中国组织工程研究 ›› 2025, Vol. 29 ›› Issue (24): 5179-5186.doi: 10.12307/2025.736
• 组织构建综述 tissue construction review • 上一篇 下一篇
肌骨交互机制视域下肌骨退行性疾病及损伤的治疗与修复
张兴宇,吴 斗,赵恩哲,宋旭彬,张晓仑
- 山西医科大学第三医院 (山西白求恩医院,山西医学科学院,同济山西医院),山西省太原市 030032
-
收稿日期:2024-09-21接受日期:2024-10-31出版日期:2025-08-28发布日期:2025-01-25 -
通讯作者:吴斗,博士,主任医师,山西医科大学第三医院 (山西白求恩医院,山西医学科学院,同济山西医院),山西省太原市 030032 -
作者简介:张兴宇,男,1997年生,山西省忻州市人,汉族,硕士,主要从事创伤骨科、骨质疏松等方面的研究。 -
基金资助:山西省基础研究计划项目(202303021222326),项目负责人:赵恩哲
Treatment and repair of musculoskeletal degenerative diseases and injuries from the perspective of muscle-bone crosstalk mechanism
Zhang Xingyu, Wu Dou, Zhao Enzhe, Song Xubin, Zhang Xiaolun
- Third Hospital of Shanxi Medical University,Shanxi Bethune Hospital,Shanxi Academy of Medical Sciences,Tongji Shanxi Hospital,Taiyuan030032,Shanxi Province,China
-
Received:2024-09-21Accepted:2024-10-31Online:2025-08-28Published:2025-01-25 -
Contact:Wu Dou, PhD, Chief physician, Third Hospital of Shanxi Medical University,Shanxi Bethune Hospital,Shanxi Academy of Medical Sciences,Tongji Shanxi Hospital,Taiyuan030032,Shanxi Province,China -
About author:Zhang Xingyu, MS, Third Hospital of Shanxi Medical University,Shanxi Bethune Hospital,Shanxi Academy of Medical Sciences,Tongji Shanxi Hospital,Taiyuan030032,Shanxi Province,China -
Supported by:Shanxi Province Basic Research Program Project, No. 202303021222326 (to ZEZ)
摘要:
文题释义:
肌骨交互:肌肉和骨骼通过机械、生化、干细胞作用相互影响,达到共调控的平衡状态。
肌骨退行性疾病及损伤:肌骨退行性疾病主要包括骨质疏松症、肌少症、肌少-骨质疏松症,肌肉骨骼损伤主要包括肌肉挫伤、肌肉撕裂、骨折、脆性骨折等。
背景:骨骼与肌肉退行性病变引发的多种疾病是老年人身体功能和运动能力下降、脆性骨折等不良预后的重要原因,严重影响老年人的身体健康和生活质量。
目的:综述肌骨交互作用机制及相关疾病病因、预防、治疗的研究进展。
方法:检索CNKI、万方和PubMed 数据库中2014-2024年发表的相关文献,中文检索词为“肌骨交互,肌肉骨骼系统,组织通讯,肌因子,骨因子,肌少-骨质疏松症,肌少症,骨质疏松症,骨再生,成纤维脂肪祖细胞”,英文检索词为“muscle-bone crosstalk,musculoskeletal system,inter-tissue communication,Myokines,Osteokines,Osteosarcopenia,Sarcopenia,Osteoporosis,Bone Regeneration,fibro-adipogenic progenitors”。通过阅读文章剔除研究内容与文章主题关系不大、侧重点不突出、内容观点陈旧的文献,最终纳入94篇文献进行归纳总结。
结果与结论:肌肉与骨骼的机械性交互、分泌因子交互和干细胞交互对肌骨系统的代谢及再生调控意义重大。针对肌因子(肌生成抑制素、鸢尾素等)和骨因子(核因子κB受体活化因子配体、硬化蛋白等)生化信号的系统干预可以改善骨骼肌和骨的质量和功能,对骨折愈合同样有积极效果。近年来发现肌骨系统中相关干细胞可进行交互作用,尤以成纤维脂肪祖细胞等肌祖细胞的活化对骨的生长、修复和再生影响显著。针对肌骨交互机制的研究可以对相关疾病的病因、预防、治疗提供思路,然而临床还未有对肌骨共病行之有效的治疗方法,大部分研究停留在细胞及动物实验阶段,因此未来还需要进行大量研究,逐步由实验向临床迈进,开发更具针对性的疗法及药物。
中国组织工程研究杂志出版内容重点:组织构建;骨细胞;软骨细胞;细胞培养;成纤维细胞;血管内皮细胞;骨质疏松;组织工程
中图分类号:
引用本文
张兴宇, 吴 斗, 赵恩哲, 宋旭彬, 张晓仑. 肌骨交互机制视域下肌骨退行性疾病及损伤的治疗与修复[J]. 中国组织工程研究, 2025, 29(24): 5179-5186.
Zhang Xingyu, Wu Dou, Zhao Enzhe, Song Xubin, Zhang Xiaolun. Treatment and repair of musculoskeletal degenerative diseases and injuries from the perspective of muscle-bone crosstalk mechanism[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5179-5186.
2.2 肌骨的机械交互作用 肌骨的机械交互作用机制是最早被认识并研究的。在解剖学上,骨骼肌通过肌腱与骨骼和关节上牢固的附着点连接,将骨骼节段转变为力学杠杆系统[23],骨骼肌在神经系统指令下完成收缩运动[24];在微观上,肌丝中的肌动蛋白和肌球蛋白异步滑动,表现为宏观的肌肉收缩,从而在关节处产生各向运动的力矩,使骨骼能够多向运动,使人体完成站立、行走、跳跃、面部表情、咀嚼等运动[25]。
沃尔夫定律指出,骨骼的大小和几何形状会根据施加的应力而变化[13],后续完善的“机械稳定器”理论和“犹他州骨骼生理学范式”指出,肌肉收缩产生的应力会诱发其附着骨骼中的合成转换代谢活动[15]。骨细胞是对机械刺激最敏感的细胞,位于骨基质中,被认为是骨重建的主要调节者。一旦成骨细胞被矿化的细胞外基质包围,它们就向骨细胞分化。当骨基质受到机械负荷时,骨细胞可以检测到应力变化。应力检测功能由骨细胞形成的腔隙性小管系统承担,骨细胞可感受伴随小管液快速流动的流体剪切应力和周围电解质浓度,将机械应变转化为生化信号,以募集破骨细胞或成骨细胞对骨进行重塑[26]。在抗阻训练中,施加在骨骼肌上的负荷会作用到骨骼上,这不仅会促进肌肉蛋白质的合成,还会发出高能量需求信号以诱导骨骼的形成,这为肌骨生物力学的相互作用提供了证据[2]。
肌肉和骨骼通过机械负荷相互作用,导致各自的重塑。其中,骨量的发育和维持在很大程度上取决于肌肉产生的机械负荷[15]。骨骼肌质量及肌肉横截面积与不同身体部位的骨量密度呈正相关[27]。从骨的发育来看,骨骼的形状主要由骨骼肌产生的机械负荷决定,在失去骨骼肌机械负荷的发育环境下会导致骨骼发育畸形,失去其固有的生理形状。在一项实验中,小鼠胚胎被敲除骨骼肌发育基因后,骨骼在缺乏骨骼肌附着且无骨骼肌主动收缩的环境下进行发育,该表型的特征是骨矿化严重受损、骨形态改变,表现为异常骨缺损、骨融合、骨发育不全;该研究还提出子宫中运动减少的婴儿会出现暂时性的软骨和关节发育不良[28]。骨骼肌机械负荷还会影响骨隆起的发育,在没有肌肉活动的情况下,骨的生理性隆起会显著减少,甚至完全消失[29]。骨骼肌对骨骼的生长也产生影响,可加剧骨骼生长缺陷。如青少年特发性脊柱侧凸中,凸侧强健的椎旁肌会降低同侧脊柱的机械负荷,从而促进骨骼生长,而凹侧较弱的椎旁肌会增加脊柱负荷并阻碍凹侧骨骼生长,导致弯曲加剧[12]。
虽然肌肉和骨骼之间的相互作用是双向的,但一些观察和研究表明,肌肉相较骨骼在交互协调中起着先行主导作用,在肌骨交互中肌肉变化较骨骼变化较先发生。在一项小鼠后肢悬吊失用实验中,证实股骨和胫骨皮质厚度的减少比腓肠肌和股四头肌质量的降低晚7 d[30]。另一项队列研究表明,从青少年到成人的成长过程中瘦体质量变化先于全身骨密度和骨骼强度的变化[31]。肌萎缩和丢失是航天失重过程中一个难以避免生理过程,被称为失用性肌萎缩和骨丢失,也发生在神经肌肉疾病患者或卧床休息肢体制动的患者。在失重环境下,肌肉骨骼系统失去大量机械刺激,主要是姿势维持骨骼肌受到很大影响,较先发生退变。尽管在太空飞行中采取了运动对策,但仍会发生肌肉萎缩和骨质流失,当宇航员回归地面恢复正常重力时,他们的肌肉恢复速度是骨质恢复速度的6倍[32]。
2.3 肌骨的分泌因子交互
