Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (6): 1390-1397.doi: 10.12307/2026.555
Previous Articles Next Articles
Inhibitory effects of different concentrations of auranofin on M1 macrophage function and its therapeutic potential in diabetic wound healing
Pan Hongfei1, Zhuang Zhenbing1, Xu Baiyun1, Yang Zhangyang1, Lin Kairui1, Zhan Bingqing1, Lan Jinghan1, Gao Heng1, Zhang Nanbo1, #br# Lin Jiayu2#br#
- 1Fujian Medical University, Fuzhou 350000, Fujian Province, China; 2Department of Endocrinology, The Second Affiliated Hospital of Fujian Medical University, Quanzhou 362000, Fujian Province, China
-
Received:2024-11-01Accepted:2025-01-20Online:2026-02-28Published:2025-07-14 -
Contact:Lin Jiayu, MD, Associate chief physician, Department of Endocrinology, The Second Affiliated Hospital of Fujian Medical University, Quanzhou 362000, Fujian Province, China -
About author:Pan Hongfei, Fujian Medical University, Fuzhou 350000, Fujian Province, China Zhuang Zhenbing, Fujian Medical University, Fuzhou 350000, Fujian Province, China Pan Hongfei and Zhuang Zhenbing contributed equally to this work. -
Supported by:Fujian Provincial Natural Science Foundation, No. 2023J01739 (to LJY); “Thematic Research Training” Project of Class 2022 Clinical Medicine (“5+3” Integration), No. 05300419 (to PHF)
CLC Number:
Cite this article
Pan Hongfei, Zhuang Zhenbing, Xu Baiyun, Yang Zhangyang, Lin Kairui, Zhan Bingqing, Lan Jinghan, Gao Heng, Zhang Nanbo, Lin Jiayu. Inhibitory effects of different concentrations of auranofin on M1 macrophage function and its therapeutic potential in diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1390-1397.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

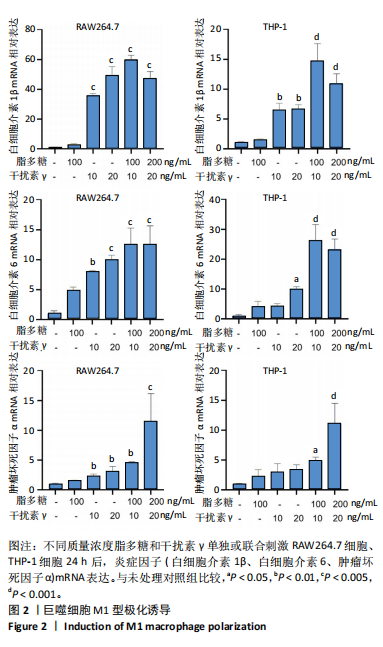
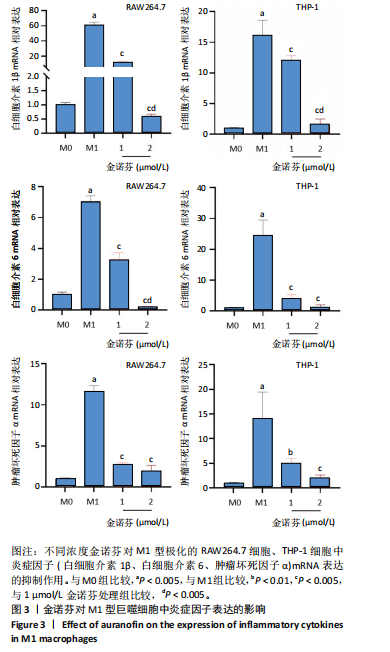
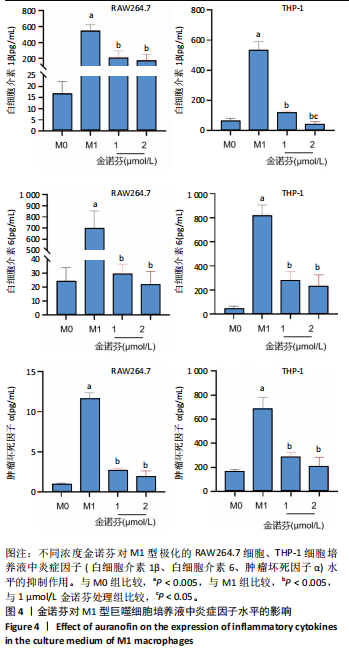
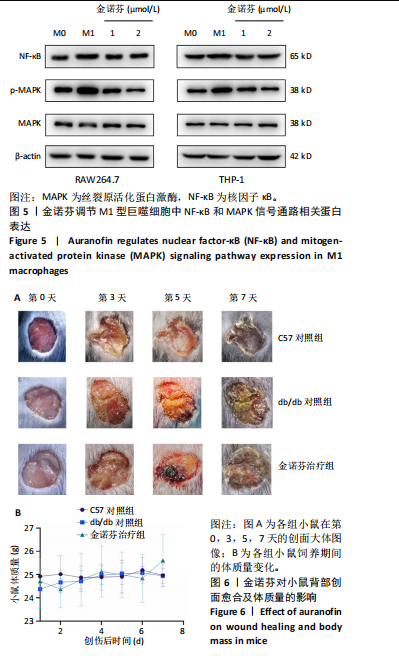
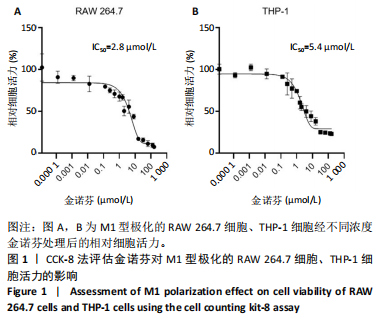
2.1 细胞存活率 对于M1型极化的RAW 264.7细胞(图1A),金诺芬在浓度为0.000 1-1 μmol/L时,细胞活力保持接近100%,表明金诺芬在这一浓度范围内对细胞活力影响较小。当金诺芬浓度超过1 μmol/L时,细胞活力开始显著下降,尤其在10 μmol/L及以上浓度,抑制效果明显,呈剂量依赖性。对于M1型极化的THP-1细胞(图1B),低浓度金诺芬处理后细胞活力维持较高水平,随着浓度增加,细胞活力逐渐下降,10 μmol/L及以上浓度时,细胞活力显著降低,趋势与M1型极化的RAW 264.7细胞类似。金诺芬对M1型极化的RAW 264.7和THP-1细胞系均表现出剂量依赖性的抑制作用,且在高浓度时对细胞活力有显著的抑制效果,后续细胞实验选择1 μmol/L和2 μmol/L金诺芬进行干预。 2.2 金诺芬抑制M1型巨噬细胞炎症因子表达 干扰素γ(10 ng/mL)与脂多糖(100 ng/mL)联合使用显著促进了两种巨噬细胞向M1型极化,表现为炎症因子mRNA表达显著增强(图2)。在此基础上,对M1型极化的RAW264.7细胞、THP-1细胞进行不同浓度金诺芬(1,2 μmol/L)处理24 h,结果显示金诺芬能显著抑制M1型巨噬细胞中炎症因子mRNA表达(图3)。 通过ELISA检测细胞培养上清液中白细胞介素1β、白细胞介素6、肿瘤坏死因子α水平,结果显示,在M1状态下,这些炎症因子的水平显著高于M0状态,表明M1型巨噬细胞具有更高的炎症活性。金诺芬在1 μmol/L和2 μmol/L浓度下,能够显著降低M1型极化的RAW264.7细胞、THP-1细胞中炎症因子水平,见图4。 2.3 金诺芬对M1型极化的RAW264.7和THP-1细胞中NF-κB(p65)、p-MAPK和总MAPK蛋白表达的影响 诱导的M1型巨噬细胞中,NF-κB和p-MAPK蛋白表达水平升高。金诺芬处理后,NF-κB(p65)和p-MAPK蛋白表达下降,见图5,提示金诺芬可能是通过抑制NF-κB以及MAPK信号通路,调节M1型巨噬细胞中白细胞介素1β、白细胞介素6、肿瘤坏死因子α免疫因子分泌。 2.4 各组小鼠背部创面愈合情况 图6A为小鼠背部皮肤创面大体图像,在创伤后第3-7天,金诺芬治疗组的创面面积较db/db对照组显著缩小。图6B显示3组小鼠在饲养期间的体质量差异无显著性意义,表明在此浓度下金诺芬对小鼠没有明显毒性。"
