Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (4): 849-857.doi: 10.12307/2025.986
Previous Articles Next Articles
A prediction model for sarcopenia in postmenopausal women: information analysis based on the China Health and Retirement Longitudinal Study database
Li Guangzheng1, Li Wei1, Zhang Bochun1, Ding Haoqin1, Zhou Zhongqi2, Li Gang3, Liang Xuezhen1, 3
- 1First Clinical Medical College, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China; 2School of Traditional Chinese Medicine, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China; 3Department of Microscopic Orthopedics, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan 250014, Shandong Province, China
-
Received:2024-10-10Accepted:2024-12-31Online:2026-02-08Published:2025-05-16 -
Contact:Liang Xuezhen, PhD, Associate professor, Master’s supervisor, First Clinical Medical College, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China; Department of Microscopic Orthopedics, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan 250014, Shandong Province, China Co-corresponding author: Li Gang, PhD, Professor, Chief physician, Doctoral supervisor, Department of Microscopic Orthopedics, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan 250014, Shandong Province, China -
About author:Li Guangzheng, Master, First Clinical Medical College, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China -
Supported by:the National Natural Science Foundation of China (General Program), No. 82074453 (to LG); the National Natural Science Foundation of China (Youth Program), No. 82205154 (to LXZ); the Shandong Provincial Natural Science Foundation of China (Youth Program), Nos. ZR2021QH004 and ZR2024MH156 (both to LXZ)
CLC Number:
Cite this article
Li Guangzheng, Li Wei, Zhang Bochun, Ding Haoqin, Zhou Zhongqi, Li Gang, Liang Xuezhen. A prediction model for sarcopenia in postmenopausal women: information analysis based on the China Health and Retirement Longitudinal Study database[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 849-857.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

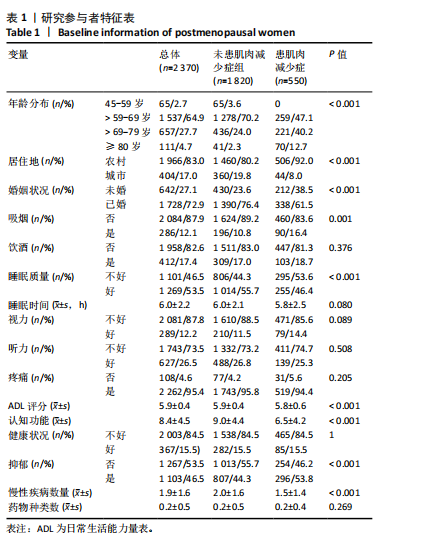
2.1 研究数据 共有2 370名绝经后女性纳入此次研究,为消除量纲影响、增加模型的稳定性,对数据进行了归一化处理。参与者的人口统计学和临床特征如表1所示。其中,有1 820名未患肌肉减少症,550名为患有肌肉减少症,肌肉减少症的患病率为23.21%;45-59岁65名,> 59-69岁1 537名,> 69-79岁657名,≥80岁111名。未患肌肉减少症组与患肌肉减少症组在年龄分布(P < 0.001)、居住地(P < 0.001)、婚姻状况(P < 0.001)、吸烟(P=0.001)、睡眠质量(P < 0.001)、ADL评分(P < 0.001)、认知功能(P < 0.001)、抑郁(P < 0.001)、慢性疾病数量(P < 0.001)方面存在显著差异。筛选后的数据按照7∶3的比例随机分为训练集(n=1 659)和验证集(n=711)。"
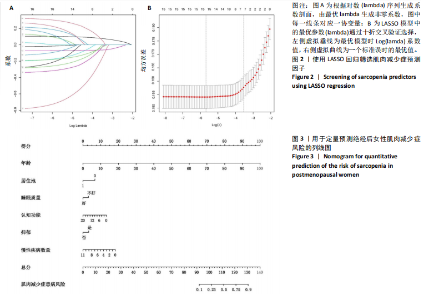
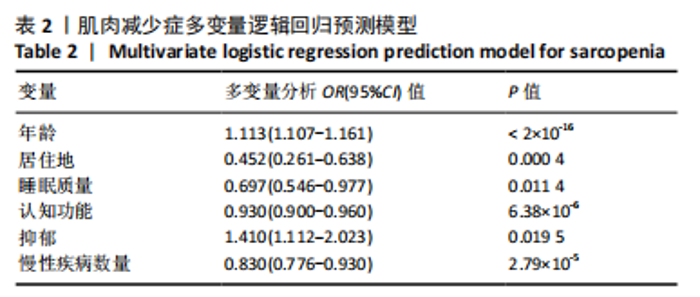