2.3.1 肌因子的交互作用 肌因子根据其在骨代谢中的作用可分为两类:骨形成因子和骨吸收因子。促进骨形成的因子包括鸢尾素、胰岛素样生长因子1、成纤维细胞生长因子2、骨形态发生蛋白1、脑源性神经营养因子、β-氨基异丁酸等;促进骨吸收的肌因子包括肌生长抑制素、白细胞介素等,这些肌因子在骨代谢、骨重建和骨再生中起关键作用[2]。
鸢尾素在肌骨交互的生物学效应中被广泛研究,它是纤连蛋白Ⅲ型结构域5蛋白水解裂解产生的片段,在运动过程中由骨骼肌生成,随后释放到血液循环中[33]。骨骼是鸢尾素的主要靶器官,鸢尾素通过增加骨形成和降低破骨细胞活性促进骨的合成代谢[34]。研究发现,肌肉减少症和骨质疏松症患者血清中的鸢尾素水平明显低于健康对照组,这表明鸢尾素对骨骼肌和骨骼疾病具有高度敏感性。年龄和机械刺激减少是骨质疏松症的重要因素,随着年龄的增长或肢体制动时间延长,血清鸢尾素水平也逐渐降低[35]。鸢尾素已被普遍认为是骨质疏松症、肌肉减少症和肌少-骨质疏松症的预测标志物[36]。
肌生成抑制素又称生长和分化因子8,属于转化生长因子β超家族,是骨骼肌和骨的负调节因子。研究表明,肌生长抑制素可抑制骨细胞来源外泌体miRNA-218的表达,增加抗骨形成代谢因子硬化蛋白、核因子κB受体活化因子配体的产生,以及促进Dickkopf相关蛋白1的产生,其为Dickkopf Wnt信号通路抑制剂[37]。肌肉生长抑制素可以靶向多种骨细胞,包括间充质干细胞、成骨细胞、骨细胞和破骨细胞[38]。肌肉生长抑制素抑制肌细胞的增殖和分化,与肌萎缩和损伤呈正相关。肌生成抑制素作用于骨可促进骨吸收,抑制骨生成[3]。据报道,在中年人群中,高肌肉生长抑制素水平与低皮质骨厚度以及低肌肉质量呈正相关[39]。
β-氨基异丁酸是一种骨骼肌在运动状态下分泌的肌因子,是缬氨酸或胸腺嘧啶的代谢物 [40]。β-氨基异丁酸的对映体L-β-氨基异丁酸可保护骨细胞免受氧化应激对线粒体功能的破坏,并最终保护骨量,遏制骨细胞的凋亡[41]。
胰岛素样生长因子1和成纤维细胞生长因子2可通过促进成骨细胞的增殖和分化,保持骨量,也是骨修复的强力因子[42]。胰岛素样生长因子1和成纤维细胞生长因子2由肌管分泌,在肌肉损伤后,肌瓣的伤口分泌物中存在高浓度的胰岛素样生长因子1,伴随局部成纤维细胞生长因子2释放增加[43]。最近发现,成纤维细胞生长因子2还可通过抑制骨硬化蛋白基因的信号转导对抗糖皮质激素对骨的吸收作用[44]。一项研究证明了卵泡刺激素结合蛋白1-转录因子EB-胰岛素样生长因子2转导通路与肌萎缩和骨丢失发病机制的联系,肌纤维中卵泡刺激素结合蛋白1的减少诱导转录因子EB的核转位,激活成纤维细胞生长因子2基因的转录和分泌,进而激活破骨细胞内的成纤维细胞生长因子2受体信号传导,刺激破骨细胞生成[22]。
白细胞介素家族的细胞因子大多是促炎递质,由全身多种细胞类型分泌。骨骼肌分泌几种白细胞介素,其中包括白细胞介素6、白细胞介素7和白细胞介素15。白细胞介素6可由肝脏合成,但运动时循环中激增的白细胞介素6由肌肉分泌,白细胞介素6 作用于成骨细胞以促进破骨细胞分化和骨钙素释放[45]。
2.3.2 骨因子的交互作用 骨因子可分为促进肌肉生长的骨因子和促进肌肉退化的骨因子,前者包括骨钙素等,后者包括硬化蛋白和核因子κB受体活化因子配体和转化生长因子β等[2]。
核因子κB受体活化因子配体是骨保护素/核因子κB受体活化因子配体/核因子κB 受体激活剂信号通路中必不可少的一环,主要位于成骨细胞和骨细胞中,核因子κB受体活化因子配体可以与其受体核因子κB 受体激活剂结合而激活下游各信号分子,包括集落刺激因子1受体和核因子κB受体,进而启动破骨细胞分化;另一方面,骨保护素是核因子κB受体活化因子配体的可溶性受体,可阻碍核因子κB受体活化因子配体和核因子κB 受体激活剂的结合,抑制破骨细胞生成 [37]。骨保护素/核因子κB受体活化因子配体/核因子κB 受体激活剂轴功能障碍或核因子κB受体活化因子配体的过表达会导致骨质疏松,而对其的抑制可逆转骨质疏松,增加骨量和强度。骨骼肌中同样表达核因子κB受体活化因子配体,其激活可抑制成肌细胞分化并诱导肌肉萎缩[46-47],
骨钙素是一种由成骨细胞分泌的激素,以羧化、欠羧化和未羧化形式存在于循环中。多项临床研究表明,运动后欠羧化骨钙素增加,欠羧化骨钙素可通过调控GPRC6A基因抑制破骨细胞的早期分化,从而阻止骨吸
收[48]。欠羧化骨钙素也与肌肉质量和功能有关,循环中的欠羧化骨钙素通过抑制肿瘤坏死因子α介导的下游信号通路来抑制炎症因子的表达,抑制肌萎缩[49]。有研究称白细胞介素6/成骨细胞/骨钙素信号传递是肌-骨-肌交互轴的新机制,肌释放白细胞介素6作用于成骨细胞后,激活核因子κB受体活化因子配体表达和促进成骨细胞分化,并释放骨钙素进入循环[45]。
硬化蛋白是由硬化蛋白基因表达的蛋白质,是一种由成熟骨细胞分泌的糖蛋白,可作为骨形成的拮抗剂。硬化蛋白不仅抑制骨形态发生蛋白诱导的Smad蛋白磷酸化,还阻断Wnt/β-catenin通路,进而抑制成骨细胞[50]。此外,硬化蛋白基因抑制Wnt/β-catenin信号通路减少成肌细胞而分化,对于肌肉质量和功能也产生负面影响[38]。抑制硬化蛋白基因可以有效增加骨质疏松症患者的骨密度及瘦体质量,增强肌肉再生,促进肌肉功能恢复[51-52]。
2.4 肌骨的干细胞交互 近年随着研究的深入,发现肌肉与骨骼间的相互作用不仅涉及机械和分泌功能,肌肉中的干细胞能够间接影响邻近的骨膜和骨骼,甚至迁移至邻近的骨骼直接为骨骼再生提供干细胞来源。骨骼维持其结构和功能很大程度上依赖骨骼干细胞/祖细胞的激活[53]。骨骼干细胞/祖细胞能自我更新,并能分化成骨、软骨和基质[54]。已确认来源于骨髓、骨骺、骨膜等多种骨骼干细胞/祖细胞可用于骨修复,这些细胞群体具有不同的谱系潜能,不同程度参与骨修复过程[55]。
成纤维脂肪祖细胞是分化为骨骼肌的重要祖细胞,成纤维脂肪祖细胞是一种定植于肌组织中的间充质干细胞,具有在组织损伤后活化为成纤维细胞、脂肪细胞和成骨细胞等间充质谱系的能力。肌肉干/祖细胞(也称肌卫星细胞)是一种位于骨骼肌组织中的成体干细胞,主要负责肌肉的生长、修复和再生,肌肉干/祖细胞在骨骼肌再生过程中与成纤维脂肪祖细胞密切配合。一项实验探究了肌源性干细胞在骨折愈合中的作用,通过转基因小鼠的谱系追踪和干细胞移植实验发现肌肉干/祖细胞在骨折断端可以形成软骨细胞[19,56]。
然而,目前尚无证据显示骨骼中的干细胞对肌肉产生直接影响。骨骼干细胞/祖细胞的成肌能力尚未得到深入研究,但成骨不全症患者同时出现骨骼脆弱和肌肉无力可能说明这两种组织之间存在潜在联系[57]。
2.5 肌骨交互机制视域下现有的临床治疗方法
2.5.1 基于机械交互机制 人体骨量在30岁达到峰值,到70岁时骨量通常会进行性减少至30%。人体肌纤维质量在25岁时达到高峰,40岁之前相对稳定,之后肌肉纤维损失加速,直至80岁时肌肉质量损失30%[58]。一项对288名老年受试者的研究表明,患肌少症的老年人患骨质疏松症的风险高4倍[59]。一项横断面研究调查了芬兰2 142名55岁及以上老年人的骨肌肉减少症患病率及其相关性,肌少症、骨质疏松症和肌少-骨质疏松症的患病率分别为13.8%,11.1%和3.9%。骨肌肉减少症与低体质量指数、慢步态速度、行动不便、日常生活的活动能力下降及抑郁有关[60]。肌骨的退行性变与年龄衰老和机体运动功能密切相关,衰老是不可逆转的危险性因素,而对运动功能的干预是可行的措施。体力活动可以抑制肌肉生长抑制素分泌到循环中,而缺乏体力活动和卧床休息则与之完全相反[61]。
运动可以预防和治疗肌骨退行性疾病,不同形式的运动对肌肉和骨骼有不同影响,其中高强度间歇训练的运动方案对机体在细胞和组织层面更有益处[62-63]。过度的高强度运动对骨骼健康不利,反而会在体内引发高水平的氧化应激,对骨组织造成负面影响。而定期进行适度运动则能增强机体的抗氧化防御能力,可以抑制过度的氧化应激反应,促进骨代谢的正平衡,延缓与年龄相关的骨质流失和骨微结构退变,对多种因素引起的骨质疏松症具有预防和治疗作用。同时运动疗法必须遵从个体化的原则并保证患者能长期坚持,以避免造成急性创伤或慢性损害,比如有氧运动,包括慢跑、爬楼梯和踏步运动更适合患骨质疏松症的老年患者[64]。PMP 22蛋白是一种由有氧运动诱导的小鼠骨骼肌细胞因子,与股骨皮质厚度呈正相关,可以抑制卵巢切除小鼠骨密度的下降,体外实验发现其与成骨细胞的形成和破骨细胞的抑制有关[65]。对一组年龄高于70岁女性的横断面研究表明,下肢的适当抗阻训练会使欠羧化骨钙素增加,同时伴随下肢肌肉力量的提高,研究发现未羧化骨钙素和α-ACT蛋白之间呈负相关,α-ACT蛋白是一种与肌肉减少症的炎症机制相关的急性期反应蛋白[66]。
2.5.2 基于生物化学交互机制 在临床实践中,许多药物已被用于单独治疗肌肉减少症和骨质疏松症。用于治疗骨质疏松症的药物包括双膦酸盐、降钙素、甲状旁腺激素类似物和雌激素,大致可分为两类:抑制骨吸收和促进骨生成的药物,从而增加骨量和骨密度并降低骨折风险[67]。目前临床上只有一种药物被专用于治疗肌肉萎缩,重组人生长激素用于治疗人类免疫缺陷病毒相关的消瘦,它有效地维持因抗反转录病毒治疗而生长激素缺乏患者的瘦体质量和体质量。重组人生长激素也被证明改善了肌肉骨骼损伤和失用性萎缩患者的预后。同时还有其他药物可以在一定程度上延缓肌肉衰老、改善肌肉功能,例如活性维生素D、β肾上腺素能受体兴奋剂和血管紧张素转换酶抑制剂[68]。地舒单抗通过靶向结合核因子κB受体活化因子配体竞争性抑制破骨细胞的形成和活性,可以有效增加肌肉质量、强度和功能,在骨折愈合期间改善骨强度和硬度;唑来膦酸通过抑制法尼基酰转移酶等酶的活性降低破骨细胞的信号传导,这两种药在临床上治疗骨质疏松起着关键作用,并对肌肉退化也有正向作用。一项研究在老年髋部骨折患者中前瞻性地比较了地舒单抗与唑来膦酸对骨密度和骨骼肌力量的改善作用, 结果显示地舒单抗的作用优于双膦酸盐[69]。