| [1] MCDERMOTT K, FANG M, BOULTON AJM, et al. Etiology, Epidemiology, and Disparities in the Burden of Diabetic Foot Ulcers. Diabetes Care. 2023;46(1):209-221. [2] LOUISELLE AE, NIEMIEC SM, ZGHEIB C, et al. Macrophage polarization and diabetic wound healing. Transl Res. 2021;236:109-116. [3] QI X, CAI E, XIANG Y, et al. An Immunomodulatory Hydrogel by Hyperthermia-Assisted Self-Cascade Glucose Depletion and ROS Scavenging for Diabetic Foot Ulcer Wound Therapeutics. Adv Mater. 2023;35(48):e2306632. [4] LV D, CAO X, ZHONG L, et al. Targeting phenylpyruvate restrains excessive NLRP3 inflammasome activation and pathological inflammation in diabetic wound healing. Cell Rep Med. 2023;4(8): 101129. [5] AITCHESON SM, FRENTIU FD, HURN SE, et al. Skin Wound Healing: Normal Macrophage Function and Macrophage Dysfunction in Diabetic Wounds. Molecules. 2021;26(16):4917. [6] CELIK C, LEE STT, TANOTO FR, et al. Decoding the complexity of delayed wound healing following Enterococcus faecalis infection. Elife. 2024;13:RP95113. [7] KANG Y, XU L, DONG J, et al. Programmed microalgae-gel promotes chronic wound healing in diabetes. Nat Commun. 2024;15(1):1042. [8] YI WJ, YUAN Y, BAO Q, et al. Analyzing Immune Cell Infiltration and Copper Metabolism in Diabetic Foot Ulcers. J Inflamm Res. 2024;17: 3143-3157. [9] SAWAYA AP, STONE RC, BROOKS SR, et al. Deregulated immune cell recruitment orchestrated by FOXM1 impairs human diabetic wound healing. Nat Commun. 2020;11(1):4678. [10] CLAYTON SM, SHAFIKHANI SH, SOULIKA AM. Macrophage and Neutrophil Dysfunction in Diabetic Wounds. Adv Wound Care (New Rochelle). 2024;13(9):463-484. [11] LI HD, YOU YK, SHAO BY, et al. Roles and crosstalks of macrophages in diabetic nephropathy. Front Immunol. 2022;13:1015142. [12] HASSANSHAHI A, MORADZAD M, GHALAMKARI S, et al. Macrophage-Mediated Inflammation in Skin Wound Healing. Cells. 2022;11(19):2953. [13] LIU W, YU M, XIE D, et al. Melatonin-stimulated MSC-derived exosomes improve diabetic wound healing through regulating macrophage M1 and M2 polarization by targeting the PTEN/AKT pathway. Stem Cell Res Ther. 2020;11(1):259. [14] CHEN J, MA H, MENG Y, et al. Analysis of the mechanism underlying diabetic wound healing acceleration by Calycosin-7-glycoside using network pharmacology and molecular docking. Phytomedicine. 