中国组织工程研究 ›› 2024, Vol. 28 ›› Issue (9): 1457-1463.doi: 10.12307/2024.013
• 骨与关节综述 bone and joint review • 上一篇 下一篇
损伤前交叉韧带修复及促进移植物愈合的策略
白 晨1,杨文骞1,孟志超1,王宇泽2
- 1山西医科大学,山西省太原市 030001;2山西医科大学附属第二医院骨科,山西省太原市 030001
-
收稿日期:2023-02-20接受日期:2023-03-23出版日期:2024-03-28发布日期:2023-07-26 -
通讯作者:王宇泽,博士,主任医师,山西医科大学附属第二医院骨科,山西省太原市 030001 -
作者简介:白晨,男,1991年生,山西省临汾市人,汉族,山西医科大学在读硕士。 -
基金资助:山西省青年科技研究基金 (201901D211505),项目负责人:王宇泽
Strategies for repairing injured anterior cruciate ligament and promoting graft healing
Bai Chen1, Yang Wenqian1, Meng Zhichao1, Wang Yuze2
- 1Shanxi Medical University, Taiyuan 030001, Shanxi Province, China; 2Department of Orthopedics of Second Affiliated Hospital of Shanxi Medical University, Taiyuan 030001, Shanxi Province, China
-
Received:2023-02-20Accepted:2023-03-23Online:2024-03-28Published:2023-07-26 -
Contact:Wang Yuze, MD, Chief physician, Department of Orthopedics of Second Affiliated Hospital of Shanxi Medical University, Taiyuan 030001, Shanxi Province, China -
About author:Bai Chen, Master candidate, Shanxi Medical University, Taiyuan 030001, Shanxi Province, China -
Supported by:Shanxi Provincial Youth Science and Technology Research Fund, No. 201901D211505 (to WYZ)
摘要:
文题释义:
前交叉韧带:是膝关节的韧带之一,起源于胫骨平台前内侧,在关节腔内沿着后内方走行,越过后交叉韧带前方,向上止于股骨外侧髁的后内侧。也有研究表明前交叉韧带分为前内侧束和后外侧束两束,可以防止胫骨前移和过度旋转,保持膝关节运动的正常生物力学,以防半月板损伤。前交叉韧带损伤:当人体旋转、切割和跳跃时,膝关节处于轻度屈曲外翻位,此时再加上股四头肌剧烈收缩,便可使胫骨近端受到较大剪切力,附着于胫骨近端的前交叉韧带不能承受其本身的最大应力,导致前交叉韧带撕裂甚至断裂。
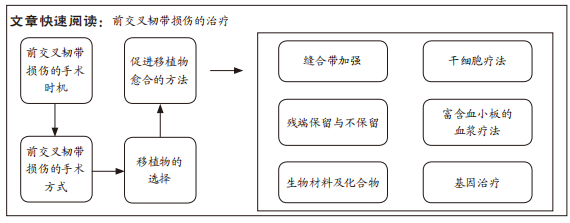
背景:近些年,对于前交叉韧带损伤的治疗日益成熟,但是,临床上对于前交叉韧带损伤的手术时机、手术方式的选择、移植物的选择及促进移植物愈合的方法等问题还存在争议。
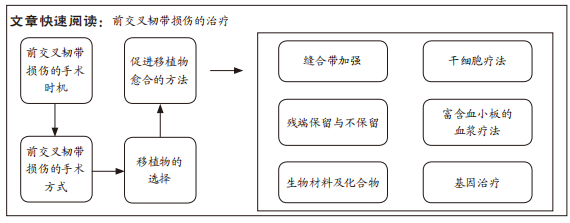
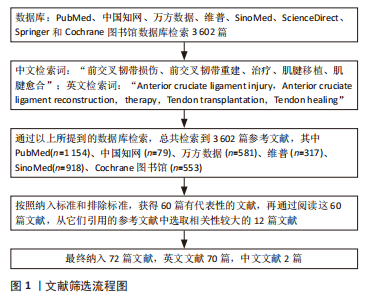
目的:总结前交叉韧带损伤的手术时机、手术方式、移植物选择和促进移植物愈合方法的最新研究进展,为前交叉韧带损伤寻找新的治疗方向。方法:从PubMed、中国知网、万方数据、维普、SinoMed、ScienceDirect、Springer和Cochrane 图书馆数据库进行前交叉韧带损伤相关文献的检索,最终经过筛选纳入相关文献72篇进行综述分析。
结果与结论:①在手术时机方面:前交叉韧带早期重建与延迟重建相比,早期重建可减缓半月板的损伤、提高生活质量、促进功能恢复,然而手术时机的不同是否会加速软骨损伤,目前还无定论。②在手术方式方面:关节镜下前交叉韧带重建术是前交叉韧带损伤的常用手术方式;前交叉韧带动态内稳定修复术在短期和长期疗效中,都可以带来和传统前交叉韧带重建术相似的结局。③在移植物的选择方面:自体腘绳肌肌腱是前交叉韧带移植物的首要选择;骨-髌腱-骨移植物和同种异体移植物作为次要选择。④在促进移植物愈合的策略方面:缝合带加强可以增加膝关节稳定性,保证移植物的愈合;干细胞通过抗炎作用、血管生成作用、抑制骨溶解和促进软骨细胞分化促进移植物的腱-骨愈合;保留前交叉韧带残端可以维持膝关节稳定、促进本体感觉恢复,为移植物的愈合提供先决条件;富血小板血浆促进移植物愈合的有效性有待商榷;而生物材料、基因治疗及干细胞治疗等促进肌腱愈合的方法还停留在分子和动物研究阶段,未来还需要进行临床转化。
https://orcid.org/0000-0006-6352-150X (白晨)
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中图分类号:
引用本文
白 晨, 杨文骞, 孟志超, 王宇泽. 损伤前交叉韧带修复及促进移植物愈合的策略[J]. 中国组织工程研究, 2024, 28(9): 1457-1463.
Bai Chen, Yang Wenqian, Meng Zhichao, Wang Yuze. Strategies for repairing injured anterior cruciate ligament and promoting graft healing[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1457-1463.