2.2 预测因子选择 通过LASSO回归预测因子筛选结果如图2所示,将与肌肉减少症相关的预测因子纳入多变量Logistic回归模型,以P < 0.05为标准筛选出年龄(P < 2×10-16)、居住地(P=0.000 4)、睡眠质量(P=0.011 4)、认知功能(P=6.38×10-6)、抑郁(P=0.019 5)、慢性疾病数量(P=2.79×10-5)进行后续分析(表2)。 2.3 预测模型开发 纳入年龄(P < 2×10-16)、居住地(P= 0.000 4)、睡眠质量(P=0.011 4)、认知功能(P=6.38×10-6)、抑郁(P=0.019 5)、慢性疾病数量(P=2.79×10-5)作为预测因子,构建预测模型并通过列线图展示(图3),可定量分析绝经后女性肌肉减少症患病风险。"
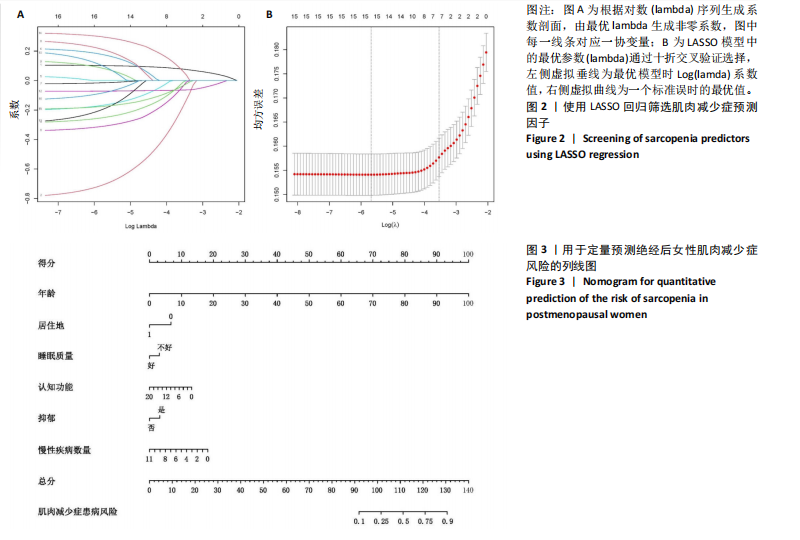

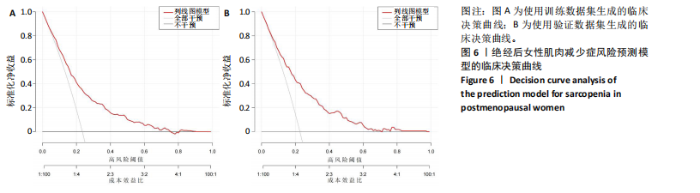
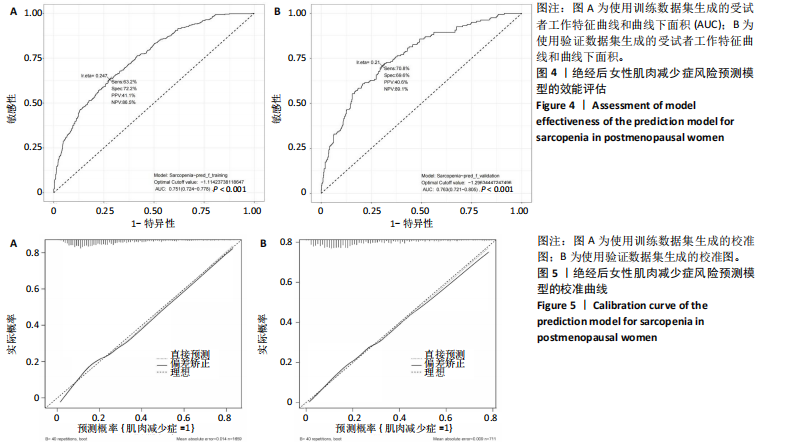
2.4 验证预测模型 通过AUC值评估训练集和验证集预测模型的效能。预测模型在训练集的AUC值为0.751(95%CI=0.724-0.778,P < 0.001),特异性为72.2%,敏感性为63.2%;在验证集的AUC值为0.763(95%CI=0.721-0.805,P < 0.001),特异性为69.6%,敏感性为70.8%(图4)。预测模型在训练集和验证集中的表现具有一定的相似性,且具有一定的区分能力和预测价值,能够在一定程度上预测绝经后女性肌肉减少症的患病风险。 2.5 校准预测模型 通过校准图和Hosmer-Lemeshow拟合优度检验来评估预测模型(P > 0.05提示模型具有良好的拟合度),结果表明模型对训练集(χ2=8.945 7,df=8,P=0.346 9)和验证集(χ2=5.417 6,df=8,P=0.712 1)都有较好的拟合度(图5)。基于多因素逻辑回归模型的校准曲线显示预测模型在训练集和验证集中的预测效能具有一致性。 2.6 临床有效性评估 利用决策曲线分析评估模型的临床有效性,结果显示预测模型在训练集和验证集均高于两种极端情况且具有一致性(图6),说明此次研究开发的临床预测模型具有较高的净收益和预测准确性。"
| [1] ROSENBERG IH. Sarcopenia: origins and clinical relevance. J Nutr. 1997; 127(5 Suppl):990s-991s. [2] BEAUDART C, DEMONCEAU C, REGINSTER JY, et al. Sarcopenia and health-related quality of life: A systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2023;14(3):1228-1243. [3] MIELGO-AYUSO J, FERNÁNDEZ-LÁZARO D. Sarcopenia, Exercise and Quality of Life. Int J Environ Res Public Health. 2021;18(10):5156. [4] JIMENEZ-GUTIERREZ GE, MARTÍNEZ-GÓMEZ LE, MARTÍNEZ-ARMENTA C, et al. Molecular Mechanisms of Inflammation in Sarcopenia: Diagnosis and Therapeutic Update. Cells. 2022;11(15):2359. [5] CHEN LK, LIU LK, WOO J, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15(2):95-101. [6] CHEN LK, WOO J, ASSANTACHAI P, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatmen. J Am Med Dir Assoc. 2020;21(3):300-307.e302. [7] LAVIANO A, GORI C, RIANDA S. Sarcopenia and nutrition. Adv Food Nutr Res. 2014;71:101-136. [8] PAPADOPOULOU SK. Sarcopenia: A Contemporary Health Problem among Older Adult Populations. Nutrients. 2020;12(5):1293. [9] ALBANO D, MESSINA C, VITALE J, et al. Imaging of sarcopenia: old evidence and new insights. Eur Radiol. 2020;30(4):2199-2208. [10] MINETTO MA, BUSSO C, GAMERRO G, et al. Quantitative assessment of volumetric muscle loss: Dual-energy X-ray absorptiometry and ultrasonography. Curr Opin Pharmacol. 2021;57:148-156. [11] JIMENEZ-GUTIERREZ GE, MARTÍNEZ-GÓMEZ LE, MARTÍNEZ-ARMENTA C, et al. Molecular Mechanisms of Inflammation in Sarcopenia: Diagnosis and Therapeutic Update. Cells. 2022;11(15):2359. [12] CHENG KY, CHOW SK, HUNG VW, et al. Diagnosis of sarcopenia by evaluating skeletal muscle mass by adjusted bioimpedance analysis validated with dual-energy X-ray absorptiometry. J Cachexia Sarcopenia Muscle. 