2023; 114:154773. [15] GENG K, MA X, JIANG Z, et al. High glucose-induced STING activation inhibits diabetic wound healing through promoting M1 polarization of macrophages. Cell Death Discov. 2023;9(1):136. [16] KANG ML, KIM HS, YOU J, et al. Hydrogel cross-linking-programmed release of nitric oxide regulates source-dependent angiogenic behaviors of human mesenchymal stem cell. Sci Adv. 2020;6(9):eaay5413. [17] LIU Y, ZHANG X, YANG L, et al. Proteomics and transcriptomics explore the effect of mixture of herbal extract on diabetic wound healing process. Phytomedicine. 2023;116:154892. [18] MUKHERJEE S, IM SS. Impact of tibial transverse transport in tissue regeneration and wound healing with perspective on diabetic foot ulcers. World J Diabetes. 2024;15(5):810-813. [19] YANG J, XIONG G, HE H, et al. SFRP2 modulates functional phenotype transition and energy metabolism of macrophages during diabetic wound healing. Front Immunol. 2024;15:1432402. [20] ZENG R, LV B, LIN Z, et al. Neddylation suppression by a macrophage membrane-coated nanoparticle promotes dual immunomodulatory repair of diabetic wounds. Bioact Mater. 2024;34:366-380. [21] SHEN S, SHEN J, LUO Z, et al. Molecular mechanisms and clinical implications of the gold drug auranofin. Coord Chem Rev. 2023;493: 215323. [22] LIU H, SHUKLA S, VERA-GONZÁLEZ N, et al. Auranofin Releasing Antibacterial and Antibiofilm Polyurethane Intravascular Catheter Coatings. Front Cell Infect Microbiol. 2019;9:37. [23] LUO J, SHANG Y, ZHAO N, et al. Hypoxia-responsive micelles deprive cofactor of stearoyl-CoA desaturase-1 and sensitize ferroptotic ovarian cancer therapy. Biomaterials. 2025;314:122820. [24] JOO MK, SHIN S, YE DJ, et al. Combined treatment with auranofin and trametinib induces synergistic apoptosis in breast cancer cells. J Toxicol Environ Health A. 2021;84(2):84-94. [25] KINOSHITA H, SHIMOZATO O, ISHII T, et al. The Thioredoxin Reductase Inhibitor Auranofin Suppresses Pulmonary Metastasis of Osteosarcoma, But Not Local Progression. Anticancer Res. 2021;41(10):4947-4955. [26] LEE SM, KOH DH, JUN DW, et al. Auranofin attenuates hepatic steatosis and fibrosis in nonalcoholic fatty liver disease via NRF2 and NF- κB signaling pathways. Clin Mol Hepatol. 2022;28(4):827-840. [27] STEERS GJ, CHEN GY, O’LEARY BR, et al. Auranofin and Pharmacologic Ascorbate as Radiomodulators in the Treatment of Pancreatic Cancer. Antioxidants (Basel). 