维生素D通过Wnt/β-catenin信号通路刺激骨形成和骨矿化,上调骨骼肌中维生素D受体水平,增加维生素D受体活性,增加肌肉线粒体功能并限制线粒体自噬,从而改善肌肉功能,增强肌肉力量[70]。重组人生长因子治疗通过影响全身生长因子和胰岛素样生长因子1水平发挥作用,从而改善机体功能、肌肉质量和骨密度[71]。选择性雌激素受体调节剂作为雄激素受体配体,对性腺减退、肌肉萎缩、骨质疏松也有积极的影响[72]。
特立帕肽被称为甲状旁腺激素类似物,连续给予特立帕肽具有分解代谢作用,而间歇给予特立帕肽对骨具有合成代谢作用[73]。特立帕肽对绝经后骨质疏松女性和骨折高风险的骨质疏松患者有较好疗效。甲状旁腺激素1受体是一种在成骨细胞中发现的G蛋白偶联受体,具有甲状旁腺激素调节功能。当甲状旁腺激素1受体被激活时,它刺激多种G蛋白偶联受体相关信号传导,包括PLC/蛋白激酶C、cAMP/蛋白激酶A和细胞外调节蛋白激酶等信号通路,致骨生成增加,还通过抑制硬化蛋白影响Wnt/β-catenin信号传导途径[73]。甲状旁腺激素对肌卫星细胞的增殖和分化具有积极影响[74]。
2.6 肌骨交互机制视域下对相关疾病潜在的干预途径 运动锻炼结合药物治疗对于肌骨退行性疾病有良好效果。在骨折患者中,卧床时间的延长和体力活动的减少是不可避免的,这意味着在短期内难以实施有效的功能恢复和抗阻运动,因此,随着对肌肉与骨骼之间相互作用的深入理解,将两者作为一个整体,开发能够作用于肌骨共同靶点的技术或药物将具有广阔的应用前景。
2.6.1 基于机械交互机制 对骨骼施加的机械应力对于刺激骨代谢和骨修复至关重要。一项动物研究表明,低幅高频振动可以通过刺激肌纤维而影响骨生成,增强骨化性骨折愈合;而且低幅高频振动有助于抵消肌肉力量和活动性的丧失,显著改善IIa型肌纤维的收缩性和横截面积,增加卫星细胞活化和抑制肌生长抑制素表达,从而延缓肌肉减少症动物模型中肌肉减少症的进展[10]。一项对710名社区老年人的随机对照试验显示,低幅高频振动疗法可有效预防跌倒并改善肌肉力量和平衡能力,表明低幅高频振动疗法可用于缓解改善老年人肌肉功能和力量的退化[75]。
2.6.2 基于生物化学交互机制 COLAIANNI等[76]研究发现,缺乏鸢尾素会减缓骨骼生长并降低骨密度,相反,外源性鸢尾素治疗不仅通过促进骨生成和降低破骨细胞活性来增加骨质量和强度,还提升了骨骼肌的质量和强度。对骨质流失小鼠模型注射鸢尾素可促进骨量恢复[77]。在小鼠骨折模型中,鸢尾素处理组的骨痂形成和矿化更快,骨痂的大小和体积及骨折端新生血管的形成相较对照组更显著,体外实验结果表明鸢尾素能促进细胞内成骨和血管生成,提示鸢尾素可能是通过促进骨形成和血管生成来促进骨折愈合的[78]。基于这些发现可开发一种鸢尾素的疗法,用于治疗卧床或航天导致的失用性骨质疏松症,还可用于加快脆性骨折患者的骨折愈合及身体机能的恢复。鱿鱼软骨的Ⅱ型胶原可介导肌源性胰岛素样生长因子1和鸢尾素的产生和释放,从而促进小鼠的骨折愈合[79]。
肌生长抑制素/促活素A信号是肌肉生长的有效抑制剂和肌肉祖细胞分化的调节剂[68]。LEE等[80]研究发现,抑制肌生长抑制素/促活素A信号传导可明显降低小鼠在太空飞行期间骨骼肌和骨骼的损失。有研究表明,肌肉减少症状态下肌生成抑制素水平升高会阻碍骨折愈合,而肌肉生长抑制素抑制剂同时促进骨折愈合和骨骼肌再生[81]。现已有多种肌肉生长抑制素抑制剂进入研制阶段,被证明可增加肌细胞蛋白质合成、减少降解、增强线粒体生物合成,保护肌肉功能[80]。BIALEK等[82]研究表明,可溶性肌生长抑制素诱饵受体对小鼠的肌肉和骨骼质量都呈现了正向作用。
在一项失用后肢模型的小鼠研究中,用L-β-氨基异丁酸处理后可观察到骨细胞凋亡减少,细胞凋亡作用与抗活性氧的保护功能相关,以阻止骨丢失[83]。一项研究证明L-β-氨基异丁酸与低强度机械负荷对肌骨存在正向协同作用,将两者合用可能对难以进行高强度运动的患者具有重要意义[41]。
针对几种骨因子的干预措施也表现出治疗骨质疏松相关骨折的潜力。研究发现骨折后硬化蛋白基因的表达增加,骨折延迟愈合,骨和骨骼肌的质量和强度也发生降低,抑制硬化蛋白基因可以有效增加骨质疏松症患者的骨密度,改善糖尿病或老年小鼠的肌肉质量和功能[84]。另一项研究证明,抑制硬化蛋白基因可缓解乳腺癌骨转移小鼠的骨转移负荷和肌肉无力,同时延长小鼠生存时间[85]。抑制硬化蛋白基因或是治疗与Wnt/β-catenin信号通路介导的细胞内信号级联相关疾病有潜力的治疗靶点。罗莫佐单抗通过靶向抑制骨硬化蛋白促进骨形成并抑制骨吸收[67],现已作为抗骨质疏松药物在国外上市,但其对肌肉的影响还未有确切研究。
抑制核因子κB受体活化因子配体可以改善骨的质量、强度和功能。有研究表明,除骨组织外,核因子κB受体活化因子配体在骨骼肌中同样表达,激活其通路可致快肌Ⅱb肌纤维的选择性萎缩伴无力,此表型通过对核因子κB受体活化因子配体的抑制治疗得到缓解[86]。骨保护素免疫球蛋白片段复合物注射剂用于抗核因子κB受体活化因子配体治疗,已被证实能够增加肌卫星细胞密度和肌纤维横截面积、抑制细胞损害和凋亡,表明骨保护素免疫球蛋白片段复合物对挽救萎缩肌肉的功能和力量、促进损伤后的肌肉再生具有治疗潜力[87]。抗核因子κB受体活化因子配体的单克隆抗体通过影响核因子κB受体活化因子配体和上游核因子κB通路影响骨骼和肌肉的生长发育[88]。
2.6.3 基于干细胞交互机制 转化生长因子β信号通路转导可调节成纤维脂肪祖细胞的激活和分化,转化生长因子β超家族的配体包括转化生长因子β、肌肉生长抑制素和骨形态发生蛋白,可以诱导细胞增殖、肌成纤维细胞分化和细胞外基质沉积。成纤维脂肪祖细胞是促进肌内成骨的关键细胞,其中骨形态发生蛋白2和骨形态发生蛋白9均能推动成纤维脂肪祖细胞向成骨细胞分化[89]。此外,激活素受体在成纤维脂肪祖细胞中的靶向表达也可以激活其在肌肉中异位骨化,是进行性骨化纤维发育不良中异位骨化的成因[90]。这两项研究表明,骨形态发生蛋白和激活素信号传导在调节成纤维脂肪祖细胞成骨分化中的关键作用。
结合成纤维脂肪祖细胞和肌卫星细胞的成骨作用,利用诱导其定向成骨分化因子的能力,在骨折愈合再生中具有广阔前景,为肌肉骨骼疾病的再生医学提供了新的方向。现阶段富血小板血浆、骨髓和脂肪组织是常用的骨科生物制品。富血小板血浆获取操作简便,对组织再生有一定的帮助,但干细胞成分浓度较低。间充质干细胞是再生医学领域最有潜力的干细胞,富含间充质干细胞的脂肪组织和脐带是其有希望的来源[91]。一些研究提出了涉及成纤维脂肪祖细胞在肌肉骨骼疾病治疗中的潜在疗法。肌肉纤维化是创伤、衰老或营养不良的反应,长期损害肌肉功能,还可延缓损伤愈合。成纤维脂肪祖细胞能通过内皮素旁分泌信号通路与肌肉细胞交互,在骨骼肌纤维化中具有关键作用,使用内皮素受体拮抗剂波生坦能够抑制纤维化并促进骨骼肌的再生,该研究将内皮素确定为拮抗人体肌肉纤维化的新成药靶点[21]。在骨肌多发伤情况下,酪氨酸激酶抑制剂伊马替尼可通过减少主要由成纤维脂肪祖细胞引起的持续性愈合组织纤维化来改善骨再生[92]。
干细胞的分泌因子也有可能成为促进骨骼和肌肉再生的潜在治疗药物。成肌细胞分泌的细胞外囊泡中的miRNA-196a-5p可抑制小鼠细胞中破骨细胞样细胞的形成、抑制破骨细胞相关基因的mRNA以及核因子κB受体活化因子配体诱导的线粒体能量代谢而保护骨量[93]。在青少年特发性脊柱侧凸患者凹侧的肌卫星细胞中,发现其分化必需的雌激素受体1表达下降及其信号传导被破坏,导致肌卫星细胞分化缺陷,而雷洛昔芬在凹侧激活脊髓旁肌雌激素受体1信号可以一定程度上逆转脊柱的病理性侧弯[12]。一项研究强调了骨折愈合过程急性炎症期对正常骨愈合的重要性,对移植的间充质干细胞进行促炎细胞因子共培养或缺氧条件预处理可增强其成骨潜力,对局部炎症进行免疫调节以促进肌肉骨骼组织的愈合和再生,而不同组织来源间充质干细胞的成骨能力还尚在研究中[94]。
肌源性和骨源性干细胞通过自身分化或是激活相关细胞信号转导通路和局部因子的调控,对骨骼肌肉系统的发育、稳态、再生作用是未来可深入探究的领域。