2021;12(6):2163-2173. [13] BEAUDART C, MCCLOSKEY E, BRUYÈRE O, et al. Sarcopenia in daily practice: assessment and management. BMC Geriatr. 2016;16(1):170. [14] CRUZ-JENTOFT AJ, SAYER AA. Sarcopenia. Lancet. 2019;393(10191): 2636-2646. [15] CAPPOLA AR, SHOBACK DM. Osteoporosis Therapy in Postmenopausal Women With High Risk of Fracture. JAMA. 2016;316(7):715-716. [16] BERTOMEU-GONZALEZ V, CORDERO A, RUIZ-NODAR JM, et al. Risk factors for major adverse cardiovascular events in postmenopausal women: UK Biobank prospective cohort study. Atherosclerosis. 2023; 386:117372. [17] HENDRYX M, NICHOLSON W, MANSON JE, et al. Social Relationships and Risk of Type 2 Diabetes Among Postmenopausal Women. J Gerontol B Psychol Sci Soc Sci. 2020;75(7):1597-1608. [18] 陶敏芳.始于围绝经期的更年期和老年期妇女健康保健策略[J].上海医学,2021,44(6):388-390. [19] DIVARIS E, ANAGNOSTIS P, GKEKAS NK, et al. Early menopause and premature ovarian insufficiency may increase the risk of sarcopenia: A systematic review and meta-analysis. Maturitas. 2023;175:107782. [20] LU L, TIAN L. Postmenopausal osteoporosis coexisting with sarcopenia: the role and mechanisms of estrogen. J Endocrinol. 2023; 259(1):e230116. [21] GERACI A, CALVANI R, FERRI E, et al. Sarcopenia and Menopause: The Role of Estradiol. Front Endocrinol (Lausanne). 2021;12:682012. [22] ANAGNOSTIS P, SIOLOS P, GKEKAS NK, et al. Association between age at menopause and fracture risk: a systematic review and meta-analysis. Endocrine. 2019;63(2):213-224. [23] LIU JH. Sarcopenia and menopause. Menopause. 2023;30(2):119-120. [24] SI Y, HANEWALD K, CHEN S, et al. Life-course inequalities in intrinsic capacity and healthy ageing, China. Bull World Health Organ. 2023; 101(5):307-316c. [25] HU Y, PENG W, REN R, et al. Sarcopenia and mild cognitive impairment among elderly adults: The first longitudinal evidence from CHARLS. J Cachexia Sarcopenia Muscle. 2022;13(6):2944-2952. [26] ZHAO Y, HU Y, SMITH JP, et al. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43(1) 61-68. [27] WU X, LI X, XU M, et al. Sarcopenia prevalence and associated factors among older Chinese population: Findings from the China Health and Retirement Longitudinal Study. PLoS One. 2021;16(3):e0247617. [28] ZHANG L, GUO L, WU H, et al. Role of physical performance measures for identifying functional disability among Chinese older adults: Data from the China Health and Retirement Longitudinal Study. PLoS One. 2019;14(4):e0215693. [29] WEN X, WANG M, JIANG CM, et al. Anthropometric equation for estimation of appendicular skeletal muscle mass in Chinese adults. Asia Pac J Clin Nutr. 2011;20(4):551-556. [30] YANG M, HU X, WANG H, et al. Sarcopenia predicts readmission and mortality in elderly patients in acute care wards: a prospective study. J Cachexia Sarcopenia Muscle. 