2.2 前交叉韧带损伤的手术时机 前交叉韧带损伤的治疗首选关节镜下前交叉韧带重建,而且手术指征也比较明确。DIERMEIER等[10]组成的国际共识专家小组总结了关节镜下前交叉韧带重建的手术指征,主要包括:前交叉韧带撕裂伴随可修复的半月板损伤或多发韧带损伤;胫骨斜率增加;日常活动时,膝关节不稳定或严重错位;从事运动员职业,或者期望恢复跳跃和旋转运动。虽然对于前交叉韧带损伤的手术指征已成国际共识,但是研究者们对于前交叉韧带损伤的手术时机(早期或延迟手术)还未达成共识。
LAROSE等[11]进行了一项随机对照试验,将患者分为前交叉韧带早期重建组(损伤时间< 12周)和延迟重建组(损伤之间> 12周),通过评估患者的软骨磨损程度、半月板损伤情况和术后运动评分,发现延迟重建仅仅会影响患者的生活质量,却不会加重软骨和半月板的损伤。SNOEKE等[12]通过长达5年的研究,对前交叉韧带早期或延迟重建两组患者的半月板损伤情况进行了评估后得出结论,早期重建可减少后内侧半月板损伤,但不能减少或者加重外侧半月板损伤。WIRTH等[13]在前交叉韧带损伤的年轻群体中,进行了前交叉韧带早期或延迟重建的研究,通过核磁检查对比5年后软骨的厚度,表明了对于活动较多的年轻人,手术时机并不能改变股骨和胫骨的软骨磨损情况。REIJMAN等[14]研究表明,在前交叉韧带断裂的患者中,早期重建在提高术后症状、膝关节功能和参与运动的能力方面有着明显的优势。由以上研究可见,前交叉韧带早期重建可减缓半月板的损伤、提高生活质量、增加活动能力,然而,手术时机是否会加速软骨损伤目前还无定论。因此,在临床上要根据患者的活动量、年龄、前交叉韧带损伤程度、伴随症状等因素来对治疗做出正确选择,但是建议选择前交叉韧带早期重建。一旦选择手术治疗,就应该严格把握前交叉韧带重建的手术指征,才能保证患者的安全和手术的顺利进行。
2.3 前交叉韧带重建的手术方式
2.3.1 前交叉韧带修复 前交叉韧带修复术在1970年之前作为前交叉韧带损伤治疗的首选,但是术后前交叉韧带再损伤率> 50%,直到1990年之后,这种手术方式才逐渐被前交叉韧带重建取代[15]。不过随着技术的研究发展,前交叉韧带修复术再次引起关注,近十年讨论比较多的是前交叉韧带动态内稳定修复术,其基本原理为:缝合前交叉韧带断端,将缝线走行于前交叉韧带内部,缝线两端分别用螺钉固定于股骨和胫骨的前交叉韧带止点处,胫骨端的螺钉因带有弹簧而不同[16]。有两项随机对照研究将前交叉韧带断裂的患者分成动态内稳定修复组和自体移植物单束重建组,随访后得出结论,两组术后2年的IKDC评分(the international knee Documentation committee Rating System)、Tegner评分、Lysholm评分和失败率无显著差异[17-18]。也有两项研究进行了为期5年的随机对照研究,证明了动态内稳定修复组和自体移植物单束重建组在术后IKDC评分、KOOS评分(Knee Injury and Osteoarthritis Outcome Score)、失败率和关节松弛度无显著差异[19-20]。因此,不论从短期效果还是长期疗效来看,前交叉韧带动态内稳定修复术都可以带来和传统前交叉韧带重建相似的结局。
2.3.2 前交叉韧带的单束重建或双束重建 关节镜下解剖单束重建是前交叉韧带重建的常用术式,手术大致过程如下:取自体腘绳肌肌腱(半腱肌和股薄肌),缝合编织成为手术待用移植物,制备股骨和胫骨的骨隧道,移植物的股骨端用翻转钢袢固定,移植物的胫骨端用可吸收或不可吸收的挤压螺钉固定。前交叉韧带双束重建是基于前交叉韧带的双束解剖理论提出的手术方式,研究者们对这种手术方式进行了长期的探索和尝试。十余年前的一项研究表明,双束前交叉韧带重建不仅可以重建前交叉韧带的双束解剖结构,还能提供足够的膝关节旋转稳定性[21]。但是最近的多项研究表明,前交叉韧带双束重建和单束重建相比,两者在术后功能评分和膝关节旋转稳定性方面没有差异,双束重建暴露了移植物愈合时间久及手术过程复杂的缺点[22-25]。因此,虽然在过去的十余年,临床工作者对前交叉韧带双束重建的适用性及优劣势做出各种研究,但是这种手术方式并没有体现出巨大的优势,反而由于其手术复杂、移植物愈合速度慢等缺点逐渐被淘汰。
2.3.3 全内前交叉韧带重建 全内前交叉韧带重建又称“all-inside前交叉韧带重建”,是由LUBOWITZ [26]在2006年首次提出。全内前交叉韧带重建与常规前交叉韧带重建的主要不同体现在以下3点[27]:①使用逆行钻孔形成较浅的骨窝结构而不是全层隧道,缩短了骨隧道长度,尽可能多的保留了骨皮质和骨膜;②移植物在胫骨端的固定采用皮质悬吊而不是干涉螺钉;③移植物制备仅需要一条肌腱而不是2条,可以降低供体发病率。YASEN等[28]研究认为,前交叉韧带全内重建的术后主观和客观效果都比较良好,并发症少、失败率低,但是在制作骨隧道时,可能损伤前交叉韧带的机械感受器。近期的多项随机对照研究表明,前交叉韧带全内重建组和传统重建组相比,两者在术后的功能评分上无明显差异,然而全内重建组有创伤小、疼痛小、感染率低及术后屈肌力量强等优点,同时存在关节松弛度高及移植物成熟慢等缺点[29-31]。由上述研究可知,前交叉韧带全内重建在术后功能恢复方面可以和传统重建相媲美,此外,全内重建具有创伤小及感染率低等优势。
因此,在前交叉韧带损伤的手术方式选择上,目前还是以关节镜下前交叉韧带单束重建为主,虽然前交叉韧带双束重建理论上完全符合前交叉韧带的双束解剖观点,但是经过数十年的实践验证,前交叉韧带双束重建并没有明显的优势,反而存在技术难度高、创伤大的缺点。前交叉韧带动态内稳定修复术和全内重建是近几年才流行的新术式,虽然有相关文献报道了它们的安全性和临床适用性,但是缺乏大量证据证明它们的优势,还需要进行更多的临床研究。随着手术技术的提高和手术方式的改进,再加上对于微创手术技术的认识及需求日益增加,前交叉韧带动态内稳定修复术和全内重建在未来很可能成为主流技术。
2.4 前交叉韧带重建的移植物选择 前交叉韧带重建最常用的移植物包括自体腘绳肌腱(hamstring tendon,HT)、自体骨-髌腱-骨(bone-patellar tendon-bone tendon,BPTB)、同种异体移植物、自体股四头肌腱(quadriceps tendon,QT)和人工合成移植物。根据最新研究、综述及Meta分析,将自体腘绳肌、自体骨-髌腱-骨和同种异体移植物的优缺点分别整理归纳[32-34],见图2。
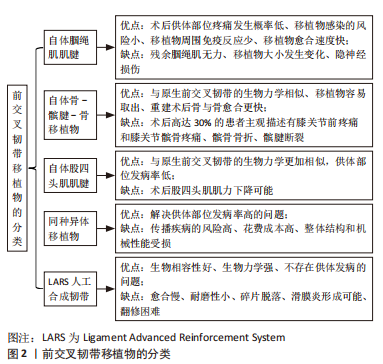
随着减少软组织剥离技术的发展,自体股四头肌腱逐渐表现出和原生前交叉韧带在生物力学上更高的相似性,在前交叉韧带重建后可以提供更加强健和稳定的结构[35]。有人进行了股四头肌移植和自体腘绳肌移植的术后2年效果对比,发现两者在术后的主观结局、膝关节稳定性和再次手术率方面没有差异[36],此外,股四头肌移植的供区发病率较低,但可能发生股四头肌肌力不足。但是,有研究者表明股四头肌移植不会造成术后的股四头肌肌力下降[37]。BARIé等[38]对比了股四头肌移植和骨-髌腱-骨移植的术后10年疗效,总结出两者的术后功能评分、关节松弛度、隧道的增宽均无显著差异,另外,股四头肌移植具有供区发病率低的优点。股四头肌肌腱的优缺点见图2。
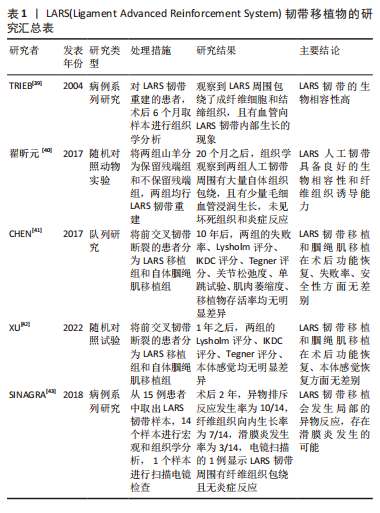
近几年,随着新型材料及合成技术的飞速发展,人工合成移植物逐渐引起人们的兴趣,尤其用聚对酞酸乙二酯材料合成的LARS韧带(Ligament Advanced Reinforcement System)已经广泛应用于临床。TRIEB等[39]在2004年首次对使用LARS韧带重建的患者取样本,通过组织学观察到,6个月后成纤维细胞通过构建囊膜黏附于LARS韧带周围,且LARS韧带上有血管向内生长和结缔组织包绕。翟昕元等[40]也通过动物实验表明了LARS有超高的生物相容性,韧带周围无炎症反应。有研究者进行了一项长达10年的对照研究,发现LARS韧带移植和自体腘绳肌移植在术后功能评分、安全性和失败率方面无差异[41]。同样,XU等[42]通过一项前瞻性研究,对比了LARS韧带移植和自体腘绳肌移植的效果,发现这两种移植技术在术后的功能评分和本体感觉恢复方面无差异。但是有一项研究质疑了LARS韧带的强度,怀疑磨损掉落的碎片可能会导致滑膜炎形成,影响关节功能,增加翻修率[43]。虽然LARS韧带在生物相容性和生物力学方面有明显的优势,然而人工合成移植物同样存在愈合慢、弹性小、耐磨性小及翻修困难等缺点[44]。LARE韧带的优缺点,见图2。LARS韧带移植物的研究汇总,见表1。
总之,在如今的前交叉韧带移植物选择中,自体腘绳肌肌腱是前交叉韧带移植物的首要选择;骨-髌腱-骨移植物由于其供体部位发病率高的缺点,常被作为第二选择;同种异体移植物存在花费成本高、传播疾病和生物力学受损的问题,当自体肌腱无法使用时,才会选择同种异体移植物;股四头肌肌腱因为剥离技术有限,经常导致供体部位肌力下降,近几年剥离技术提高,股四头肌肌腱可以作为移植物的备选;虽然LARS韧带在生物相容性和生物力学方面都比较优秀,但是由于价格昂贵、术后并发症多等原因而当做移植物的备用选择之一。医疗技术在发展,股四头肌肌腱和人工韧带在将来会更加完美。
