Chinese Journal of Tissue Engineering Research ›› 2020, Vol. 24 ›› Issue (15): 2381-2386.doi: 10.3969/j.issn.2095-4344.2603
Previous Articles Next Articles
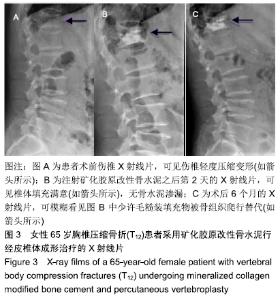
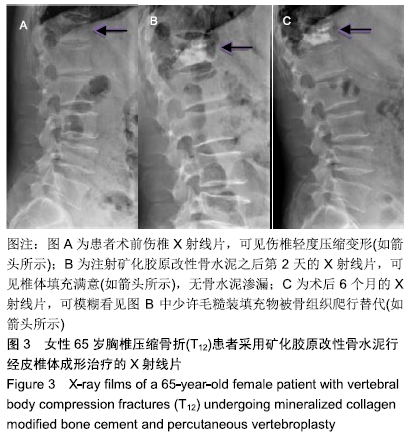
Application of mineralized collagen modified bone cement in the treatment of osteoporotic vertebral compression fractures
Jiang Wenkang1, 2, Geng Wei2, Xu Yingying2, Yang Xiaomei2, Ren Hangling2, Zhang Jingtao2, Ma Jinzhu1, 2
- 1Shandong First Medical University & Shandong Academy of Medical Sciences, Taian 271016, Shandong Province, China; 2Liaocheng People’s Hospital, Liaocheng 252000, Shandong Province, China
-
Received:2019-09-16Revised:2019-09-18Accepted:2019-10-26Online:2020-05-28Published:2020-03-23 -
Contact:Ma Jinzhu, Chief physician, Shandong First Medical University & Shandong Academy of Medical Sciences, Taian 271016, Shandong Province, China; Liaocheng People’s Hospital, Liaocheng 252000, Shandong Province, China -
About author:Jiang Wenkang, Physician, Shandong First Medical University & Shandong Academy of Medical Sciences, Taian 271016, Shandong Province, China; Liaocheng People’s Hospital, Liaocheng 252000, Shandong Province, China -
Supported by:a grant from the Research Center of Medical and Health Science and Technology Development of the Ministry of Health, No. W2012ZT36
CLC Number:
Cite this article
Jiang Wenkang, Geng Wei, Xu Yingying, Yang Xiaomei, Ren Hangling, Zhang Jingtao, Ma Jinzhu. Application of mineralized collagen modified bone cement in the treatment of osteoporotic vertebral compression fractures[J]. Chinese Journal of Tissue Engineering Research, 2020, 24(15): 2381-2386.
share this article
| [1] ZHANG Y, SHI L, TANG P, et al. Comparison of the efficacy between two micro-operative therapies of old patients with osteoporotic vertebral compression fracture: a network meta-analysis. J Cell Biochem. 2017;118(10):3205-3212. [2] TAO CS, QIU ZY, MENG QY, et al. Mineralized collagen incorporated polymethyl methacrylate bone cement for percutaneous vertebroplasty and percutaneous kyphoplasty. J Biomater Tissue Eng. 2014;4(12): 1100-1106. [3] 余伟波,梁德,江晓兵,等.经皮椎体成形术和经皮椎体后凸成形术治疗伴椎体内真空裂隙的骨质疏松椎体压缩骨折比较[J].中国修复重建外科杂志, 2016,30(9):1104-1110. [4] 梁佩清,全昌云,康婷,等.改性PMMA骨水泥的临床研究进展[J].功能材料, 2017,48(2):2048-2054. [5] JIANG HJ, XU J, QIU ZY, et al. Mechanical properties and cytocompatibility improvement of vertebroplasty PMMA bone cements by incorporating mineralized collagen. Materials. 2015;8:2616-2634. [6] LIAO SS, GUAN K, CUI FZ, et al. Lumbar spinal fusion with a mineralized collagen matrix and rhBMP-2 in a rabbit model. Spine. 2003;28:1954-1960. [7] LIAO SS, CUI FZ, ZHANG W, et al. Hierarchically biomimetic bone scaffold materials: nano-HA/collagen/PLA composite. J Biomed Mater Res B Appl Biomater. 2004;69:158-165. [8] KOU JM, FU TY, JIA XJ, et al. Clinical observations on repair of noninfected bone nonunion by using mineralized collagen graft. J Biomater Tissue Eng. 2014;4:1107-1112. [9] QIU Z, ZHANG Y, ZHANG Z, et al. Biodegradable mineralized collagen plug for the reconstruction of craniotomy burr-holes:a report of three cases. Transl Neurosci Clin. 2015;1:3-9. [10] FENG L, ZHANG L, CUI Y, et al. Clinical evaluations of mineralized collagen in the extraction sites preservation. Regen Biomater. 2016; 3:41-48. [11] ZHOU T, LIN H, WANG H, et al. Comparative study on the biomechanics between improved PVP and traditional PKP in the treatment of vertebral peripheral wall damage-type OVCF. Exp Ther Med. 2017;14(1):575-580. [12] DU JP, LIU JJ, FAN Y, et al. Surgery for multisegment thoracolumbar mild osteoporotic fractures: revised assessment system of thoracolumbar osteoporotic fracture. World Neurosurgery. 