2017;8(2):251-258. [31] HUANG W, ZHOU Y. Effects of education on cognition at older ages: evidence from China’s Great Famine. Soc Sci Med. 2013;98:54-62. [32] BU F, DENG XH, ZHAN NN, et al. Development and validation of a risk prediction model for frailty in patients with diabetes. BMC Geriatr. 2023;23(1):172. [33] HU JY, WANG Y, TONG XM, et al. When to consider logistic LASSO regression in multivariate analysis? Eur J Surg Oncol. 2021;47(8):2206. [34] LYU J, LI Z, WEI H, et al. A potent risk model for predicting new-onset acute coronary syndrome in patients with type 2 diabetes mellitus in Northwest China. Acta Diabetol. 2020;57(6):705-713. [35] TOURNADRE A, VIAL G, CAPEL F, et al. Sarcopenia. Joint Bone Spine. 2019;86(3):309-314. [36] DAMLUJI AA, ALFARAIDHY M, ALHAJRI N, et al. Sarcopenia and Cardiovascular Diseases. Circulation. 2023;147(20):1534-1553. [37] WANG LT, HUANG WC, HUNG YC, et al. Association between Depressive Symptoms and Risk of Sarcopenia in Taiwanese Older Adults. J Nutr Health Aging. 2021;25(6):790-794. [38] YUAN S, LARSSON SC. Epidemiology of sarcopenia: Prevalence, risk factors, and consequences. Metabolism. 2023;144:155533. [39] WILKINSON DJ, PIASECKI M, ATHERTON PJ. The age-related loss of skeletal muscle mass and function: Measurement and physiology of muscle fibre atrophy and muscle fibre loss in humans. Ageing Res Rev. 2018;47:123-132. [40] CURTIS E, LITWIC A, COOPER C, et al. Determinants of Muscle and Bone Aging. J Cell Physiol. 2015;230(11):2618-2625. [41] MALTAIS ML, DESROCHES J, DIONNE IJ. Changes in muscle mass and strength after menopause. J Musculoskelet Neuronal Interact. 2009;9(4):186-197. [42] LU X, CHU H, WANG L, et al. Age- and sex-related differences in muscle strength and physical performance in older Chinese. Aging Clin Exp Res. 2020;32(5):877-883. [43] HAH YS, LEE WK, LEE S, et al. β-Sitosterol Attenuates Dexamethasone-Induced Muscle Atrophy via Regulating FoxO1-Dependent Signaling in C2C12 Cell and Mice Model. Nutrients. 2022;14(14):2894. [44] NISHIKAWA H, FUKUNISHI S, ASAI A, et al. Pathophysiology and mechanisms of primary sarcopenia (Review). Int J Mol Med. 2021; 48(2):156. [45] LU L, MAO L, FENG Y, et al. Effects of different exercise training modes on muscle strength and physical performance in older people with sarcopenia: a systematic review and meta-analysis. BMC Geriatr. 