[1] 张建, 华琦. 中国老龄化的特征发展趋势与对策[J]. 中国心血管杂志,2010,15(1):79-80.
[2] 唐海,罗先正.1043例髋部骨折的病因分析[J] .中华骨科杂志, 1996,16(12):763-765.
[3] OTTO A, BANKE IJ, MEHL J, et al. Retrograde fixation of the lesser trochanter in the adolescent: new surgical technique and clinical results of two cases. Arch Orthop Trauma Surg. 2019;139(4):537-545.
[4] ZHOU JQ, CHANG SM. Failure of PFNA: helical blade perforation and tip-apex distance. Injury. 2012;43(7):1227-1228.
[5] 李双,张世民,张立智,等. 不同组合前内侧皮质支撑复位对股骨转子间骨折髓内钉术后稳定性影响的生物力学研究[J]. 中华创伤骨科杂志,2019,21(1):57-64.
[6] 张世民,余斌. AO/OTA-2018版股骨转子间骨折分类的解读与讨论[J]. 中华创伤骨科杂志,2018,20(7):583-587.
[7] REN H, AO R, WU L, et al. Effect of lesser trochanter posteromedial wall defect on the stability of femoral intertrochanteric fracture using 3D simulation. J Orthop Surg Res. 2020;15(1):242.
[8] 徐锴,李开南.股骨近端内侧壁及其支撑固定的研究进展[J].中华创伤骨科杂志,2018,20(12):1101-1104.
[9] EHRNTHALLER C, OLIVIER AC, GEBHARD F, et al. The role of lesser trochanter fragment in unstable pertrochanteric A2 proximal femur fractures - is refixation of the lesser trochanter worth the effort? Clin Biomech (Bristol, Avon). 2017;42:31-37.
[10] 肖永志,杭志刚,刘艳华. 粗隆间骨折的后内侧骨皮质连续性重建方法及意义[J]. 中国矫形外科杂志,2006,14(20):1589-1591.
[11] 陆伟成,罗振东,张建明,等. 内侧皮质损伤对老年股骨粗隆间骨折术后疗效的影响[J]. 生物骨科材料与临床研究,2016,13(4):78-80.
[12] 路德,吴晓波,解品亮,等.快速康复外科在老年股骨转子间骨折围术期的运用效果[J]. 中华创伤杂志,2018,34(10):939-944.
[13] 宋阳,毕荣修.影像学位置对PFNA手术治疗股骨粗隆间骨折疗效的影响[J].重庆医学,2014,43(7):858-861.
[14] 李双,张立智,张世民. 尖顶距与股距尖顶距的研究进展[J]. 中华创伤骨科杂志,2016,18(8):733-736.
[15] 胡捷斯,杨继梅,鲁晓波,等.股骨头缺血性坏死患者髋关节X线检查相关参数与Harris评分的关系[J].山东医药,2018,58(20):75-77.
[16] 王郑浩,李开南,兰海. 基于三维CT的股骨转子间骨折后内侧壁骨折地图的研究[J]. 中华创伤骨科杂志,2019,21(9):745-751.
[17] CHU X, LIU F, HUANG J, et al. Good short term outcome of arthroplasty with W agner SL implants for unstable intertrochanteric osteoporotic fractures. J Arthroplasty. 2014;29(3):605-608.
[18] 曹培锋,洪勇平.股骨小转子缺损及复位固定的生物力学比较[J].中华矫形外科杂志,2009,17(22):1722-1724.
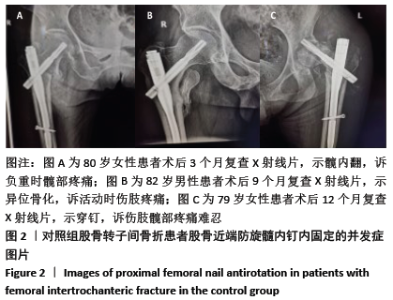
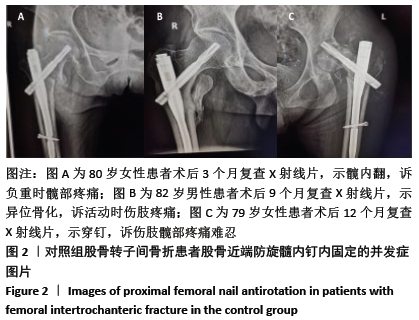
[19] 梁玉柱,王旭明,于小均,等.老年股骨转子间骨折患者新型股骨近端内固定术后并发症原因分析和处理[J]. 中华老年医学杂志, 2018,37(12):1324-1327.
[20] LIU CC, XING WZ, ZHANG YX, et al. Three-dimensional finite element analysis and comparison of a new intramedullary fixation with interlocking intramedullary nail. Cell Biochem Biophys. 2015;71: 717-724.
[21] CHANG SM, ZHANG YQ, MA Z, et al. Fracture reduction with positive medial cortical support: a key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch Orthop Trauma Surg. 2015;135:811-818.
[22] 陈燕才.动力髋螺钉联合钢丝对股骨粗隆见骨折合并内侧壁骨折疗效分析[J].现代诊断与治疗,2017,28(4):607-609.
[23] 何小文,吴子征,张键. 股骨转子间骨折重建股骨距的临床解剖学研究[J]. 中国临床医学,2012,19(4):383-385.
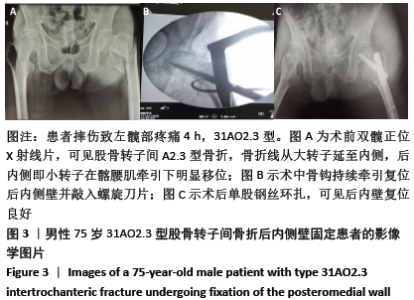
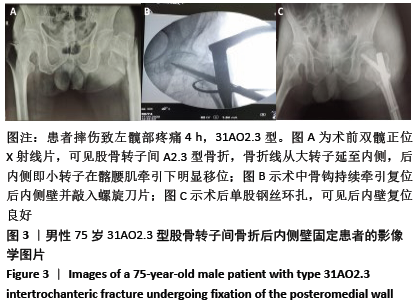
[24] 彭硕,周铁军. 一种治疗股骨转子间骨折合并后内侧壁骨折的新方法[J]. 实用骨科杂志, 2018,24(12):1132-1135.
[25] 杨伟,魏文东,王欢,等.骨钩辅助PFNA治疗不稳定股骨转子间骨折[J]. 重庆医学,2018,47(12):1675-1677.
[26] KIM GM, NAM KW, SEO KB, et al. Wiring technique for lesser trochanter fixation in proximal IM nailing of unstable intertrochanteric fractures: A modified candy-package wiring technique. Injury. 2017;48(2):406-413.
[27] 徐驰,周勇,赵军,等. PFNA治疗老年股骨转子间骨折的隐性失血分析[J]. 中国矫形外科杂志,2018,26(6):510-515.
[28] 杜守超,张世民,张英琪,等.不稳定股骨转子间骨折前内侧皮质支撑复位的影像学研究[J]. 中国矫形外科杂志,2018,26(18):7-12.
[29] 李明,黄迪超,李海洋,等. 骨科机器人导航手术的研究进展[J]. 中华创伤杂志, 2019,35(4):377-384.
[30] 梁玉柱,郭洪刚. 老年骨质疏松性髋部骨折:昨天,今天及未来[J].中国组织工程研究,2017,21(15):2438-2443.
|