2.5 促进移植物愈合的方法 移植物愈合过程分为移植物的退变、增殖、韧带化三个阶段,第一阶段:移植物的成纤维细胞坏死,细胞数量急剧减少,产生细胞因子和趋化因子,发生炎症反应,持续约4周;第二阶段:术后4-12周出现移植物的细胞活性升高和细胞外基质变化,以细胞增殖和胶原基质的再吸收为特征,通过移植物血管化,沉积新的胶原,再进行生化和组织学修饰,最后重塑移植物和重建血管;第三阶段:术后12周,移植物进行自适应重塑,达到原生前交叉韧带的生物力学性能和结构,逐渐韧带化[45]。
2.5.1 缝合带加强 是在前交叉韧带断裂并发旋转不稳定的情况下,进行前交叉韧带重建联合前外侧复合体加强术。YOO等[46]研究表明,与孤立前交叉韧带重建相比,联合缝合带加强可以增强移植物的稳定性,使患者可以更快地恢复活动。HAMIDO等[47]也发现,与孤立前交叉韧带重建相比,联合前外侧复合体加强可以降低膝关节旋转不稳定性和器械性膝关节松弛度,提高术后功能评分。可见,缝合带加强可以增加膝关节稳定性,保证移植物的愈合。
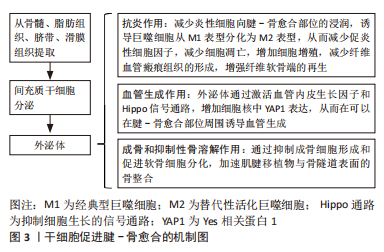
2.5.2 干细胞疗法 干细胞自身具有超强的自我更新能力、长期生存能力和多向分化潜能[48],在促进移植物愈合及再生领域逐渐引起人们注意。干细胞的来源有很多种,包括胚胎干细胞、脂肪组织来源干细胞、骨髓来源间充质干细胞等。在促进移植物愈合方面,最常被研究的是骨髓来源间充质干细胞,这种干细胞一般从手术过程中的骨髓里面提取,在生长因子、机械刺激、生物材料等分化诱导剂的作用下,朝着韧带、纤维软骨和骨的方向分化,并通过旁分泌途径调节炎症,促进移植物再生[49]。
有研究者探索了骨髓来源干细胞的旁分泌机制,通过自身分泌的生长因子、细胞因子和外泌体,调节移植物愈合部位的分子成分,从而有抗凋亡、抗瘢痕形成、促进血管生成和免疫调节的功能,进而达到促进肌腱愈合的目的[50]。LIM等[51]在一项动物模型实验中,将骨髓来源间充质干细胞植入实验组模型的腱-骨愈合界面,和空白组对照发现,实验组模型的腱-骨愈合界面有大量软骨生成,空白组则是瘢痕组织。也有对于脂肪来源干细胞可用性的研究,一项实验发现,和骨髓来源间充质干细胞相比,应用了脂肪组织来源干细胞的模型发生异位骨化的风险和免疫原性均低[52]。然而最近的一项研究对脂肪来源干细胞的作用发出了质疑,这项研究将受试者分为脂肪来源干细胞干预组和空白组,结果提示两组在术后12个月的膝关节功能改善程度和移植物的愈合速率方面无明显差异[53]。为了验证脂肪来源干细胞的有效性,FRANKLIN等[54]发明了肌腱衍生水凝胶,对老鼠模型分别使用肌腱衍生水凝胶和生理盐水,干预1周后两组均给予皮下注射脂肪来源干细胞,结果发现使用了肌腱衍生水凝胶的模型在肌腱愈合程度方面明显优于空白组,通过流式细胞技术证实肌腱衍生水凝胶通过吸引干细胞的归巢促进肌腱愈合。因此,干细胞可以为促进移植物愈合提供新的研究方向,但需要更加先进的技术支持。间充质干细胞促进腱-骨愈合机制图,见图3。
2.5.3 残端保留与不保留 关于前交叉韧带重建中,前交叉韧带的胫骨残端保留与否,也是近几年研究的热点。XIE等[55]通过Meta分析得出,在患者功能评分、膝关节稳定性和胫骨隧道扩大方面,残端保留可以获得更好的结果,但是在并发症(活动范围、再损伤率)方面无明显优势。最近,一项研究表明,在前交叉韧带重建手术中,保留残端组织可能会降低2年内的手术失败率和翻修率[56]。也有学者发现,前交叉韧带残端包含参与本体感觉的机械感受器,将损伤在6个月以内的残端黏附于后交叉韧带,可以保护前交叉韧带的本体感觉,维持膝关节的稳定性,从而对移植物的愈合发挥巨大好处[57]。以上研究证明,保留前交叉韧带残端可以维持膝关节稳定、促进本体感觉恢复,为移植物的愈合提供先决条件。
2.5.4 富血小板血浆(platelet-rich plasma,PRP)疗法 富含血小板的血浆中有很多细胞因子,这些因子参与肌腱的修复,因此PRP被广泛应用。富血小板血浆中血小板内α-颗粒释放的细胞因子,已被证明可以改善炎症、促进细胞增殖、加速组织重塑、促进软骨分化和创面愈合[58]。Mcrobb等[59]研究发现,富血小板血浆通过促进移植物的早期血管化,从而影响着移植物的愈合,最终加速移植物的韧带化。但是,ZHU等[60]通过一项Meta分析得出,富血小板血浆在前交叉韧带重建后中短期内可以减轻术后疼痛,改善膝关节功能,但不能改善膝关节松弛和隧道扩大,也不能加速移植物的愈合。与此同时,CAO等[61]通过一项回顾性研究发现,尽管富血小板血浆的使用在术后影像学的表现上体现出积极作用,但没有足够证据可以证明其有较好的临床效果和促进肌腱愈合的能力。可见,虽然富血小板血浆的生理作用理论上可以促进移植物愈合,但是其促进肌腱愈合的分子机制还需要更多的研究来揭示,富血小板血浆在临床实践中的有效性还有待商榷。
2.5.5 生物材料及化合物 随着生物工程技术的进步,促进移植物肌腱-骨愈合的生物材料和化合物的研究也在迅速发展。生物材料的类型多种多样,包括超高分子量聚乙烯、磷酸钙纳米颗粒、生物纳米纤维支架、镁制品和水凝胶微球等。有研究证明超高分子量聚乙烯具有很高的血管化能力,它表面携带的蛋白质和生长因子可以明显改善肌腱组织再生[62]。LIAO等[63]研究发现,非晶态磷酸钙纳米颗粒能提高肌腱-骨交界处的生物力学强度和促进新生血管的形成,从而促进肌腱-骨愈合。ZHAO等[64]也发现,生物纳米纤维支架有利于细胞的附着和增殖,从而达到促进肌腱-骨愈合的效果。WANG等[65]通过比较钛螺钉和镁螺钉在临床手术中的应用效果发现,镁具有骨诱导的作用,通过促进肌腱移植物腱-骨交界处的矿化,来提高肌腱-骨愈合的速度,此外,镁制品还可以降低骨隧道扩大的发生率。一项研究表明,新型负载细胞因子和细胞的水凝胶微球可以作为多功能药物递送系统,从而促进肌腱-骨愈合[66]。以上所有研究表明,生物材料及化合物已被广泛研究,并取得了良好的效果,在未来很可能被用于临床治疗。
2.5.6 基因治疗 基因治疗的机制是将带有生长因子的基因转染至干细胞,转染后的干细胞分泌特定的生长因子,这些生长因子靶向作用于移植物愈合部位,从而很高效地促进了移植物愈合[67]。一项动物实验研究发现,在移植物-骨隧道交界处植入含有成纤维细胞生长因子的转基因间充质干细胞,可增加成骨细胞数量、改善移植物生物力学性能[68]。因此,基因治疗在理论上可以促进移植物的愈合,但是想把基因治疗应用于临床,还需要更加成熟的技术。
2.5.7 其他方法 促进移植物愈合的新方法还有很多,比如低强度脉冲超声、转化生长因子、骨形态发生蛋白2和多种方式的联合应用等。XU等[69]在一项对大鼠模型的实验中,使用低强度脉冲超声治疗肩袖撕裂,发现使用低强度脉冲超声的实验组,巨噬细胞数量和抗炎基因的表达较高,表明这种无创物理疗法可能是通过促进巨噬细胞极化来促进肌腱的愈合。ARIMURA等[70]通过一项动物实验发现,转化生长因子可以通过抑制基质金属蛋白酶途径,促进愈合部位纤维组织的形成,从而增加移植物的生物学强度。KIM等[71]研究者进行了一项兔子模型的对照实验,结果表明,使用了骨形态发生蛋白2的实验组在第4,8周的骨密度、聚合酶链反应均高于对照组,可见骨形态发生蛋白2也能促进肌腱-骨交界处愈合和提高肌腱-骨交界处的生物力学强度。HAN等[72]发现,骨髓来源间充质干细胞和富血小板血浆联合应用在促进肌腱骨愈合方面有着协同作用。
由以上各点可知,外侧复合体缝合带加强和前交叉韧带保留残端重建可以维持膝关节的稳定性,为移植物的腱-骨愈合提供先决条件。尽管很多临床工作人员将富血小板血浆应用到术后关节注射,但是它的有效性还需要进一步验证,况且富血小板血浆促进腱-骨愈合的分子机制也不清楚。随着科学技术的飞速发展,多种多样的生物材料相应而生,生物材料的合成技术日益成熟,在很多动物实验中,生物材料促进移植物愈合的有效性已得到证实,将其应用到临床也指日可待。基因和干细胞治疗是最前沿的技术,很多人对它们分子机制的研究有了进展性突破,也在动物模型中也验证了其有效性,但目前还没有应用于临床中,可见基因和干细胞治疗在未来会有广阔的前景。随着医疗技术的发展和科学技术的进步,将会产生更多促进移植物腱-骨愈合的方法。