2022;11(5):971. [28] YANG L, WANG H, YANG X, et al. Auranofin mitigates systemic iron overload and induces ferroptosis via distinct mechanisms. Signal Transduct Target Ther. 2020;5(1):138. [29] HWANGBO H, JI SY, KIM MY, et al. Anti-Inflammatory Effect of Auranofin on Palmitic Acid and LPS-Induced Inflammatory Response by Modulating TLR4 and NOX4-Mediated NF-κB Signaling Pathway in RAW264.7 Macrophages. Int J Mol Sci. 2021;22(11):5920. [30] NDUGIRE W, RAVIRANGA NGH, LAO J, et al. Gold Nanoclusters as Nanoantibiotic Auranofin Analogues. Adv Healthc Mater. 2022;11(9): e2101032. [31] HU H, JIANG H, ZHANG K, et al. Memantine nitrate MN-08 suppresses NLRP3 inflammasome activation to protect against sepsis-induced acute lung injury in mice. Biomed Pharmacother. 2022;156:113804. [32] SUBIN P, SABUHOM P, NALADTA A, et al. An Evaluation of the Anti-Inflammatory Effects of a Thai Traditional Polyherbal Recipe TPDM6315 in LPS-Induced RAW264.7 Macrophages and TNF-α-Induced 3T3-L1 Adipocytes. Curr Issues Mol Biol. 2023;45(6):4891-4907. [33] DUNKHUNTHOD B, TALABNIN C, MURPHY M, et al. Gymnema inodorum (Lour.) Decne. Extract Alleviates Oxidative Stress and Inflammatory Mediators Produced by RAW264.7 Macrophages. Oxid Med Cell Longev. 2021;2021:8658314. [34] CUI XY, PARK SH, PARK WH. Auranofin inhibits the proliferation of lung cancer cells via necrosis and caspase‑dependent apoptosis. Oncol Rep. 2020;44(6):2715-2724. [35] HOU GX, LIU PP, ZHANG S, et al. Elimination of stem-like cancer cell side-population by auranofin through modulation of ROS and glycolysis. Cell Death Dis. 2018;9(2):89. [36] HESKETH M, SAHIN KB, WEST ZE, et al. Macrophage Phenotypes Regulate Scar Formation and Chronic Wound Healing. Int J Mol Sci. 2017;18(7):1545. [37] SHARIFIAGHDAM M, SHAABANI E, FARIDI-MAJIDI R, et al. Macrophages as a therapeutic target to promote diabetic wound healing. Mol Ther. 2022;30(9):2891-2908. [38] HAN S, KIM K, KIM H, et al. Auranofin inhibits overproduction of pro-inflammatory cytokines, cyclooxygenase expression and PGE2 production in macrophages. Arch Pharm Res. 2008;31(1):67-74. [39] WANG S, LIU G, LI Y, et al. Metabolic Reprogramming Induces Macrophage Polarization in the Tumor Microenvironment. Front Immunol. 2022;13:840029. [40] RODRÍGUEZ-ENRÍQUEZ S, ROBLEDO-CADENA DX, PACHECO-VELÁZQUEZ SC, et al. Repurposing auranofin and meclofenamic acid as energy-metabolism inhibitors and anti-cancer drugs. PLoS One. 2024;19(9):e0309331. |
| [1] |
Dong Chunyang, Zhou Tianen, Mo Mengxue, Lyu Wenquan, Gao Ming, Zhu Ruikai, Gao Zhiwei.
