS, et al. Nontraumatic Osteonecrosis of the Femoral Head: Where Do We Stand Today: A 5-Year Update. J Bone Joint Surg Am. 2020;102(12):1084-1099.
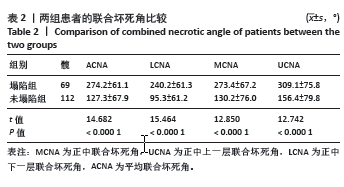
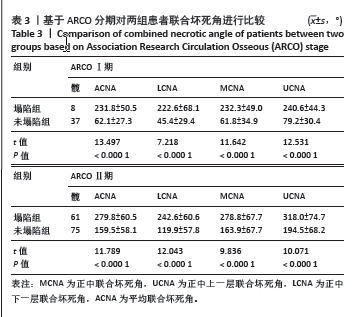
[6] KERBOUL M, THOMINE J, POSTEL M, et al. The conservative surgical treatment of idiopathic aseptic necrosis of the femoral head. J Bone Joint Surg Br. 1974;56(2):291-296.
[7] SHEN X, LUO J, TANG X, et al. Deep Learning Approach for Diagnosing Early Osteonecrosis of the Femoral Head Based on Magnetic Resonance Imaging. J Arthroplasty. 2023;38(10):2044-2050.
[8] 孙伟, 高福强, 李子荣. 股骨头坏死临床诊疗技术专家共识(2022年)[J]. 中国修复重建外科杂志,2022,36(11):1319-1326.
[9] KARANTANAS AH, DRAKONAKI EE. The role of MR imaging in avascular necrosis of the femoral head. Semin Musculoskelet Radiol. 2011;15(3): 281-300.
[10] KOO KH, KIM R. Quantifying the extent of osteonecrosis of the femoral head. A new method using MRI. J Bone Joint Surg Br. 1995;77(6):875-880.
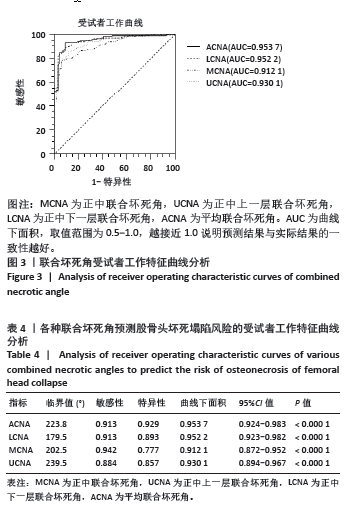
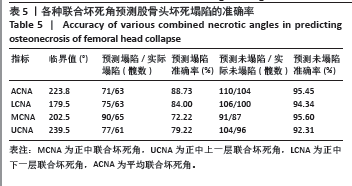
[11] HA YC, JUNG WH, KIM JR, et al. Prediction of collapse in femoral head osteonecrosis: a modified Kerboul method with use of magnetic resonance images. J Bone Joint Surg Am. 2006;88 Suppl 3:35-40.
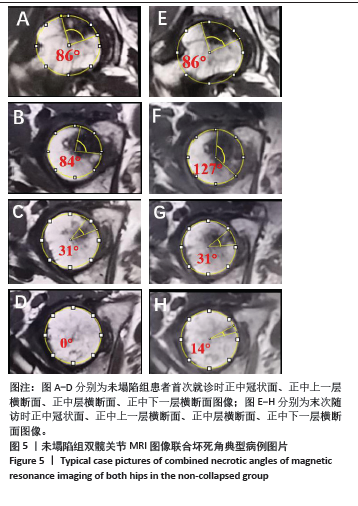
[12] KUBO Y, MOTOMURA G, IKEMURA S, et al. The effect of the anterior boundary of necrotic lesion on the occurrence of collapse in osteonecrosis of the femoral head. Int Orthop. 2018;42(7):1449-1455.
[13] 王秋霞, 史传道, 张高魁, 等. 基于股骨头坏死数据库分析成人股骨头坏死误诊相关因素[J]. 临床误诊误治,2020,33(2):4-9.
[14] FAN Y, ZHANG J, CHEN M, et al. Diagnostic value of necrotic lesion boundary in bone collapse of femoral head osteonecrosis. Int Orthop. 2022;46(3):423-431.
[15] IKEMURA S, MOTOMURA G, KAWANO K, et al. The Discrepancy in the Posterior Boundary of Necrotic Lesion Between Axial and Oblique Axial Slices of MRI in Patients with Osteonecrosis of the Femoral Head. J Bone Joint Surg Am. 2022;104(Suppl 2):33-39.
[16] KOLB AR, PATSCH JM, VOGL WD, et al. The role of the subchondral layer in osteonecrosis of the femoral head: analysis based on HR-QCT in comparison to MRI findings. Acta Radiol. 2019;60(4):501-508.
