[1] GUAN M, CHEN Y, WEI Y, et al. Long-lasting bactericidal activity through selective physical puncture and controlled ions release of polydopamine and silver nanoparticles-loaded TiO2 nanorods in vitro and in vivo. Int J Nanomedicine. 2019;14:2903-2914.
[2] GULATI K, CHOPRA D, KOCAK-OZTUG NA, et al. Fit and forget: The future of dental implant therapy via nanotechnology. Adv Drug Deliv Rev. 2023;199:114900.
[3] WANG Y, TAN P, WU Y, et al. Artificial intelligence-enhanced skin-like sensors based on flexible nanogenerators. View. 2022;3(5):20220026.
[4] KAMP NJ, AL-KHATIB SM. The subcutaneous implantable cardioverter-defibrillator in review. Am Heart J. 2019;217:131-139.
[5] ZHOU L, LYU J, LIU F, et al. Immunogenic PANoptosis-Initiated Cancer Sono-Immune Reediting Nanotherapy by Iteratively Boosting Cancer Immunity Cycle. Adv Mater. 2024;36(2):2305361.
[6] WHITAKER R, HERNAEZ-ESTRADA B, HERNANDEZ RM, et al. Immunomodulatory Biomaterials for Tissue Repair. Chem Rev. 2021; 121(18):11305-11335.
[7] PARKER JB, GRIFFIN MF, SPIELMAN AF, et al. Exploring the Overlooked Roles and Mechanisms of Fibroblasts in the Foreign Body Response. Adv Wound Care (New Rochelle). 2023;12(2):85-96.
[8] ZHANG B, SU Y, ZHOU J, et al. Toward a Better Regeneration through Implant‐Mediated Immunomodulation: Harnessing the Immune Responses. Adv Sci. 2021;8(16):2100446.
[9] TYLEK T, BLUM C, HRYNEVICH A, et al. Precisely defined fiber scaffolds with 40 μm porosity induce elongation driven M2-like polarization of human macrophages. Biofabrication. 2020;12(2):025007.
[10] SCHOENENBERGER AD, TEMPFER H, LEHNER C, et al. Macromechanics and polycaprolactone fiber organization drive macrophage polarization and regulate inflammatory activation of tendon in vitro and in vivo. Biomaterials. 2020;249:120034.
[11] DENG M, TAN J, HU C, et al. Modification of PLGA Scaffold by MSC-Derived Extracellular Matrix Combats Macrophage Inflammation to Initiate Bone Regeneration via TGF-β-Induced Protein. Adv Healthc Mater. 2021;10(12):e2100872.
[12] CHU C, LIU L, RUNG S, et al. Modulation of foreign body reaction and macrophage phenotypes concerning microenvironment. J Biomed Mater Res A. 2020;108(1):127-135.
[13] YUE L, SHI Y, SU X, et al. Matrix metalloproteinases inhibitors in idiopathic pulmonary fibrosis: Medicinal chemistry perspectives. Eur J Med Chem. 2021;224:113714.
[14] NOSKOVICOVA N, HINZ B, PAKSHIR P. Implant Fibrosis and the Underappreciated Role of Myofibroblasts in the Foreign Body Reaction. Cells. 2021;10(7): 1794.
[15] SCHUSTER R, ROCKEL JS, KAPOOR M, et al. The inflammatory speech of fibroblasts. Immunol Rev. 2021;302(1):126-146.
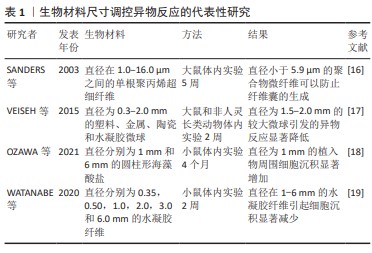
[16] SANDERS JE, ROCHEFORT JR. Fibrous encapsulation of single polymer microfibers depends on their vertical dimension in subcutaneous tissue. J Biomed Mater Res A. 2003;67(4):1181-1187.
[17] VEISEH O, DOLOFF JC, MA M, et al. Size- and shape-dependent foreign body immune response to materials implanted in rodents and non-human primates. Nat Mater. 2015;14(6):643-651.