2021;21(1):708. [46] WANG HH, SUN YN, QU TQ, et al. Nobiletin Prevents D-Galactose-Induced C2C12 Cell Aging by Improving Mitochondrial Function. Int J Mol Sci. 2022;23(19):11963. [47] CRITCHLOW AJ, HIAM D, WILLIAMS R, et al. The role of estrogen in female skeletal muscle aging: A systematic review. Maturitas. 2023; 178:107844. [48] MANGAN G, IQBAL S, HUBBARD A, et al. Delay in post-ovariectomy estrogen replacement negates estrogen-induced augmentation of post-exercise muscle satellite cell proliferation. Can J Physiol Pharmacol. 2015;93(11):945-951. [49] PELLEGRINO A, TIIDUS PM, VANDENBOOM R. Mechanisms of Estrogen Influence on Skeletal Muscle: Mass, Regeneration, and Mitochondrial Function. Sports Med. 2022;52(12):2853-2869. [50] FAN L, WANG Z, ZHAO Y, et al. Urban-Rural Disparities in Knowledge, Use and Perceived Benefits of Nutrition Labels in China: Evidence from 10 Provinces. Nutrients. 2023;15(5):1171. [51] 李建新,李春华.城乡老年人口健康差异研究[J].人口学刊,2014, 36(5):37-47. [52] CORBO I, FORTE G, FAVIERI F, et al. Poor Sleep Quality in Aging: The Association with Mental Health. Int J Environ Res Public Health. 2023;20(3):1661. [53] PIOVEZAN RD, ABUCHAM J, DOS SANTOS RV, et al. The impact of sleep on age-related sarcopenia: Possible connections and clinical implications. Ageing Res Rev. 2015;23(Pt B):210-220. [54] RAWTAER I, MAHENDRAN R, CHAN HY, et al. A nonpharmacological approach to improve sleep quality in older adults. Asia Pac Psychiatry. 2018;10(2):e12301. [55] CHANG KV, HSU TH, WU WT, et al. Association Between Sarcopenia and Cognitive Impairment: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc. 2016;17(12):1164.e1167-1164.e1115. [56] ROBERTSON DA, SAVVA GM, KENNY RA. Frailty and cognitive impairment--a review of the evidence and causal mechanisms. Ageing Res Rev. 2013;12(4):840-851. [57] CHOU MY, NISHITA Y, NAKAGAWA T, et al. Role of gait speed and grip strength in predicting 10-year cognitive decline among community-dwelling older people. BMC Geriatr. 2019;19(1):186. [58] LI Z, TONG X, MA Y, et al. Prevalence of depression in patients with sarcopenia and correlation between the two diseases: systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2022;13(1):128-144. [59] LIALY HE, MOHAMED MA, ABDALLATIF LA, et al. Effects of different physiotherapy modalities on insomnia and depression in perimenopausal, menopausal, and post-menopausal women: a systematic review. BMC Womens Health. 2023;23(1):363. [60] LEACH LS, CHRISTENSEN H, MACKINNON AJ, et al. Gender differences in depression and anxiety across the adult lifespan: the role of psychosocial mediators. Soc Psychiatry Psychiatr Epidemiol. 