| [1] LOMBARDI G, ZIEMANN E, BANFI G. Physical activity and bone health: what is the role of immune system? A narrative review of the third way. Front Endocrinol. 2019;10:60. [2] GOMARASCA M, BANFI G, LOMBARDI G. Myokines: The endocrine coupling of skeletal muscle and bone. Adv Clin Chem. 2020;94:155-218. [3] KIRK B, FEEHAN J, LOMBARDI G, et al. Muscle, bone, and fat crosstalk: the biological role of myokines, osteokines, and adipokines. Curr Osteoporos Rep. 2020;18(4):388-400. [4] STEPPE L, MEGAFU M, TSCHAFFON-MÜLLER MEA, et al. Fracture healing research: Recent insights. Bone Rep. 2023;19:101686. [5] DING P, GAO C, GAO Y, et al. Osteocytes regulate senescence of bone and bone marrow. Elife. 2022;11:e81480. [6] KUBAT GB, BOUHAMIDA E, ULGER O, et al. Mitochondrial dysfunction and skeletal muscle atrophy: Causes, mechanisms, and treatment strategies. Mitochondrion. 2023;72:33-58. [7] WANG Z. Aging and Aging-Related Diseases: Mechanisms and Interventions. Adv Exp Med Biol. 2018. doi:10.1007/978-981-13-1117-8. [8] XIE WQ, HE M, YU DJ, et al. Correlation study between bone metabolic markers, bone mineral density, and sarcopenia. J Endocrinol Invest. 2024;47(6):1559-1572. [9] GIELEN E, DUPONT J, DEJAEGER M, et al. Sarcopenia, osteoporosis and frailty. Metabolism. 2023;145:155638. [10] ZHANG N, CHIM YN, WANG J, et al. Impaired fracture healing in sarco‐osteoporotic mice can be rescued by vibration treatment through myostatin suppression. J Orthop Res. 2020;38(2):277-287. [11] ZHOU J, YI J, BONEWALD L. Muscle-bone crosstalk in amyotrophic lateral sclerosis. Curr Osteoporos Rep. 2015;13:274-279. [12] SHAO X, FU X, YANG J, et al. The asymmetrical ESR1 signaling in muscle progenitor cells determines the progression of adolescent idiopathic scoliosis. Cell Discov. 2023;9(1):44. [13] WOLFF J. The Classic: on the Inner Architecture of Bones and its Importance for Bone Growth:(Ueber die innere Architectur der Knochen und ihre Bedeutung für die Frage vom Knochenwachsthum). Clin Orthop Relat Res. 2010;468(4):1056-1065. [14] MOHR T, ANDERSEN JL, BIERING-SØRENSEN F, et al. Long term adaptation to electrically induced cycle training in severe spinal cord injured individuals. Spinal Cord. 1997;35(1):1-16. [15] FROST HM. The Utah paradigm of skeletal physiology: an overview of its insights for bone, cartilage and collagenous tissue organs. J Bone Miner Metab. 2000;18:305-316. [16] PEDERSEN BK, ÅKERSTRÖM TC, NIELSEN AR, et al. Role of myokines in exercise and metabolism. J Appl Physiol (1985). 2007;103(3):1093-1098. [17] BRAY N. Targeting myostatin for direct joint defence. Nat Rev Drug Discov. 2015;14(10):677-677. [18] TAGLIAFERRI C, WITTRANT Y, DAVICCO MJ, et al. Muscle and bone, two interconnected tissues. Ageing Res Rev. 2015;21:55-70. [19] ABOU-KHALIL R, YANG F, LIEU S, et al. Role of muscle stem cells during skeletal regeneration. Stem Cells. 2015;33(5):1501-1511. [20] KIM H, WRANN CD, JEDRYCHOWSKI M, et al. Irisin mediates effects on bone and fat via αV integrin receptors. Cell. 2018;175(7):1756-1768.e17. [21] JULIEN A, KANAGALINGAM A, MARTÍNEZ-SARRÀ E, et al. Direct contribution of skeletal muscle mesenchymal progenitors to bone repair. Nat Commun. 2021; 12(1):2860. [22] MAO Y, YAN, YANG J, et al. Muscle-bone cross-talk through the FNIP1-TFEB-IGF2 axis is associated with bone metabolism in human and mouse. Sci Transl Med. 2024;16(750):eadk9811. [23] FRONTERA WR, OCHALA J. Skeletal muscle: a brief review of structure and function. Calcif Tissue Int. 2015;96:183-195. [24] JAYASINGHE SAL, SCHEIDT RA, SAINBURG RL. Neural control of stopping and stabilizing the arm. Front Integr Neurosci. 2022;16:835852.
[25] SYLVESTER AD, LAUTZENHEISER SG, KRAMER PA. A review of musculoskeletal modelling of human locomotion. Interface Focus. 2021;11(5):20200060. [26] INTEMANN J, DE GORTER DJJ, NAYLOR AJ, et al. Importance of osteocyte-mediated regulation of bone remodelling in inflammatory bone disease. Swiss Med Wkly. 2020;150(0506):w20187-w20187. [27] GOODMAN CA, HORNBERGER TA, ROBLING AG. Bone and skeletal muscle: key players in mechanotransduction and potential overlapping mechanisms. Bone. 2015;80:24-36. [28] MURPHY P, ROLFE RA. Building a Co-ordinated Musculoskeletal System: The Plasticity of the Developing Skeleton in Response to Muscle Contractions//Roles of Skeletal Muscle in Organ Development: Prenatal Interdependence among Cells, Tissues, and Organs. Cham: Springer International Publishing, 2023:81-110. [29] LEEK CC, SOULAS JM, BHATTACHARYA I, et al. Deletion of Fibroblast growth factor 9 globally and in skeletal muscle results in enlarged tuberosities at sites of deltoid tendon attachments. Dev Dyn. 2021; 250(12):1778-1795. [30] WANG L, YOU X, LOTINUN S, et al. Mechanical sensing protein PIEZO1 regulates bone homeostasis via osteoblast-osteoclast crosstalk. Nat Commun. 