[18] OZAWA F, NAGATA S, ODA H, et al. Lotus-root-shaped cell-encapsulated construct as a retrieval graft for long-term transplantation of human iPSC-derived β-cells. iScience. 2021;24(4):102309.
[19] WATANABE T, OKITSU T, OZAWA F, et al. Millimeter-thick xenoislet-laden fibers as retrievable transplants mitigate foreign body reactions for long-term glycemic control in diabetic mice. Biomaterials. 2020;255: 120162.
[20] HUH BK, KIM BH, KIM CR, et al. Elastic net of polyurethane strands for sustained delivery of triamcinolone around silicone implants of various sizes. Mater Sci Eng C Mater Biol Appl. 2020;109:110565.
[21] ZHOU L, LI K, LIU Y, et al. Living Cell-Derived Intelligent Nanobots for Precision Oncotherapy. Adv Funct Mater. 2024;34(10):2311857.
[22] IVANOVA E, FAYZULLIN A, MINAEV N, et al. Surface Topography of PLA Implants Defines the Outcome of Foreign Body Reaction: An In Vivo Study. Polymers (Basel). 2023;15(20):4119.
[23] LAMICHHANE S, ANDERSON JA, VIERHOUT T, et al. Polytetrafluoroethylene topographies determine the adhesion, activation, and foreign body giant cell formation of macrophages. J Biomed Mater Res A. 2017;105(9):2441-2450.
[24] MAJD H, SCHERER SS, BOO S, et al. Novel micropatterns mechanically control fibrotic reactions at the surface of silicone implants. Biomaterials. 2015;54:136-147.
[25] DWIVEDI R, KUMAR S, PANDEY R, et al. Polycaprolactone as biomaterial for bone scaffolds: Review of literature. J Oral Biol Craniofac Res. 2020; 10(1):381-388.
[26] ZHENG X, XIN L, LUO Y, et al. Near-Infrared-Triggered Dynamic Surface Topography for Sequential Modulation of Macrophage Phenotypes. ACS Appl Mater Interfaces. 2019;11(46):43689-43697.
[27] BARNSLEY GP, SIGURDSON LJ, BARNSLEY SE. Textured surface breast implants in the prevention of capsular contracture among breast augmentation patients: a meta-analysis of randomized controlled trials. Plast Reconstr Surg. 2006;117(7):2182-2190.
[28] ROBOTTI F, BOTTAN S, FRASCHETTI F, et al. A micron-scale surface topography design reducing cell adhesion to implanted materials. Sci Rep. 2018;8(1):10887.
[29] WILSON CJ, CLEGG RE, LEAVESLEY DI, et al. Mediation of biomaterial-cell interactions by adsorbed proteins: a review. Tissue Eng. 2005;11(1-2):1-18.
[30] LEE CH, KIM YJ, JANG JH, et al. Modulating macrophage polarization with divalent cations in nanostructured titanium implant surfaces. Nanotechnology. 2016;27(8):085101.
[31] WEI Q, BECHERER T, ANGIOLETTI-UBERTI S, et al. Protein interactions with polymer coatings and biomaterials. Angew Chem Int Ed Engl. 2014;53(31):8004-8031.
[32] CHEN S, LIU L, JIANG S. Strong resistance of oligo(phosphorylcholine) self-assembled monolayers to protein adsorption. Langmuir. 2006; 22(6):2418-2421.
[33] LEE SY, LEE Y, LE THI P, et al. Sulfobetaine methacrylate hydrogel-coated anti-fouling surfaces for implantable biomedical devices. Biomater Res. 2018;22:3.
[34] XIE Y, HU C, FENG Y, et al. Osteoimmunomodulatory effects of biomaterial modification strategies on macrophage polarization and bone regeneration. Regen Biomater. 2020;7(3):233-245.
[35] THEVENOT P, HU W, TANG L. Surface chemistry influences implant biocompatibility. Curr Top Med Chem. 2008;8(4):270-280.
[36] DUAN Y, ZHENG H, LI Z, et al. Unsaturated polyurethane films grafted with enantiomeric polylysine promotes macrophage polarization to a M2 phenotype through PI3K/Akt1/mTOR axis. Biomaterials. 2020;246:120012.