2008;43(12):983-998. [61] KESSLER RC, MCGONAGLE KA, ZHAO S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8-19. [62] KRIS-ETHERTON PM, PETERSEN KS, HIBBELN JR, et al. Nutrition and behavioral health disorders: depression and anxiety. Nutr Rev. 2021;79(3):247-260. [63] AROSIO B, CESARI M. Nutrition and Muscle Health. Nutrients. 2021; 13(3):797. [64] ROSHANAEI-MOGHADDAM B, KATON WJ, RUSSO J. The longitudinal effects of depression on physical activity. Gen Hosp Psychiatry. 2009; 31(4):306-315. [65] PARK H, KIM K. Depression and Its Association with Health-Related Quality of Life in Postmenopausal Women in Korea. Int J Environ Res Public Health. 2018;15(11):2327. [66] ZHANG X, ZHAO Y, CHEN S, et al. Anti-diabetic drugs and sarcopenia: emerging links, mechanistic insights, and clinical implications. J Cachexia Sarcopenia Muscle. 2021;12(6):1368-1379. [67] VAN BAKEL SIJ, GOSKER HR, LANGEN RC, et al. Towards Personalized Management of Sarcopenia in COPD. Int J Chron Obstruct Pulmon Dis. 2021;16:25-40. [68] TANDON P, MONTANO-LOZA AJ, LAI JC, et al. Sarcopenia and frailty in decompensated cirrhosis. J Hepatol. 2021;75 Suppl 1(Suppl 1): S147-s162. [69] YANG J, JIANG F, YANG M, et al. Sarcopenia and nervous system disorders. J Neurol. 2022; 269(11):5787-5797. [70] NOCE A, MARRONE G, OTTAVIANI E, et al. Uremic Sarcopenia and Its Possible Nutritional Approach. Nutrients. 2021;13(1):147. [71] MO YH, SU YD, DONG X, et al. Development and Validation of a Nomogram for Predicting Sarcopenia in Community-Dwelling Older Adults. J Am Med Dir Assoc. 2022;23(5):715-721. [72] HAN S, ZHANG F, YU H, et al. Systemic inflammation accelerates the adverse effects of air pollution on metabolic syndrome: Findings from the China health and Retirement Longitudinal Study (CHARLS). Environ Res. 2022;215(Pt 1):114340. |
| [1] | Chen Ju, Zheng Jinchang, Liang Zhen, Huang Chengshuo, Lin Hao, Zeng Li. Effect and mechanism of beta-caryophyllene in mice with osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1341-1347. |
| [2] | Wen Guangwei, Zhen Yinghao, Zheng Taikeng, Zhou Shuyi, Mo Guoye, Zhou Tengpeng, Li Haishan, Lai Yiyi. Effects and mechanisms of isoginkgetin on osteoclastogenesis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1348-1358. |
| [3] | Li Linzhen, Jiao Hongzhuo, Chen Weinan, Zhang Mingzhe, Wang Jianlong, Zhang Juntao. Effect of icariin-containing serum on lipopolysaccharide-induced inflammatory damage in human chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1368-1374. |
| [4] | Pan Hongfei, Zhuang Zhenbing, Xu Baiyun, Yang Zhangyang, Lin Kairui, Zhan Bingqing, Lan Jinghan, Gao Heng, Zhang Nanbo, Lin Jiayu. Inhibitory effects of different concentrations of auranofin on M1 macrophage function and its therapeutic potential in diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1390-1397. |