2020;11(1):282. [31] JACKOWSKI SA, LANOVAZ JL, VAN OORT C, et al. Does lean tissue mass accrual during adolescence influence bone structural strength at the proximal femur in young adulthood? Osteoporos Int. 2014;25:1297-1304. [32] LAU P, VICO L, RITTWEGER J. Dissociation of bone resorption and formation in spaceflight and simulated microgravity: Potential role of myokines and osteokines? Biomedicines. 2022;10(2):342. [33] MAAK S, NORHEIM F, DREVON CA, et al. Progress and challenges in the biology of FNDC5 and irisin. Endocr Rev. 2021;42(4):436-456. [34] LIU S, CUI F, NING K, et al. Role of irisin in physiology and pathology. Front Endocrinol. 2022;13:962968. [35] ROOMI AB, NORI W, HAMED RM. Lower serum irisin levels are associated with increased osteoporosis and oxidative stress in postmenopausal. Rep Biochem Mol Biol. 2021;10(1):13. [36] ALSAAWI TA, ALDISI D, ABULMEATY MMA, et al. Screening for sarcopenia among elderly arab females: influence of body composition, lifestyle, irisin, and vitamin D. Nutrients. 2022;14(9): 1855. [37] QIN Y, PENG Y, ZHAO W, et al. Myostatin inhibits osteoblastic differentiation by suppressing osteocyte-derived exosomal microRNA-218: A novel mechanism in muscle-bone communication. J Biol Chem. 2017;292(26):11021-11033. [38] HE C, HE W, HOU J, et al. Bone and muscle crosstalk in aging. Front Cell Dev Biol. 2020;8:585644. [39] KURIYAMA N, OZAKI E, KOYAMA T, et al. Evaluation of myostatin as a possible regulator and marker of skeletal muscle-cortical bone interaction in adults. J Bone Miner Metab. 2021;39:404-415. [40] BONEWALD L. Use it or lose it to age: A review of bone and muscle communication. Bone. 2019;120:212-218. [41] PRIDEAUX M, SMARGIASSI A, PENG G, et al. L BAIBA Synergizes with Sub Optimal Mechanical Loading to Promote New Bone Formation. JBMR Plus. 2023;7(6):e10746. [42] NOVAIS A, CHATZOPOULOU E, CHAUSSAIN C, et al. The potential of FGF-2 in craniofacial bone tissue engineering: a review. Cells. 2021;10(4):932. [43] MAZZIOTTI G, LANIA AG, CANALIS E. Skeletal disorders associated with the growth hormone–insulin-like growth factor 1 axis. Nat Rev Endocrinol. 2022;18(6):353-365. [44] ADHIKARY S, CHOUDHARY D, TRIPATHI AK, et al. FGF-2 targets sclerostin in bone and myostatin in skeletal muscle to mitigate the deleterious effects of glucocorticoid on musculoskeletal degradation. Life Sci. 2019;229:261-276. [45] CHOWDHURY S, SCHULZ L, PALMISANO B, et al. Muscle-derived interleukin 6 increases exercise capacity by signaling in osteoblasts. J Clin Invest. 2020;130(6): 2888-2902. [46] MARCADET L, BOUREDJI Z, ARGAW A, et al. The roles of RANK/RANKL/OPG in cardiac, skeletal, and smooth muscles in health and disease. Front Cell Dev Biol. 2022;10:903657. [47] DUFRESNE SS, DUMONT NA, BOULANGER-PIETTE A, et al. Muscle RANK is a key regulator of Ca2+ storage, SERCA activity, and function of fast-twitch skeletal muscles. Am J Physiol Cell Physiol. 2016;310(8): C663-C672. [48] WANG H, LI J, XU Z, et al. Undercarboxylated osteocalcin inhibits the early differentiation of osteoclast mediated by Gprc6a. PeerJ. 2021;9: e10898. [49] PARK D, KIM DY, BYUN MR, et al. Undercarboxylated, But Not Carboxylated, Osteocalcin Suppresses TNF-α-Induced Inflammatory Signaling Pathway in Myoblasts. J Endocr Soc. 2022;6(8):bvac084. [50] MORETTI A, IOLASCON G. Sclerostin: clinical insights in muscle–bone crosstalk. J Int Med Res. 2023;51(8):03000605231193293. [51] RECKER RR, BENSON CT, MATSUMOTO T, et al. A randomized, double‐blind phase 2 clinical trial of blosozumab, a sclerostin antibody, in postmenopausal women with low bone mineral density. J Bone Miner Res. 2015;30(2):216-224. [52] KIM SP, FREY JL, LI Z, et al. Sclerostin influences body composition by regulating catabolic and anabolic metabolism in adipocytes. Proc Natl Acad Sci U S A. 2017;114(52):E11238-E11247. [53] JEFFERY EC, MANN TLA, POOL JA, et al. Bone marrow and periosteal skeletal stem/progenitor cells make distinct contributions to bone maintenance and repair. Cell Stem Cell. 2022;29(11):1547-1561.e6. [54] CHAN CKF, GULATI GS, SINHA R, et al. Identification of the human skeletal stem cell. Cell. 2018;175(1):43-56.e21. [55] SEROWOKY MA, ARATA CE, CRUMP JG, et al. Skeletal stem cells: insights into maintaining and regenerating the skeleton. Development. 