[37] VISALAKSHAN RM, MACGREGOR MN, SASIDHARAN S, et al. Biomaterial Surface Hydrophobicity-Mediated Serum Protein Adsorption and Immune Responses. ACS Appl Mater Interfaces. 2019;11(31):27615-27623.
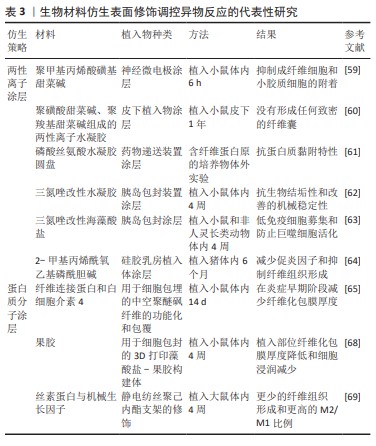
[38] QIAN Y, LI L, SONG Y, et al. Surface modification of nanofibrous matrices via layer-by-layer functionalized silk assembly for mitigating the foreign body reaction. Biomaterials. 2018;164:22-37.
[39] GIRAULT E, BIGUENET F, EIDENSCHENK A, et al. Fibrous biomaterials: Effect of textile topography on foreign body reaction. J Biomed Mater Res B Appl Biomater. 2021;109(10):1512-1524.
[40] WU L, ZHANG Z. Effects of implant and vocal fold stiffness on voice production after medialization laryngoplasty in an MRI-based vocal fold model. J Biomech. 2023;149:111483.
[41] GORI M, VADALÀ G, GIANNITELLI SM, et al. Biomedical and Tissue Engineering Strategies to Control Foreign Body Reaction to Invasive Neural Electrodes. Front Bioeng Biotechnol. 2021;9:659033.
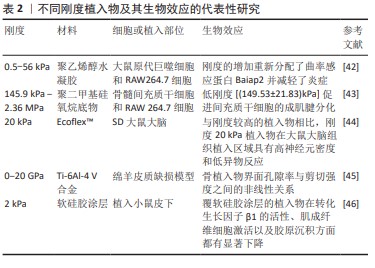
[42] NI Y, QI H, ZHANG F, et al. Macrophages modulate stiffness-related foreign body responses through plasma membrane deformation. Proc Natl Acad Sci U S A. 2023;120(3):e2213837120.
[43] SHENG R, LIU J, ZHANG W, et al. Material Stiffness in Cooperation with Macrophage Paracrine Signals Determines the Tenogenic Differentiation of Mesenchymal Stem Cells. Adv Sci. 2023;10(17):2206814.
[44] ZHANG EN, CLÉMENT J, ALAMERI A, et al. Mechanically Matched Silicone Brain Implants Reduce Brain Foreign Body Response. Adv Mater Technol. 2021;6(3):2000909.
[45] KELLY CN, WANG T, CROWLEY J, et al. High-strength, porous additively manufactured implants with optimized mechanical osseointegration. Biomaterials. 2021;279:121206.
[46] LODYGA M, HINZ B. TGF-β1 - A truly transforming growth factor in fibrosis and immunity. Semin Cell Dev Biol. 2020;101:123-139.
[47] LI R, FENG D, HAN S, et al. Macrophages and fibroblasts in foreign body reactions: How mechanical cues drive cell functions? Mater Today Bio. 2023;22:100783.
[48] PARK S, PARK M, KIM BH, et al. Acute suppression of TGF-ß with local, sustained release of tranilast against the formation of fibrous capsules around silicone implants. J Control Release. 2015;200:125-137.
[49] XIE X, DOLOFF JC, YESILYURT V, et al. Reduction of measurement noise in a continuous glucose monitor by coating the sensor with a zwitterionic polymer. Nat Biomed Eng. 2018;2(12):894-906.
[50] MILLER M, CHO JY, MCELWAIN K, et al. Corticosteroids prevent myofibroblast accumulation and airway remodeling in mice. Am J Physiol Lung Cell Mol Physiol. 2006;290(1):L162-169.