Action mechanism of metformin combined with Eomecon chionantha Hance dressing in treatment of deep second-degree burn wounds#br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2001-2013.
|
| [2] | Peng Zhiwei, Chen Lei, Tong Lei. Luteolin promotes wound healing in diabetic mice: roles and mechanisms [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1398-1406. |
| [3] | Sun Yajie, Zhao Xinchen, Bo Shuangling. Spatiotemporal expression of bone morphologic protein 7 in mouse kidney development [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1156-1161. |
| [4] | Wen Xiaolong, Weng Xiquan, Feng Yao, Cao Wenyan, Liu Yuqian, Wang Haitao. Effects of inflammation on serum hepcidin and iron metabolism related parameters in patients with type 2 diabetes mellitus: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1294-1301. |
| [5] | Yang Zeyu, Zhi Liang, Wang Jia, Zhang Jingyi, Zhang Qingfang, Wang Yulong, Long Jianjun. A visualized analysis of research hotspots in high-frequency repetitive transcranial magnetic stimulation from the macroscopic perspective [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1320-1330. |
| [6] | Yan Chengbo, Luo Qiuchi, Fan Jiabing, Gu Yeting, Deng Qian, Zhang Junmei. Effect of type 2 diabetes mellitus on orthodontic tooth movement and bone microstructure parameters on the tension side in rats [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 824-831. |
| [7] | Wang Mingqi, Feng Shiya, Han Yinhe, Yu Pengxin, Guo Lina, Jia Zixuan, Wang Xiuli. Construction and evaluation of a neuralized intestinal mucosal tissue engineering model in vitro [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 892-900. |
| [8] | Wang Jie, Huang Rui, Zhang Ye, Shou Zhaoxi, Yao Jie, Liu Chenxi, Liao Jian. Role and mechanism of probiotics in peri-implantitis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 901-907. |
| [9] | Cao Wenqi, Feng Xiuzhi, Zhao Yi, Wang Zhimin, Chen Yiran, Yang Xiao, Ren Yanling. Effect of macrophage polarization on osteogenesis-angiogenesis coupling in type 2 diabetic osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 917-925. |
| [10] | Yang Xiao, Bai Yuehui, Zhao Tiantian, Wang Donghao, Zhao Chen, Yuan Shuo. Cartilage degeneration in temporomandibular joint osteoarthritis: mechanisms and regenerative challenges [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 926-935. |
| [11] | Xu Jiamu, Yang Cheng, Li Weimin, Wang Chunqing. Role and pathogenesis of pyroptosis and inflammatory factors in osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 691-700. |
| [12] | Wang Zhuo, Sun Panpan, Cheng Huanzhi, Cao Tingting. Application of chitosan in repair and regeneration of oral hard and soft tissues [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(2): 459-468. |
| [13] | Liu Xiaohong, Zhao Tian, Mu Yunping, Feng Wenjin, Lyu Cunsheng, Zhang Zhiyong, Zhao Zijian, Li Fanghong. Acellular dermal matrix hydrogel promotes skin wound healing in rats [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(2): 395-403. |
| [14] | Huang Xinxu, Zhang Xin, Wang Jian. Living microecological hydrogels promote skin wound healing [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(2): 489-498. |
| [15] | Zuo Na, Tang Qi, Yu Meng, Tao Kai. Effect of miR-196b-5p in adipose-derived stem cell exosomes on burn wound healing in rats [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(1): 43-49. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||