| [1] DELLA VILLA F, BUCKTHORPE M, GRASSI A, et al. Systematic video analysis of ACL injuries in professional male football (soccer): injury mechanisms, situational patterns and biomechanics study on 134 consecutive cases. Br J Sports Med. 2020;54(23):1423-1432. [2] PAUDEL Y R, SOMMERFELDT M, VOAKLANDER D. Increasing incidence of anterior cruciate ligament reconstruction: a 17-year population-based study. Knee Surg Sports Traumatol Arthrosc. 2023;31(1):248-255. [3] 杨金江,吴杰尹,合勇等.解剖单束与传统单束重建前交叉韧带的临床疗效及分析[J].临床和实验医学杂志,2021,20(9):968-972. [4] NAKAMURA T, KOGA H, OTABE K, et al. Comparison of three approaches for femoral tunnel during double-bundle anterior cruciate ligament reconstruction: a case controlled study. J Orthop Sci. 2019;24(1):147-152. [5] TRAN TD, TRAN QL. A cadaveric study on the anatomy of anterior cruciate ligament in vietnamese adults. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2018;14:22-25. [6] ELKIN JL, ZAMORA E, GALLO RA. Combined anterior cruciate ligament and medial collateral ligament knee injuries: anatomy, diagnosis, management recommendations, and return to sport. Curr Rev Musculoskelet Med. 2019; 12(2):239-244. [7] KRAEUTLER M, WOLSKY R, VIDAL A, et al. Anatomy and biomechanics of the native and reconstructed anterior cruciate ligament: surgical implications. J Bone Joint Surg Am. 2017;99(5):438-445. [8] KOC BB, JANSEN EJP, VAN DIJK P, et al. Mechanoreceptors observed in a ligamentous structure between the posterior horn of the lateral meniscus and the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2021;29(6):1701-1708. [9] LANDIS SE, BAKER RT, SEEGMILLER JG. Non-contact anterior cruciate ligament and lower extremity injury risk prediction using functional movement screen and knee abduction moment: an epidemiological observation of female intercollegiate athletes. Int J Sports Phys Ther. 2018; 13(6):973-984. [10] DIERMEIER T, ROTHRAUFF B, ENGEBRETSEN L, et al. Treatment after anterior cruciate ligament injury: panther symposium ACL treatment consensus group. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2390-2402. [11] LAROSE G, LEITER J, PEELER J, et al. Quality of life during the wait for ruptured anterior cruciate ligament reconstruction: a randomized controlled trial. Can J Surg. 2022;65(2):E269-E274. [12] SNOEKER BA, ROEMER FW, TURKIEWICZ A, et al. Does early anterior cruciate ligament reconstruction prevent development of meniscal damage? Results from a secondary analysis of a randomised controlled trial. Br J Sports Med. 2020;54(10):612-617. [13] WIRTH W, ECKSTEIN F, CULVENOR AG, et al. Early anterior cruciate ligament reconstruction does not affect 5 year change in knee cartilage thickness: secondary analysis of a randomized clinical trial. Osteoarthritis Cartilage. 2021;29(4):518-526. [14] REIJMAN M, EGGERDING V, VAN ES E, et al. Early surgical reconstruction versus rehabilitation with elective delayed reconstruction for patients with anterior cruciate ligament rupture: COMPARE randomised controlled trial. Bmj. 2021;372:375. [15] MAHAPATRA P, HORRIAT S, ANAND B. Anterior cruciate ligament repair - past, present and future. J Exp Orthop. 2018;5(1):20. [16] SCHLIEMANN B, LENSCHOW S, DOMNICK C, et al. Knee joint kinematics after dynamic intraligamentary stabilization: cadaveric study on a novel anterior cruciate ligament repair technique. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1184-1190. [17] HOOGESLAG RAG, BROUWER RW, BOER BC, et al. Acute anterior cruciate ligament rupture: repair or reconstruction? two-year results of a randomized controlled clinical trial. Am J Sports Med. 2019;47(3):567-577. [18] KöSTERS C, GLASBRENNER J, SPICKERMANN L, et al. Repair with dynamic intraligamentary stabilization versus primary reconstruction of acute anterior cruciate ligament tears: 2-year results from a prospective randomized study. Am J Sports Med. 2020;48(5):1108-1116. [19] HOOGESLAG R A G, HUIS IN ‘T VELD R, BROUWER R W, et al. Acute anterior cruciate ligament rupture: repair or reconstruction? Five-year results of a randomized controlled clinical trial. Am J Sports Med. 2022;50(7): 1779-1787. [20] GLASBRENNER J, RASCHKE M J, KITTL C, et al. Comparable instrumented knee joint laxity and patient-reported outcomes after ACL repair with dynamic intraligamentary stabilization or ACL reconstruction: 5-year results of a randomized controlled trial. Am J Sports Med. 2022;50(12):3256-3264. [21] PEñA E, CALVO B, MARTINEZ M, et al. Influence of the tunnel angle in ACL reconstructions on the biomechanics of the knee joint. Clinical biomechanics (Bristol, Avon). 