| [5] | Peng Zhiwei, Chen Lei, Tong Lei. Luteolin promotes wound healing in diabetic mice: roles and mechanisms [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1398-1406. |
| [6] | Lyu Xiaofan, Huang Yi, Ding Liucheng . Mitochondrial mechanism and intervention therapy in diabetic cystopathy [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1508-1515. |
| [7] | Yang Zhijie, Zhao Rui, Yang Haolin, Li Xiaoyun, Li Yangbo, Huang Jiachun, Lin Yanping, Wan Lei, HuangHongxing. Postmenopausal osteoporosis: predictive values of muscle mass, grip strength, and appendicular skeletal muscle index [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1073-1080. |
| [8] | Yin Yongcheng, Zhao Xiangrui, Yang Zhijie, Li Zheng, Li Fang, Ning Bin. Effect and mechanism of peroxiredoxin 1 in microglial inflammation after spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1106-1113. |
| [9] | Zhang Jiuxuan, Zhang Jinnan, Sui Xiaofan, Pei Xiaxia, Wei Jianhong, Su Qiang, Li Tian. Effects of ammonia poisoning on cognitive behavior and hippocampal synaptic damage in mice [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1122-1128. |
| [10] | Sun Yajie, Zhao Xinchen, Bo Shuangling. Spatiotemporal expression of bone morphologic protein 7 in mouse kidney development [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1156-1161. |
| [11] | Li Haojing, Wang Xin, Song Chenglin, Zhang Shengnan, Chen Yunxin. Therapeutic efficacy of extracorporeal shock wave therapy in the upper trapezius muscle area combined with exercise control training in patients with chronic non-specific neck pain [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1162-1170. |
| [12] | Liu Yu, Lei Senlin, Zhou Jintao, Liu Hui, Li Xianhui. Mechanisms by which aerobic and resistance exercises improve obesity-related cognitive impairment [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1171-1183. |
| [13] | Yu Huifen, Mo Licun, Cheng Leping. The position and role of 5-hydroxytryptamine in the repair of tissue injury [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1196-1206. |
| [14] | Wang Zhengye, Liu Wanlin, Zhao Zhenqun. Advance in the mechanisms underlying miRNAs in steroid-induced osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1207-1214. |
| [15] | Bu Yangyang, Ning Xinli, Zhao Chen. Intra-articular injections for the treatment of osteoarthritis of the temporomandibular joint: different drugs with multiple combined treatment options [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1215-1224. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||