[17] LIU LH, LI ZR, SUN W, et al. Reliability and Repeatability of the China-Japan Friendship Hospital Typing Classification for Nontraumatic Osteonecrosis of the Femoral Head. J Bone Joint Surg Am. 2022; 104(Suppl 2):40-46.
[18] WEI QS, LI ZQ, HONG ZN, et al. Predicting Collapse in Osteonecrosis of the Femoral Head Using a New Method: Preserved Angles of Anterior and Lateral Femoral Head. J Bone Joint Surg Am. 2022;104(Suppl 2): 47-53.
[19] YUE Y, YANG H, LI Y, et al. Combining ultrasonic and computed tomography scanning to characterize mechanical properties of cancellous bone in necrotic human femoral heads. Med Eng Phys. 2019;66:12-17.
[20] CHI Z, WANG S, ZHAO D, et al. Evaluating the Blood Supply of the Femoral Head During Different Stages of Necrosis Using Digital Subtraction Angiography. Orthopedics. 2019;42(2):e210-e215.
[21] ZHANG Z, YU T, XIE L, et al. Biomechanical bearing-based typing method for osteonecrosis of the femoral head: ABC typing. Exp Ther Med. 2018;16(3):2682-2688.
[22] MA J, GE J, CHENG L, et al. Subchondral Bone Plate Classification: A New and More Sensitive Approach for Predicting the Prognosis of Osteonecrosis of the Femoral Head. Cartilage. 2023;14(3):269-277.
[23] FENG W, YE P, NI S, et al. One-stage simultaneous hip-preserving surgeries for the management of bilateral femoral head osteonecrosis: a mean 7.0-year follow-up. J Orthop Surg Res. 2019; 14(1):455.
[24] TAN B, LI W, ZENG P, et al. Epidemiological Study Based on China Osteonecrosis of the Femoral Head Database. Orthop Surg. 2021; 13(1):153-160.
[25] STEINBERG ME, OH SC, KHOURY V, et al. Lesion size measurement in femoral head necrosis. Int Orthop. 2018;42(7):1585-1591.
[26] HATANAKA H, MOTOMURA G, IKEMURA S, et al. Differences in magnetic resonance findings between symptomatic and asymptomatic pre-collapse osteonecrosis of the femoral head. Eur J Radiol. 2019; 112:1-6.
[27] HINDOYAN KN, LIEBERMAN JR, MATCUK GR, JR, et al. A Precise and Reliable Method of Determining Lesion Size in Osteonecrosis of the Femoral Head Using Volumes. J Arthroplasty. 2020;35(1):285-290.
[28] BOONTANAPIBUL K, HUDDLESTON JI, 3RD, AMANATULLAH DF, et al. Modified Kerboul Angle Predicts Outcome of Core Decompression With or Without Additional Cell Therapy. J Arthroplasty. 2021;36(6): 1879-1886.
[29] 赵汝顺, 郝阳泉, 许鹏, 等. 不同坏死病灶位置对非创伤性股骨头坏死自然病程的影响[J]. 中国组织工程研究,2024,28(6) 917-921.
[30] 鲁超, 刘洪智, 刘道兵, 等. 股骨头坏死病灶分布规律探讨 [J]. 中国矫形外科杂志,2014,22(5):396-400.
[31] IKEMURA S, MAWATARI T, MATSUI G, et al. The depth of the low-intensity band on the T1-weighted MR image is useful for distinguishing subchondral insufficiency fracture from osteonecrosis of the collapsed femoral head. Arch Orthop Trauma Surg. 2018; 138(8):1053-1058.
[32] LAVERNIA CJ, SIERRA RJ. Core decompression in atraumatic osteonecrosis of the hip. J Arthroplasty. 2000;15(2):171-178.
[33] 魏秋实, 何伟, 张庆文, 等. 岭南袁氏中医药防治股骨头坏死传承文化研究[J]. 新中医,2022,54(23):216-220.
[34] SAI KRISHNA MLV, KAR S, KUMAR R, et al. The Role of Conservative Management in the Avascular Necrosis of the Femoral Head: A Review of Systematic Reviews. Indian J Orthop. 2023;57(3):410-420.
[35] 张磊, 金红婷, 童培建. 骨健口服液早期干预非创伤性股骨头坏死的临床研究[J]. 中医正骨,2016,28(3):14-19.
[36] AGARWALA S, BANAVALI SD, VIJAYVARGIYA M. Bisphosphonate Combination Therapy in the Management of Postchemotherapy Avascular Necrosis of the Femoral Head in Adolescents and Young Adults: A Retrospective Study From India. J Glob Oncol. 2018;4:1-11. |