2006;21(5):508-516. [22] AGA C, RISBERG MA, FAGERLAND MW, et al. No difference in the KOOS quality of life subscore between anatomic double-bundle and anatomic single-bundle anterior cruciate ligament reconstruction of the knee: a prospective randomized controlled trial with 2 years’ follow-up. Am J Sports Med. 2018;46(10):2341-2354. [23] IRRGANG JJ, TASHMAN S, PATTERSON CG, et al. Anatomic single vs. double-bundle ACL reconstruction: a randomized clinical trial-Part 1: clinical outcomes. Knee Surg Sports Traumatol Arthrosc. 2021;29(8):2665-2675. [24] AKMEŞE R, YOĞUN Y, KüçüKKARAPINAR İ, et al. Radiological maturation and clinical results of double-bundle and single-bundle anterior cruciate ligament reconstruction. A 5-year prospective case-controlled trial. Arch Orthop Trauma Surg. 2022;142(6):1125-1132. [25] SEPPäNEN A, SUOMALAINEN P, HUHTALA H, et al. Double bundle ACL reconstruction leads to better restoration of knee laxity and subjective outcomes than single bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2022;30(5):1795-1808. [26] LUBOWITZ JH. No-tunnel anterior cruciate ligament reconstruction: the transtibial all-inside technique. Arthroscopy. 2006;22(8):900.e1-11. [27] NUELLE CW, BALLDIN BC, SLONE HS. All-inside anterior cruciate ligament reconstruction. Arthroscopy. 2022;38(8):2368-2369. [28] YASEN S, BORTON Z, EYRE-BROOK A, et al. Clinical outcomes of anatomic, all-inside, anterior cruciate ligament (ACL) reconstruction. Knee. 2017; 24(1):55-62. [29] LIN R, ZHONG Q, WU X, et al. Randomized controlled trial of all-inside and standard single-bundle anterior cruciate ligament reconstruction with functional, MRI-based graft maturity and patient-reported outcome measures. BMC Musculoskelet Disord. 2022;23(1):289. [30] PAUTASSO A, CAPELLA M, BARBERIS L, et al. All-inside technique in ACL reconstruction: mid-term clinical outcomes and comparison with AM technique (Hamstrings and BpTB grafts). Eur J Orthop Surg Traumatol. 2021;31(3):465-472. [31] KOULOUMENTAS P, KAVROUDAKIS E, CHARALAMPIDIS E, et al. Superior knee flexor strength at 2 years with all-inside short-graft anterior cruciate ligament reconstruction vs a conventional hamstring technique. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3592-3598. [32] BAAWA-AMEYAW J, PLASTOW R, BEGUM F, et al. Current concepts in graft selection for anterior cruciate ligament reconstruction. EFORT Open Rev. 2021;6(9):808-815. [33] YANG X, WANG F, HE X, et al. Network meta-analysis of knee outcomes following anterior cruciate ligament reconstruction with various types of tendon grafts. Int Orthop. 2020;44(2):365-380. [34] SUN K, TIAN S, ZHANG J, et al. Anterior cruciate ligament reconstruction with BPTB autograft, irradiated versus non-irradiated allograft: a prospective randomized clinical study. Knee Surg Sports Traumatol Arthrosc. 2009;17(5):464-474. [35] DIERMEIER T, TISHERMAN R, HUGHES J, et al. Quadriceps tendon anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2644-2656. [36] LIND M, NIELSEN TG, SOERENSEN OG, et al. Quadriceps tendon grafts does not cause patients to have inferior subjective outcome after anterior cruciate ligament (ACL) reconstruction than do hamstring grafts: a 2-year prospective randomised controlled trial. Br J Sports Med. 2020;54(3):183-187. [37] HORSTMANN H, PETRI M, TEGTBUR U, et al. Quadriceps and hamstring tendon autografts in ACL reconstruction yield comparably good results in a prospective, randomized controlled trial. Arch Orthop Trauma Surg. 2022;142(2):281-289. [38] BARIé A, SPRINCKSTUB T, HUBER J, et al. Quadriceps tendon vs. patellar tendon autograft for ACL reconstruction using a hardware-free press-fit fixation technique: comparable stability, function and return-to-sport level but less donor site morbidity in athletes after 10 years. Arch Orthop Trauma Surg. 2020;140(10):1465-1474. [39] TRIEB K, BLAHOVEC H, BRAND G, et al. In vivo and in vitro cellular ingrowth into a new generation of artificial ligaments. Eur Surg Res. 2004;36(3):148-151. [40] 翟昕元,林小风.LARS人工韧带重建前交叉韧带:生物相容性及与骨组织的愈合[J].