2018;114: e969-e975. [13] 李昂,李坚.骨质疏松椎体压缩性骨折的微创治疗进展[J]. 中国社区医师, 2017,33(34):20-22. [14] 吴晶晶. 矿化胶原改性PMMA骨水泥研究[D].北京:中国地质大学,2016. [15] KUHN KD, HONTZSCH D. Augmentation with PMMA cement. Der Unfallchirurg. 2015;118(9):737-748. [16] SUGINO A, MIYAZAKI T, KAWACHI G, et al. Relationship between apatite-forming ability and mechanical properties of bioactive PMMA-based bone cement modified with calcium salts and alkoxysilane. J Mater Sci Mater Med. 2008;19(3):1399-1405. [17] WU J, XU S, QIU Z, et al. Comparison of human mesenchymal stem cells proliferation and differentiation on poly(methyl methacrylate) bone cements with and without mineralized collagen incorporation. J Biomater Appl. 2016;30(6):722-731. [18] LI T, WENG X, BIAN Y, et al. Influence of nano-ha coated bone collagen to acrylic (polymethylmethacrylate) bone cement on mechanical properties and bioactivity. PLoS One. 2015;10(6): e0129018. [19] WANG X, KOU JM, YUE Y, et al. Clinical outcome comparison of polymethylmethacrylate bone cement with and without mineralized collagen modification for osteoporotic vertebral compression fractures. Medicine. 2018;97(37):e12204. [20] ANDREI D, POPA I, BRAD S, et al. The variability of vertebral body volume and pain associated with osteoporotic vertebral fractures: conservative treatment versus percutaneous transpedicular vertebroplasty. Int Orthop. 2017;41(5):963-968. [21] CHEN C, LI DW, WANG Q, et al. The cost effectiveness analysis of minimally invasive surgery and conservative treatment in elderly osteoporotic spinal fracture. Zhongguo Gu Shang. 2016;29(7):614-618. [22] LI YX, GUO DQ, ZHANG SC, et al. Risk factor analysis for re-collapse of cemented vertebrae after percutaneous vertebroplasty (PVP) or percutaneous kyphoplasty (PKP). Int Orthop. 2018;42(9):2131-2139. [23] WANG H, SRIBASTAV SS, YE F, et al. Comparison of percutaneous vertebroplasty and balloon kyphoplasty for the treatment of single level vertebral compression fractures: a meta-analysis of the literature. Pain Physician. 2015;18(3):209-222. [24] YANG EZ, XU JG, HUANG GZ, et al. Percutaneous vertebroplasty versus conservative treatment in aged patients with acute osteoporotic vertebral compression fractures: a prospective randomized controlled clinical study. Spine (Phila Pa 1976). 2016;41(8):653-660. [25] YANG J, ZHANG K, ZHANG S, et al. Preparation of calcium phosphate cement and polymethyl methacrylate for biological composite bone cements. Med Sci Monit. 2015;21:1162-1172. [26] 邱贵兴,裴福兴,胡侦明,等. 中国骨质疏松性骨折诊疗指南——骨质疏松性骨折诊断及治疗原则[J]. 黑龙江科学, 2018,9(2):85-88+95. [27] 宋天喜,胡艳丽,崔云,等. 仿生矿化胶原人工骨在兔脊柱后外侧融合中的应用研究[J]. 中国修复重建外科杂志, 2018,32(9):1137-1143. [28] TODTMANN N, LODE A, MANN R, et al. Influence of different modifications of a calcium phosphate cement on resorption and new bone formation: an in vivo study in the minipig. J Biomed Mater Res B Appl Biomater. 2013;101(8):1410-1418. [29] ZHU J, ZHANG K, LUO K, et al. Mineralized collagen modified polymethyl methacrylate bone cement for osteoporotic compression vertebral fracture at 1-year follow-up. Spine. 2019;44(12):827-838. [30] EPSTEIN NE. A comparison of kyphoplasty, vertebroplasty, or non-surgical treatment of traumatic/atraumatic osteoporotic vertebral compression fractures: a short review. Surg Neurol Int. 2019;10:54. |
| [1] | Tang Hui, Yao Zhihao, Luo Daowen, Peng Shuanglin, Yang Shuanglin, Wang Lang, Xiao Jingang. High fat and high sugar diet combined with streptozotocin to establish a rat model of type 2 diabetic osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1207-1211. |