[51] FITZGERALD JJ. Suppression of scarring in peripheral nerve implants by drug elution. J Neural Eng. 2016;13(2):026006.
[52] PAKSHIR P, YOUNESI F, WOOTTON KA, et al. Controlled release of low-molecular weight, polymer-free corticosteroid coatings suppresses fibrotic encapsulation of implanted medical devices. Biomaterials. 2022;286:121586.
[53] CHANDORKAR Y, BHASKAR N, MADRAS G, et al. Long-term sustained release of salicylic acid from cross-linked biodegradable polyester induces a reduced foreign body response in mice. Biomacromolecules. 2015;16(2):636-649.
[54] MALIK AF, HOQUE R, OUYANG X, et al. Inflammasome components Asc and caspase-1 mediate biomaterial-induced inflammation and foreign body response. Proc Natl Acad Sci U S A. 2011;108(50): 20095-20100.
[55] CHEN T, YUAN J, DUNCANSON S, et al. Alginate encapsulant incorporating CXCL12 supports long-term allo- and xenoislet transplantation without systemic immune suppression. Am J Transplant. 2015;15(3):618-627.
[56] DESAI T, SHEA LD. Advances in islet encapsulation technologies. Nat Rev Drug Discov. 2017;16(5):338-350.
[57] FARAH S, DOLOFF JC, MÜLLER P, et al. Long-term implant fibrosis prevention in rodents and non-human primates using crystallized drug formulations. Nat Mater. 2019;18(8):892-904.
[58] YANG Q, WU B, ELES JR, et al. Zwitterionic Polymer Coating Suppresses Microglial Encapsulation to Neural Implants In Vitro and In Vivo. Adv Biosyst. 2020;4(6):e1900287.
[59] DONG D, TSAO C, HUNG HC, et al. High-strength and fibrous capsule-resistant zwitterionic elastomers. Sci Adv. 2021;7(1):eabc5442.
[60] LI B, YUAN Z, JAIN P, et al. De novo design of functional zwitterionic biomimetic material for immunomodulation. Sci Adv. 2020;6(22): eaba0754.
[61] CHEN X, YANG D. Functional zwitterionic biomaterials for administration of insulin. Biomater Sci. 2020;8(18):4906-4919.
[62] VEGAS AJ, VEISEH O, DOLOFF JC, et al. Corrigendum: Combinatorial hydrogel library enables identification of materials that mitigate the foreign body response in primates. Nat Biotechnol. 2016;34(6): 666.
[63] KANG S, KIM J, KIM S, et al. Efficient reduction of fibrous capsule formation around silicone breast implants densely grafted with 2-methacryloyloxyethyl phosphorylcholine (MPC) polymers by heat-induced polymerization. Biomater Sci. 2020;8(6):1580-1591.
[64] TAN RP, HALLAHAN N, KOSOBRODOVA E, et al. Bioactivation of Encapsulation Membranes Reduces Fibrosis and Enhances Cell Survival. ACS Appl Mater Interfaces. 2020;12(51):56908-56923.
[65] SAHASRABUDHE NM, BEUKEMA M, TIAN L, et al. Dietary Fiber Pectin Directly Blocks Toll-Like Receptor 2-1 and Prevents Doxorubicin-Induced Ileitis. Front Immunol. 2018;9:383.
[66] FAN W, FU D, ZHANG L, et al. Enoxaparin sodium bone cement plays an anti-inflammatory immunomodulatory role by inducing the polarization of M2 macrophages. J Orthop Surg Res. 2023;18(1):380.
[67] HU S, MARTINEZ-GARCIA FD, MOEUN BN, et al. An immune regulatory 3D-printed alginate-pectin construct for immunoisolation of insulin producing β-cells. Mater Sci Eng C Mater Biol Appl. 2021; 123:112009.
[68] SONG Y, LI L, ZHAO W, et al. Surface modification of electrospun fibers with mechano-growth factor for mitigating the foreign-body reaction. Bioact Mater. 2021;6(9):2983-2998.
[69] BADYLAK SF. TISSUE REGENERATION.A scaffold immune microenvironment. Science (New York, N.Y.). 2016;352(6283):298. |