中国组织工程研究,2017,21(16):2565-2569. [41] CHEN T, ZHANG P, CHEN J, et al. Long-term outcomes of anterior cruciate ligament reconstruction using either synthetics with remnant preservation or hamstring autografts: a 10-year longitudinal study. Am J Sports Med. 2017;45(12):2739-2750. [42] XU C, LIU T, WANG M, et al. Comparison of proprioception recovery following anterior cruciate ligament reconstruction using an artificial graft versus an autograft. BMC Musculoskelet Disord. 2022;23(1):1056. [43] SINAGRA ZP, KOP A, PABBRUWE M, et al. Foreign body reaction associated with artificial lars ligaments: a retrieval study. Orthop J Sports Med. 2018; 6(12):2325967118811604. [44] LI S, WANG S, LIU W, et al. Current strategies for enhancement of the bioactivity of artificial ligaments: a mini-review. J Orthop Translat. 2022;36: 205-215. [45] MORETTI L, BIZZOCA D, CASSANO G, et al. Graft intra-articular remodeling and bone incorporation in acl reconstruction: the state of the art and clinical implications. J Clin Med. 2022;11(22):6704. [46] YOO J, YANG E. Clinical results of an arthroscopic modified Brostrom operation with and without an internal brace. J Orthop Traumatol. 2016; 17(4):353-360. [47] HAMIDO F, HABIBA AA, MARWAN Y, et al. Anterolateral ligament reconstruction improves the clinical and functional outcomes of anterior cruciate ligament reconstruction in athletes. Knee Surg Sports Traumatol Arthrosc. 2021;29(4):1173-1180. [48] ZUK P, ZHU M, ASHJIAN P, et al. Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell. 2002;13(12):4279-4295. [49] WANG C, HU Y, ZHANG S, et al. Application of stem cell therapy for ACL graft regeneration. Stem Cells Int. 2021;2021:6641818. [50] XU Y, ZHANG W, WANG L, et al. Stem cell therapies in tendon-bone healing. World J Stem Cells. 2021;13(7):753-775. [51] LIM J, HUI J, LI L, et al. Enhancement of tendon graft osteointegration using mesenchymal stem cells in a rabbit model of anterior cruciate ligament reconstruction. Arthroscopy. 2004;20(9):899-910. [52] UYSAL A, MIZUNO H. Tendon regeneration and repair with adipose derived stem cells. Curr Stem Cell Res Ther. 2010;5(2):161-167. [53] ALENTORN-GELI E, SEIJAS R, MARTíNEZ-DE LA TORRE A, et al. Effects of autologous adipose-derived regenerative stem cells administered at the time of anterior cruciate ligament reconstruction on knee function and graft healing. J Orthop Surg (Hong Kong). 2019;27(3):2309499019867580. [54] FRANKLIN A, GI MIN J, ODA H, et al. Homing of adipose-derived stem cells to a tendon-derived hydrogel: a potential mechanism for improved tendon-bone interface and tendon healing. J Hand Surg Am. 2020;45(12): 1180.e1-1180.e12. [55] XIE H, FU Z, ZHONG M, et al. Effects of remnant preservation in anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Front Surg. 2022;9:952930. [56] VAN KEULEN L, HOOGESLAG R, BROUWER R, et al. The importance of continuous remnant preservation in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2022;30(5):1818-1827. [57] KOSY J, MANDALIA V. Anterior cruciate ligament mechanoreceptors and their potential importance in remnant-preserving reconstruction: a review of basic science and clinical findings. J Knee Surg. 2018;31(8):736-746. [58] MEHRABANI D, SEGHATCHIAN J, ACKER J. Platelet rich plasma in treatment of musculoskeletal pathologies. Transfus Apher Sci. 2019;58(6):102675. [59] MCROBB J, KAMIL K, AHMED I, et al. Influence of platelet-rich plasma (PRP) analogues on healing and clinical outcomes following anterior cruciate ligament (ACL) reconstructive surgery: a systematic review. Eur J Orthop Surg Traumatol. 