| [2] | Li Zhongfeng, Chen Minghai, Fan Yinuo, Wei Qiushi, He Wei, Chen Zhenqiu. Mechanism of Yougui Yin for steroid-induced femoral head necrosis based on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1256-1263. |
| [3] | Hou Guangyuan, Zhang Jixue, Zhang Zhijun, Meng Xianghui, Duan Wen, Gao Weilu. Bone cement pedicle screw fixation and fusion in the treatment of degenerative spinal disease with osteoporosis: one-year follow-up [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 878-883. |
| [4] | Li Shibin, Lai Yu, Zhou Yi, Liao Jianzhao, Zhang Xiaoyun, Zhang Xuan. Pathogenesis of hormonal osteonecrosis of the femoral head and the target effect of related signaling pathways [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 935-941. |
| [5] | Xiao Fangjun, Chen Shudong, Luan Jiyao, Hou Yu, He Kun, Lin Dingkun. An insight into the mechanism of Salvia miltiorrhiza intervention on osteoporosis based on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 772-778. |
| [6] | Liu Bo, Chen Xianghe, Yang Kang, Yu Huilin, Lu Pengcheng. Mechanism of DNA methylation in exercise intervention for osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 791-797. |
| [7] | Zhong Yuanming, Wan Tong, Zhong Xifeng, Wu Zhuotan, He Bingkun, Wu Sixian. Meta-analysis of the efficacy and safety of percutaneous curved vertebroplasty and unilateral pedicle approach percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 456-462. |
| [8] | Nie Shaobo, Li Jiantao, Sun Jien, Zhao Zhe, Zhao Yanpeng, Zhang Licheng, Tang Peifu. Mechanical stability of medial support nail in treatment of severe osteoporotic intertrochanteric fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 329-333. |
| [9] | Zhu Yun, Chen Yu, Qiu Hao, Liu Dun, Jin Guorong, Chen Shimou, Weng Zheng. Finite element analysis for treatment of osteoporotic femoral fracture with far cortical locking screw [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3832-3837. |
| [10] | Feng Guancheng, Fang Jianming, Lü Haoran, Zhang Dongsheng, Wei Jiadong, Yu Bingbing. How does bone cement dispersion affect the early outcome of percutaneous vertebroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3450-3457. |
| [11] | Chen Lei, Zheng Rui, Jie Yongsheng, Qi Hui, Sun Lei, Shu Xiong. In vitro evaluation of adipose-derived stromal vascular fraction combined with osteochondral integrated scaffold [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3487-3492. |
| [12] | Liu Chang, Li Datong, Liu Yuan, Kong Lingbo, Guo Rui, Yang Lixue, Hao Dingjun, He Baorong. Poor efficacy after vertebral augmentation surgery of acute symptomatic thoracolumbar osteoporotic compression fracture: relationship with bone cement, bone mineral density, and adjacent fractures [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3510-3516. |
| [13] | Cai Qunbin, Yang Lijuan, Li Qiumin, Chen Xinmin, Zheng Liqin, Huang Peizhen, Lin Ziling, Jiang Ziwei . Feasibility of internal fixation removal of intertrochanteric fractures in elderly patients based on fracture mechanics [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3313-3318. |
| [14] | Liu Yulin, Li Guotai. Combined effects of hyperbaric oxygen, vibration training and astaxanthin on bone mineral density, glucose metabolism and oxidative stress in diabetic osteoporosis rats [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(20): 3117-3124. |
| [15] | Lin Haishan, Mieralimu Muertizha, Li Peng, Ma Chao, Wang Li. Correlation between skeletal muscle fiber characteristics and bone mineral density in postmenopausal women with hip fractures [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(20): 3144-3149. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||