2020;147(5): dev179325. [56] GIULIANI G, ROSINA M, REGGIO A. Signaling pathways regulating the fate of fibro/adipogenic progenitors (FAPs) in skeletal muscle regeneration and disease. FEBS J. 2022;289(21):6484-6517. [57] PHILLIPS CL, JEONG Y. Osteogenesis imperfecta: Muscle-bone interactions when bi-directionally compromised. Curr Osteoporos Rep. 2018;16:478-489. [58] 董单,许超,万晴冬,等.肌少-骨质疏松症的研究进展[J].中华内分泌代谢杂志,2023,39(7):625-631. [59] LOCQUET M, BEAUDART C, BRUYÈRE O, et al. Bone health assessment in older people with or without muscle health impairment. Osteoporos Int. 2018;29:1057-1067. [60] BLOMQVIST M, NUOTIO M, SÄÄKSJÄRVI K, et al. Osteosarcopenia in Finland: prevalence and associated factors. Arch Osteoporos. 2024;19(1):1-11. [61] SMEUNINX B, ELHASSAN YS, MANOLOPOULOS KN, et al. The effect of short‐term exercise prehabilitation on skeletal muscle protein synthesis and atrophy during bed rest in older men. J Cachexia Sarcopenia Muscle. 2021;12(1):52-69. [62] CHEN J, ZHOU R, FENG Y, et al. Molecular mechanisms of exercise contributing to tissue regeneration. Signal Transduct Target Ther. 2022;7(1):383. [63] SURESH KUMAR H, BARNETT EN, FOWLKES JL, et al. Biomechanical Stimulation of Muscle Constructs Influences Phenotype of Bone Constructs by Modulating Myokine Secretion. JBMR Plus. 2023;7(11):e10804. [64] GAO H, ZHAO Y, ZHAO L, et al. The Role of Oxidative Stress in Multiple Exercise-Regulated Bone Homeostasis. Aging Dis. 2023;14(5):1555. [65] KAWAGUCHI M, KAWAO N, MURATANI M, et al. Role of peripheral myelin protein 22 in chronic exercise‐induced interactions of muscle and bone in mice. J Cell Physiol. 2022;237(5):2492-2502. [66] LEVINGER I, SCOTT D, NICHOLSON GC, et al. Undercarboxylated osteocalcin, muscle strength and indices of bone health in older women. Bone. 2014;64:8-12. [67] PANA A, SOURTZI P, KALOKAIRINOU A, et al. Sarcopenia and polypharmacy among older adults: a scoping review of the literature. Arch Gerontol Geriatr. 2022;98:104520. [68] RODGERS BD, WARD CW. Myostatin/activin receptor ligands in muscle and the development status of attenuating drugs. Endocr Rev. 2022;43(2):329-365. [69] RUPP T, VON VOPELIUS E, STRAHL A, et al. Beneficial effects of denosumab on muscle performance in patients with low BMD: a retrospective, propensity score-matched study. Osteoporos Int. 2022;33(10):2177-2184. [70] BASS JJ, KAZI AA, DEANE CS, et al. The mechanisms of skeletal muscle atrophy in response to transient knockdown of the vitamin D receptor in vivo. J Physiol. 2021;599(3):963-979. [71] ALTOWATI MA, SHEPHERD S, MCGROGAN P, et al. Effects of recombinant human growth hormone in children with Crohn’s disease on the muscle-bone unit: a preliminary study. Horm Res Paediatr. 2018;90(2):128-131. [72] ELAHMER NR, WONG SK, MOHAMED N, et al. Mechanistic Insights and Therapeutic Strategies in Osteoporosis: A Comprehensive Review. Biomedicines. 2024;12(8):1635. [73] BRENT MB, STOLTENBORG FE, BRÜEL A, et al. Teriparatide and abaloparatide have a similar effect on bone in mice. Front Endocrinol. 2021;12:628994. [74] ROMAGNOLI C, ZONEFRATI R, LUCATTELLI E, et al. In Vitro Effects of PTH (1-84) on Human Skeletal Muscle-Derived Satellite Cells. Biomedicines. 2023;11(4):1017. [75] LEUNG KS, LI CY, TSE YK, et al. Effects of 18-month low-magnitude high-frequency vibration on fall rate and fracture risks in 710 community elderly-a cluster-randomized controlled trial. Osteoporos Int. 2014;25:1785-1795. [76] COLAIANNI G, CUSCITO C, MONGELLI T, et al. The myokine irisin increases cortical bone mass. Proc Natl Acad Sci U S A. 2015;112(39):12157-12162. [77] COLAIANNI G, MONGELLI T, CUSCITO C, et al. Irisin prevents and restores bone loss and muscle atrophy in hind-limb suspended mice. Sci Rep. 2017;7(1):2811. [78] KAN T, HE Z, DU J, et al. Irisin promotes fracture healing by improving osteogenesis and angiogenesis. J Orthop Translat. 