2023;33(2):225-253. [60] ZHU T, ZHOU J, HWANG J, et al. Effects of platelet-rich plasma on clinical outcomes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Orthop J Sports Med. 2022;10(1): 23259671211061535. [61] CAO Y, WAN Y. Effectiveness of platelet-rich plasma in anterior cruciate ligament reconstruction: a systematic review of randomized controlled trials. Orthop Surg. 2022;14(10):2406-2417. [62] WAHED S, DUNSTAN C, BOUGHTON P, et al. Functional ultra-high molecular weight polyethylene composites for ligament reconstructions and their targeted applications in the restoration of the anterior cruciate ligament. Polymers (Basel). 2022;14(11):2189. [63] LIAO H, YU H, SONG W, et al. Amorphous calcium phosphate nanoparticles using adenosine triphosphate as an organic phosphorus source for promoting tendon-bone healing. J Nanobiotechnology. 2021;19(1):270. [64] ZHAO S, ZHAO J, DONG S, et al. Biological augmentation of rotator cuff repair using bFGF-loaded electrospun poly(lactide-co-glycolide) fibrous membranes. Int J Nanomedicine. 2014;9:2373-2385. [65] WANG J, XU J, FU W, et al. Biodegradable magnesium screws accelerate fibrous tissue mineralization at the tendon-bone insertion in anterior cruciate ligament reconstruction model of rabbit. Sci Rep. 2017;7:40369. [66] ZHAO X, ZHOU Y, LI J, et al. Opportunities and challenges of hydrogel microspheres for tendon-bone healing after anterior cruciate ligament reconstruction. J Biomed Mater Res B Appl Biomater. 2022;110(2):289-301. [67] HAO Z, WANG S, ZHANG X, et al. Stem cell therapy: a promising biological strategy for tendon-bone healing after anterior cruciate ligament reconstruction. Cell Prolif. 2016;49(2):154-162. [68] CHEN B, LI B, QI Y, et al. Enhancement of tendon-to-bone healing after anterior cruciate ligament reconstruction using bone marrow-derived mesenchymal stem cells genetically modified with bFGF/BMP2. Sci Rep. 2016;6:25940. [69] XU Z, LI S, WAN L, et al. Role of low-intensity pulsed ultrasound in regulating macrophage polarization to accelerate tendon-bone interface repair. J Orthop Res. 2022. doi:10.1002/jor.25454. [70] ARIMURA H, SHUKUNAMI C, TOKUNAGA T, et al. TGF-β1 improves biomechanical strength by extracellular matrix accumulation without increasing the number of tenogenic lineage cells in a rat rotator cuff repair model. Am J Sports Med. 2017;45(10):2394-2404. [71] KIM J, KIM H, KIM S, et al. Enhancement of tendon-bone healing with the use of bone morphogenetic protein-2 inserted into the suture anchor hole in a rabbit patellar tendon model. Cytotherapy. 2014;16(6):857-867. [72] HAN L, FANG W, JIN B, et al. Enhancement of tendon-bone healing after rotator cuff injuries using combined therapy with mesenchymal stem cells and platelet rich plasma. Eur Rev Med Pharmacol Sci. 2019;23(20): 9075-9084. |
| [1] | 袁维勃, 刘 婵, 余丽梅. 肝脏类器官在肝脏疾病模型与移植治疗中的应用潜力[J]. 中国组织工程研究, 2025, 29(8): 1684-1692. |
| [2] | 王 娟, 王广兰, 左会武. 运动疗法对前交叉韧带重建后康复疗效影响的网状Meta分析[J]. 中国组织工程研究, 2025, 29(8): 1714-1726. |
| [3] | 孙玉婷, 吴家媛, 张 剑. 影响牙髓干细胞成骨及成牙本质分化的相关物理因素及作用机制[J]. 中国组织工程研究, 2025, 29(7): 1531-1540. |
| [4] | 喻 婷, 吕冬梅, 邓 浩, 孙 涛, 程 钎. 淫羊藿苷预处理增强人牙周膜干细胞对M1型巨噬细胞的影响[J]. 中国组织工程研究, 2025, 29(7): 1328-1335. |
| [5] | 杨治航, 孙祖延, 黄文良, 万 喻, 陈仕达, 邓 江. 神经生长因子促进兔骨髓间充质干细胞软骨分化并抑制肥大分化[J]. 中国组织工程研究, 2025, 29(7): 1336-1342. |
| [6] | 胡涛涛, 刘 兵, 陈 诚, 殷宗银, 阚道洪, 倪 杰, 叶凌霄, 郑祥兵, 严 敏, 邹 勇. 过表达神经调节蛋白1的人羊膜间充质干细胞促进小鼠皮肤创面愈合[J]. 中国组织工程研究, 2025, 29(7): 1343-1349. |
| [7] | 金 凯, 唐 婷, 李美乐, 谢裕安. 人脐带间充质干细胞条件培养基及外泌体对肝癌细胞增殖、迁移、侵袭和凋亡的影响[J]. 中国组织工程研究, 2025, 29(7): 1350-1355. |
| [8] | 李帝均, 酒精卫, 刘海峰, 闫 磊, 李松岩, 王 斌. 明胶三维微球装载人脐带间充质干细胞修复慢性肌腱病[J]. 中国组织工程研究, 2025, 29(7): 1356-1362. |
| [9] | 娄 国, 张 敏, 付常喜. 8周运动预适应增强脂肪干细胞治疗心肌梗死大鼠的效果[J]. 中国组织工程研究, 2025, 29(7): 1363-1370. |
| [10] | 刘 琪, 李林臻, 李玉生, 焦泓焯, 杨 程, 张君涛. 淫羊藿苷含药血清促进3种细胞共培养体系中软骨细胞增殖和干细胞成软骨分化[J]. 中国组织工程研究, 2025, 29(7): 1371-1379. |
| [11] | 艾克帕尔·艾尔肯, 陈晓涛, 吾凡别克·巴合提. 成骨诱导人牙周膜干细胞来源外泌体促进炎症微环境下人牙周膜干细胞成骨分化[J]. 中国组织工程研究, 2025, 29(7): 1388-1394. |
| [12] | 德 吉, 索朗达, 魏宇辰, 王 斌, 阿旺措吉, 仁青措姆, 崔久增, 张 磊, 巴 贵. 藏西北绒山羊子宫内膜容受性相关基因和可变剪接事件的综合分析[J]. 中国组织工程研究, 2025, 29(7): 1429-1436. |
| [13] | 章镇宇, 梁秋健, 杨 军, 韦相宇, 蒋 捷, 黄林科, 谭 桢. 新橙皮苷治疗骨质疏松症的靶点及对骨髓间充质干细胞成骨分化的作用[J]. 中国组织工程研究, 2025, 29(7): 1437-1447. |
| [14] | 王 咪, 马书杰, 刘 杨, 齐 瑞. 缺血性脑卒中铁死亡特征基因NFE2L2的鉴定与验证[J]. 中国组织工程研究, 2025, 29(7): 1466-1474. |
| [15] | 谢刘刚, 崔书克, 郭楠楠, 李遨宇, 张菁瑞. 干细胞治疗阿尔茨海默病的研究热点与前沿[J]. 中国组织工程研究, 2025, 29(7): 1475-1485. |
前交叉韧带损伤的症状表现为膝关节疼痛、膝关节不稳、膝关节肿胀、膝关节活动异常,还有一部分人表现为典型的关节绞锁。如果延误治疗时机,可能会损伤膝关节周围韧带、半月板和关节内软骨,甚至会导致继发性骨关节炎的发生[3]。
虽然很多文章已经研究了前交叉韧带损伤的治疗进展,但是他人文章的内容不全面或者侧重点不同,例如:①手术方式不全面,缺少前交叉韧带修复术和全内修复术的介绍;②移植物的阐述不全面,没有分开对比各种移植物的优缺点,对最近讨论较多的股四头肌肌腱和人工韧带介绍不详细;③文章侧重介绍术后康复,且没有写出促进移植物愈合的方法。目前对于前交叉韧带损伤的治疗以关节镜下前交叉韧带重建手术为主[4],但是早期或延迟手术仍然是争议的话题。尽管传统的手术方式已经很成熟,然而近几年前交叉韧带修复术和全内前交叉韧带重建逐渐引起临床人员的关注。另外,关于股四头肌肌腱和人工韧带的移植物选择、促进移植物愈合的方法等问题还有待进一步解决。
文章总结了前交叉韧带损伤的手术时机(早期或延迟手术)、手术方式(前交叉韧带修复术和全内重建技术)、移植物选择(主要讲述股四头肌肌腱移植物和人工合成移植物的修复效果、生物相容性和并发症等)和促进移植物愈合方法(干细胞促进腱-骨愈合机制、富血小板血浆、生物材料、基因治疗等)的最新研究进展,为前交叉韧带损伤寻找新的治疗方向。 中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
1.1.1 检索人及检索时间 由第一作者在2023-01-18进行检索。
1.1.2 检索文献时限 2017年1月到2023年1月。
1.1.3 检索数据库 包括PubMed、中国知网、万方数据、维普、SinoMed、ScienceDirect、Springer及Cochrane 图书馆数据库。
1.1.4 检索词 中文检索词为“前交叉韧带损伤、前交叉韧带重建、治疗、肌腱移植、肌腱愈合”;英文检索词为“Anterior cruciate ligament injury,Anterior cruciate ligament reconstruction,therapy,Tendon transplantation,Tendon healing”。
1.1.5 检索文献类型 包括中文及英文综述、研究原著、病例报告和Meta分析。
1.1.6 手工检索情况 无。
1.1.7 检索策略 以PubMed数据库检索策略为例,检索式:((((“Anterior Cruciate Ligament Injuries”[Mesh]) OR ((ACL Injuries[Title/Abstract]) OR (ACL Injury[Title/Abstract]) OR (Injuries, ACL[Title/Abstract]) OR (Injury, ACL[Title/Abstract]) OR (Anterior Cruciate Ligament Injury[Title/Abstract]) OR (Anterior Cruciate Ligament Tear[Title/Abstract]) OR (ACL Tears[Title/Abstract]) OR (ACL Tear[Title/Abstract]) OR (Tear, ACL[Title/Abstract]) OR (Tears, ACL[Title/Abstract]) OR (Anterior Cruciate Ligament Tears[Title/Abstract]))) OR (anterior cruciate ligament reconstruction)) AND ((tendon transplantation) OR (tendon healing) OR (therapy))。中文以万方数据库为例,检索式为:((关键词=交叉韧带损伤) OR (关键词=前交叉韧带重建)) AND ((关键词=治疗) OR (关键词=肌腱移植) OR (关键词=肌腱愈合))。
1.1.8 检索文献量 初步检索到3 594篇文献。
1.2 入组标准
1.2.1 纳入标准 ①与前交叉韧带损伤、前交叉韧带重建、肌腱移植、肌腱愈合相关性高的文献;②主要讨论前交叉韧带损伤的早期与延迟重建、手术方式、不同移植物结局比较、促进移植物愈合方法的文献;③证据充足、结果客观及影响因子相对较高的文献。
1.2.2 排除标准 排除观点过时、内容重复、无法获取全文、观点不明确以及不相关的文献。
1.3 文献质量评估及数据的提取 通过以上所提到的数据库检索,总共检索到3 602篇参考文献,其中PubMed(n=1 154)、中国知网(n=79)、万方数据(n=581)、维普(n=317)、SinoMed(n=918)、Cochrane 图书馆(n=553)。经 2 位作者讨论,并按照上面的选入标准为准则,最终获得 60篇(PubMed 58篇、中国知网 2篇)内容上有代表性的文献,再通过阅读这60篇文献,从它们引用的文献中选取相关性较大的12篇文献,最终纳入72篇文献,英文文献70篇(英文作者文献56篇,中文作者文献14篇),中文文献2篇。文章的参考文献以英文文献为主,中文文献为辅。文献检索流程图,见图1。
3.2 作者综述区别于他人他篇的特点 ①收集了近年的文献,比较全面的总结了前交叉韧带损伤的最新治疗进展:a.讨论了早期与延迟治疗的比较;b.对比了两种新术式(动态内稳定修复术和全内重建)与传统术式的优劣势;c.详细总结了各种移植物的优缺点(尤其对近几年研究较多的股四头肌肌腱和LARS韧带做了全面阐述);d.在促进移植物愈合的方法上,分析了富血小板血浆的临床疗效,对临床上使用较多的外侧复合体加强和保留残端重建也进行了探讨,介绍了基因、干细胞和生物材料三者促进腱-骨愈合的可能机制。②他人总结前交叉韧带研究进展的文章,存在内容不够新颖或不够全面的问题,在现阶段本文具有全面性和新颖性。③文章中有快速阅读图例、各种移植物优缺点的图解、干细胞促进腱-骨愈合的机制图,也添加了关于各研究的表格,使文章阅读更加简洁明了。
3.3 综述的局限性 ①文章研究的内容比较广泛,各个部分的文献量较少,而且所纳入的文献包括随机对照试验、病例对照、综述和Meta分析,文章类型杂乱,会导致结论的偏差;②文章仅收集了近7年的相关文献,时间跨度较短,没有对研究内容追根溯源,可能对疾病的了解不够深入;③可能由于纳入文献的干预手段不同、测量法不同、评价量表的主观性、术后康复锻炼的不同、术后随访时间的不同等原因,导致结果的差异;④该研究没有讨论前交叉韧带不同部位或者不同程度损伤该如何治疗、前交叉韧带损伤并发半月板损伤和软骨损伤的手术方式及时机、术后康复、术后心理治疗等内容。
3.4 综述的重要意义 文章通过查阅最近年的文献,分别从前交叉韧带损伤的手术时机、手术方式、移植物选择和促进移植物愈合方法4个方面,比较系统地阐述了前交叉韧带损伤的最新治疗进展,为前交叉韧带损伤寻找新的治疗方向,给基础研究和临床研究提供了参考。
3.5 课题专家组对未来的建议 ①临床工作人员应该加强技术创新,进行更多的临床试验,了解新术式的临床适用性,在未来探索出安全性高、创伤性小、痛苦少的手术方式。②组织工程的科研人员要进行更广泛、更科学、更严谨的基因、分子、细胞、动物及临床试验研究,掌握基因和干细胞的分子机制,推动干细胞和基因应用于临床的进程。③加强多学科、多领域的合作,在未来筛选出在生物相容性、生物力学和促进腱-骨愈合等方面均有优势的物理化学材料和生物材料。 中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
 #br#
#br#
文题释义:
前交叉韧带:是膝关节的韧带之一,起源于胫骨平台前内侧,在关节腔内沿着后内方走行,越过后交叉韧带前方,向上止于股骨外侧髁的后内侧。也有研究表明前交叉韧带分为前内侧束和后外侧束两束,可以防止胫骨前移和过度旋转,保持膝关节运动的正常生物力学,以防半月板损伤。前交叉韧带损伤:当人体旋转、切割和跳跃时,膝关节处于轻度屈曲外翻位,此时再加上股四头肌剧烈收缩,便可使胫骨近端受到较大剪切力,附着于胫骨近端的前交叉韧带不能承受其本身的最大应力,导致前交叉韧带撕裂甚至断裂。
前交叉韧带在维持膝关节正常结构和功能方面起着不可或缺的作用,前交叉韧带损伤是膝关节运动损伤中比较常见的一种类型,如果治疗不当,可能会损伤膝关节周围韧带、半月板和关节内软骨,甚至会导致继发性骨关节炎。近些年,对于前交叉韧带损伤的治疗日益成熟,但是,临床上对于前交叉韧带损伤的手术时机、手术方式的选择、移植物的选择、促进移植物愈合的方法等问题还存在争议。
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||