2022;37:37-45. [79] LI Z, TIAN Y, ZHANG L, et al. Type II collagen from squid cartilage mediated myogenic IGF-I and irisin to activate the Ihh/PThrp and Wnt/β-catenin pathways to promote fracture healing in mice. Food Funct. 2021;12(14):6502-6512. [80] LEE SJ, LEHAR A, MEIR JU, et al. Targeting myostatin/activin A protects against skeletal muscle and bone loss during spaceflight. Proc Natl Acad Sci U S A. 2020; 117(38):23942-23951. [81] ZHANG N, CHIM YN, WANG J, et al. Impaired fracture healing in sarco-osteoporotic mice can be rescued by vibration treatment through myostatin suppression. J Orthop Res. 2020;38(2):277-287. [82] BIALEK P, PARKINGTON J, LI X, et al. A myostatin and activin decoy receptor enhances bone formation in mice. Bone. 2014;60:162-171. [83] KITASE Y, VALLEJO JA, GUTHEIL W, et al. β-aminoisobutyric acid, l-BAIBA, is a muscle-derived osteocyte survival factor. Cell Rep. 2018;22(6): 1531-1544. [84] RAMLI FF, CHIN KY. A review of the potential application of osteocyte-related biomarkers, fibroblast growth factor-23, sclerostin, and dickkopf-1 in predicting osteoporosis and fractures. Diagnostics. 2020;10(3):145. [85] MAUREL DB, MATSUMOTO T, VALLEJO JA, et al. Characterization of a novel murine Sost ERT2 Cre model targeting osteocytes. Bone Res. 2019;7(1):6. [86] HAMOUDI D, BOUREDJI Z, MARCADET L, et al. Muscle weakness and selective muscle atrophy in osteoprotegerin-deficient mice. Hum Mol Genet. 2020;29(3): 483-494. [87] BOUREDJI Z, HAMOUDI D, MARCADET L, et al. Testing the efficacy of a human full-length OPG-Fc analog in a severe model of cardiotoxin-induced skeletal muscle injury and repair. Mol Ther Methods Clin Dev. 2021;21:559-573. [88] ONO T, HAYASHI M, SASAKI F, et al. RANKL biology: bone metabolism, the immune system, and beyond. Inflamm Regen. 2020;40:1-16. [89] JUBAN G, SACLIER M, YACOUB-YOUSSEF H, et al. AMPK activation regulates LTBP4-dependent TGF-β1 secretion by pro-inflammatory macrophages and controls fibrosis in Duchenne muscular dystrophy. Cell Rep. 2018;25(8):2163-2176.e6. [90] LEES-SHEPARD JB, YAMAMOTO M, BISWAS AA, et al. Activin-dependent signaling in fibro/adipogenic progenitors causes fibrodysplasia ossificans progressiva. Nat Commun. 2018;9(1):471. [91] FANG WH, VANGSNESS JR CT. Food and Drug Administration’s Position on Commonly Injected Biologic Materials in Orthopaedic Surgery. Am J Sports Med. 2021;49(12):3414-3421. [92] BENSALAH M, MURAINE L, BOULINGUIEZ A, et al. A negative feedback loop between fibroadipogenic progenitors and muscle fibres involving endothelin promotes human muscle fibrosis. J Cachexia Sarcopenia Muscle. 2022;13(3):1771-1784. [93] TAKAFUJI Y, TATSUMI K, KAWAO N, et al. MicroRNA-196a-5p in extracellular vesicles secreted from myoblasts suppresses osteoclast-like cell formation in mouse cells. Calcif Tissue Int. 2021;108:364-376. [94] MARUYAMA M, RHEE C, UTSUNOMIYA T, et al. Modulation of the inflammatory response and bone healing. Front Endocrinol (Lausanne). 2020;11:386. |
| [1] | 陈伊娴, 陈 晨, 卢立恒, 汤锦鹏, 于晓巍. 雷公藤甲素治疗骨关节炎的网络药理学分析与实验验证[J]. 中国组织工程研究, 2026, 30(4): 805-815. |
| [2] | 鄢成波, 罗秋池, 樊佳兵, 顾叶婷, 邓 倩, 张军梅. 2型糖尿病对大鼠正畸牙移动与张力侧骨微结构参数的影响[J]. 中国组织工程研究, 2026, 30(4): 824-831. |
| [3] | 李广政, 李 威, 张博淳, 丁浩秦, 周忠起, 李 刚, 梁学振. 绝经后女性肌肉减少症预测模型:中国健康与养老全国追踪调查数据库信息分析[J]. 中国组织工程研究, 2026, 30(4): 849-857. |
| [4] | 邹荣基, 喻芳芳, 王茂林, 贾卓鹏 . 雷公藤内酯酮抑制铁死亡改善大脑动脉闭塞/再灌注模型大鼠脑缺血再灌注损伤[J]. 中国组织工程研究, 2026, 30(4): 873-881. |
| [5] | 陈小青, 卞路瑶, 陆星宇, 杨 涛, 李湘海. 心俞穴位埋线预处理改善急性心肌缺血模型大鼠的心功能[J]. 中国组织工程研究, 2026, 30(4): 882-891. |
| [6] | 王明琦, 冯诗雅, 韩银河, 于朋鑫, 郭丽娜, 贾子萱, 王秀丽. 神经化肠黏膜组织工程模型的构建及体外评价[J]. 中国组织工程研究, 2026, 30(4): 892-900. |
| [7] | 王 杰, 黄 芮, 张 也, 首朝曦, 姚 杰, 刘辰希, 廖 健. 益生菌在种植体周炎中的作用及机制[J]. 中国组织工程研究, 2026, 30(4): 901-907. |
| [8] | 曹文琪, 冯秀芝, 赵 奕, 王智民, 陈怡然, 杨 潇, 任艳玲. 巨噬细胞极化对2型糖尿病性骨质疏松症成骨-成血管偶联的影响[J]. 中国组织工程研究, 2026, 30(4): 917-925. |
| [9] | 杨 肖, 白月辉, 赵甜甜, 王东昊, 赵 琛, 袁 硕. 颞下颌关节骨关节炎软骨退变:机制及再生的挑战[J]. 中国组织工程研究, 2026, 30(4): 926-935. |
| [10] | 余诗宇, 俞苏桐, 徐 杨, 镇祥燕, 韩凤选. 组织工程治疗策略在口腔黏膜下纤维化中的研究与应用进展[J]. 中国组织工程研究, 2026, 30(4): 936-948. |
| [11] | 金智勇, 汪宇峰, 赵滨杰, 熊敏全, 严 力. 基于双侧肢体控制策略视角分析肢体间不对称对运动能力的影响[J]. 中国组织工程研究, 2026, 30(4): 949-963. |
| [12] | 孙嘉禾, 史冀鹏, 朱天瑞, 权赫龙, 徐红旗. 运动对肌少症及其合并症老年人影响的Meta分析[J]. 中国组织工程研究, 2026, 30(4): 997-1007. |
| [13] | 曾 浩, 孙鹏程, 柴 源, 黄有荣, 张 驰, 章晓云. 甲状腺功能和骨质疏松症的关联:欧洲人群全基因组数据分析[J]. 中国组织工程研究, 2026, 30(4): 1019-1027. |
| [14] | 容向宾, 郑海波, 莫学燊, 侯 坤, 曾 平, . 血浆代谢物、免疫细胞与髋骨关节炎的因果推断:GWAS数据欧洲群体资料分析[J]. 中国组织工程研究, 2026, 30(4): 1028-1035. |
| [15] | 何启旺, 陈 波, 梁复超, 康泽伟, 周 原, 季桉旭, 唐夏林, . 阿尔茨海默病和肌少症及体质量指数的关系:欧洲人群GWAS数据集分析[J]. 中国组织工程研究, 2026, 30(4): 1036-1046. |
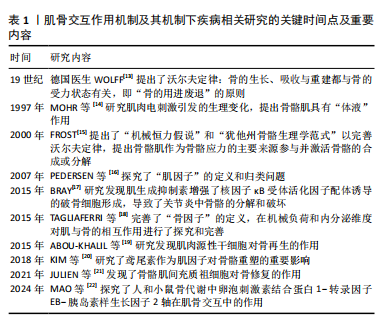
除受到全身因素影响外,肌肉与骨骼之间也存在重要的相互调控作用。近年来有大量研究专注于探究肌肉与骨骼两者之间的交互作用。从生物力学来看,人们首先认识到骨骼肌与骨骼的解剖学结构和机械应力传导有紧密联系,两者构建了机械结构和力学作用的统一整体。随着分子生物学的研究深入,发现肌肉和骨骼都具备内分泌作用,可以分别分泌肌因子和骨因子[2],可通过自分泌、旁分泌或内分泌的途径作用于彼此或机体其他系统[3]。最新的干细胞研究表明,肌肉和骨骼中的干细胞可以通过干细胞演化和细胞因子的表达直接或间接实现自身和对方的调控[4]。
骨转换依靠骨形成和骨吸收调控,其中骨形成由间充质干细胞衍生的成骨细胞介导,成骨细胞具有产生和组织形成骨细胞外基质的能力,负责合成和沉积新骨组织;骨吸收由单核细胞源性破骨细胞促进,它们分解矿化基质,将钙和磷酸盐释放到血液中,这个过程对钙稳态至关重要,而肌稳态受肌蛋白合成和降解之间的净平衡调控[2,5]。当肌形成与骨转换处于负平衡状态时,机体即发生肌萎缩和骨丢失,肌萎缩对应肌肉质量和肌力的降低、肌纤维数量及横截面积下降、肌蛋白含量降低、肌细胞线粒体功能障碍[6];骨丢失则表现为骨组织质量、微观结构、成分组成以及皮质骨和松质骨之间比例的降低[7]。肌肉和骨骼健康的变化密切相关,肌肉萎缩和骨质流失通常相伴发生[8]。临床上有诸多疾病与肌骨交互机制相关,主要有肌骨系统退行性疾病,如骨质疏松症、肌肉减少症,近年新提出的肌少-骨质疏松症是前两者共存的综合征[9],肌萎缩导致跌倒风险增加,伴随骨丢失所致骨骼强度下降,易导致脆性骨折、骨折延迟愈合等预后不良后果[10]。患有神经肌肉疾病或长期卧床休息的患者,以及执行太空飞行任务的宇航员,在运动系统失用且失负荷的因素下即会诱发肌萎缩和骨丢失。一些肌肉和骨骼的发育不良、发育畸形等疾病也与肌骨交互机制存在关系,如肌萎缩侧索硬化症和青少年特发性脊柱侧凸等疾病[11-12]。目前对肌骨退行性疾病和肌骨损伤的治疗主要集中于单独对肌肉或骨骼代谢的干预,不足以促进肌少-骨质疏松症等疾病肌骨退变的逆转、损伤后肌肉和骨折愈合及功能恢复。对肌骨交互机制的研究,为阐明此类疾病的病因提供了新方向,对开发共同针对肌和骨的临床疗法和药物具有重要意义。该文通过从生物力学、分子生物学、细胞生物学3个方面探讨肌骨交互的机制,以及基于此机制的肌肉骨骼疾病和肌骨损伤愈合的预防、治疗和干预,对国内外最新的研究成果进行阐述。
中国组织工程研究杂志出版内容重点:组织构建;骨细胞;软骨细胞;细胞培养;成纤维细胞;血管内皮细胞;骨质疏松;组织工程
1.1 资料来源
1.1.1 检索人及检索时间 由第一作者于2024年9月进行文献检索。
1.1.2 文献检索时限 检索时限为2014-2024年。
1.1.3 检索数据库 CNKI、万方和PubMed 数据库。
1.1.4 检索词 中文检索词为“肌骨交互,肌肉骨骼系统,组织通讯,肌因子,骨因子,肌少-骨质疏松症,肌少症,骨质疏松症,骨再生,成纤维脂肪祖细胞”,英文检索词为“muscle-bone crosstalk,musculoskeletal system,inter-tissue communication,Myokines,Osteokines,
Osteosarcopenia,Sarcopenia,Osteoporosis,Bone
Regeneration,fibro-adipogenic progenitors”。
1.1.5 检索文献类型 综述报告、研究原著等。
1.1.6 检索策略 中英文数据库检索策略,见图1。
1.2 入组标准
1.2.1 纳入标准 论述肌骨交互机制及此机制下肌骨退行性疾病和肌骨损伤的相关文献。
1.2.2 排除标准 ①研究方法缺乏科学性、数据可靠性差或样本量过小的研究;②证据等级不高及质量较低的文献;③年代久远,观点较陈旧的文献;④非重点研究肌骨交互作用且未详细描述两者机制的文章;⑤非重点研究肌骨退变和肌骨损伤的文章;⑥中文与外文研究重复的文章。
1.3 质量评估 由2名独立研究人员按照设定的纳入和排除标准分别对检索出来的文献设立数据库,阅读题目、摘要和全文对文献进行筛选,如果筛选过程中遇见分歧,2人进行讨论,并参考第三者意见获得最终决定。根据纳入及排除标准,对94篇符合标准的文献进行综述。文献筛选流程图见图2。
随着公共医疗水平的进步,全球人口平均寿命逐年上升,肌肉骨骼系统退行性疾病对老年人群的健康危害已是世界性的重大公共卫生问题和社会经济负担。肌肉和骨骼系统交互紧密,共赢共损,互为因果,其机制引发目前医学界的广泛研究。该文分别从肌骨的机械性交互、分泌因子交互、干细胞交互3方面进行归纳和总结,系统阐述了在该机制下肌骨退行性疾病和肌骨损伤从发生机制到治疗的研究现状,但更深度的机制与干预手段还未有明确阐明,未来的研究必将针对肌肉与骨骼共同作用靶点开发药物和针对性的临床疗法,实现肌骨系统的共病共治。
3.1 既往他人在该领域研究的贡献和存在的问题 以肌骨交互机制解释肌少-骨质疏松症为首要的肌骨退行性病变及(脆性)骨折的愈合再生相关研究已有较多报道,深入探讨分析了这些病症的发病机制,以及不同干预方式的有效性并进行了效果对比,为预防与治疗老年人肌骨退行性疾病及对骨折愈合治疗提供了实际案例及实质性见解。此前已有多篇文章在肌骨交互视角下对骨质疏松症、肌少症、肌少-骨质疏松症进行了关于机械性交互和分泌因子交互层面的探讨,但对肌骨交互视域下骨折的愈合重建、肌肉损伤的生长修复鲜有提及,在干细胞视角上对肌骨交互层面的探讨上也少有涉及,基于该机制对疾病的治疗方面鲜有全面论述。
3.2 该综述区别于他人他篇的特点 该文从近年相关研究入手,对肌骨交互的基本机制进行阐述,对机械性交互机制提供了新的运动干预手段与思路,如抗阻运动、有氧运动和低幅高频振动等,针对分泌因子交互的细胞因子、信号通路及其靶点做出具体阐述,对其因子干预的现状做出总结,对前景进行展望,并将干细胞交互做出自身分化和分泌因子两方面的归纳分析,总结出较为完整的干预方法与潜在前景。
3.3 该综述的局限性 当前关于肌骨交互的机制、参与的信号通路等研究还在相对早期阶段,相关疾病的机制研究、预防及治疗的方法尚不清晰,肌骨共病共治的治疗手段和药物研究仍旧欠缺。干细胞交互中的研究较少,基本集中于肌源性干细胞对骨作用,骨源性干细胞对肌肉作用尚未被证明。因此,该文仅探讨了现研究中的机制和治疗方法,并依靠已有机制推断可能的潜在干预手段及方案。
3.4 该综述的重要意义 文章通过综述大量肌骨交互机制及其相关疾病的研究,得出以下结论:①肌肉与骨骼的机械性交互、分泌因子交互和干细胞交互机制对肌骨系统的代谢及再生调控意义重大;②针对肌因子(肌生成抑制素、鸢尾素等)和骨因子(核因子κB受体活化因子配体、硬化蛋白等)生化信号的系统干预可以改善骨骼肌和骨的质量与功能,对骨折愈合同样有积极效果;③近年来发现肌骨系统中相关干细胞可进行交互作用,尤以成纤维脂肪祖细胞和肌卫星细胞等肌源性间充质干细胞的活化对骨的生长、修复和再生影响显著;④针对肌骨交互机制的研究可以对相关疾病的病因、预防、治疗提供思路,然而临床还未有对肌骨共病行之有效的治疗方法,大部分研究停留在细胞及动物实验阶段,因此未来还需要进行大量研究,逐步由实验向临床迈进,开发更具针对性的疗法及药物,更好地为临床服务。
中国组织工程研究杂志出版内容重点:组织构建;骨细胞;软骨细胞;细胞培养;成纤维细胞;血管内皮细胞;骨质疏松;组织工程
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||