Chinese Journal of Tissue Engineering Research ›› 2019, Vol. 23 ›› Issue (32): 5240-5248.doi: 10.3969/j.issn.2095-4344.1476
Different interventions and implants for the functional recovery and complications of displaced midshaft clavicular fractures: a network meta-analysis
Chen Zhe1, Shi Qingyang1, Gao Zhuo1, Peng Yingying1, Wang Yongqing2
- 1Tianjin University of Traditional Chinese Medicine, Tianjin 301600, China; 2Tianjin 4th Centre Hospital, Tianjin 300140, China
-
Online:2019-11-18Published:2019-11-18 -
Contact:Wang Yongqing, Chief physician, Professor, Doctoral supervisor, Tianjin 4th Centre Hospital, Tianjin 300140, China -
About author:Chen Zhe, Master candidate, Tianjin University of Traditional Chinese Medicine, Tianjin 301600, China -
Supported by:the Key Research Project of Tianjin Health Industry, No. 15KG122 (to WYQ)
CLC Number:
Cite this article
Chen Zhe, Shi Qingyang, Gao Zhuo, Peng Yingying, Wang Yongqing. Different interventions and implants for the functional recovery and complications of displaced midshaft clavicular fractures: a network meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2019, 23(32): 5240-5248.
share this article

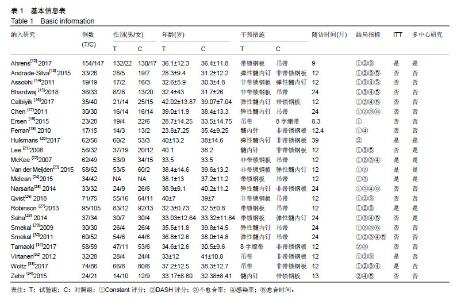
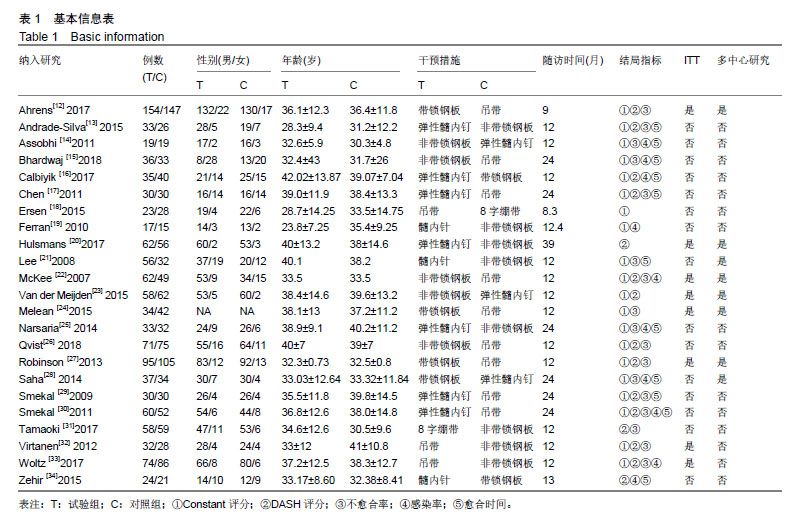
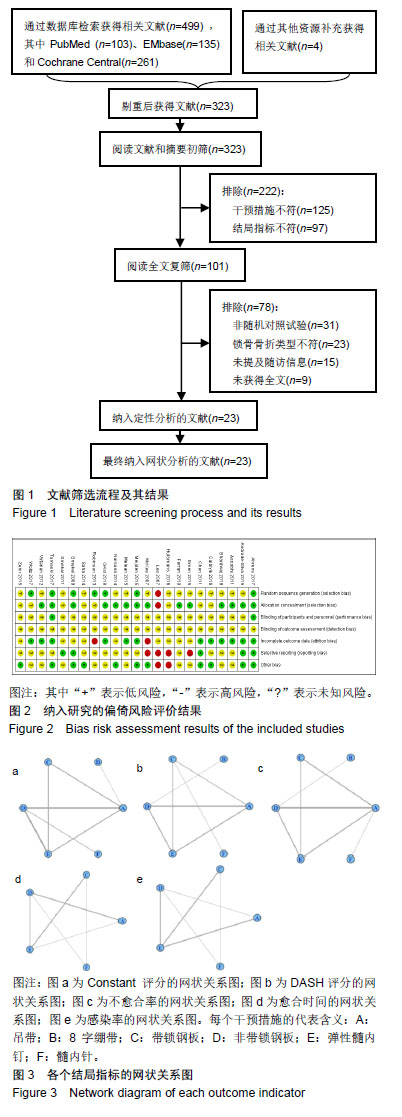
2.1 文献筛选流程及结果 初检得到文献503篇,经过层层筛查,最终纳入23个随机对照试验[12-34],均为英文文献,共2 234例患者。文献筛选流程及结果见图1。 2.2 纳入研究的基本特征 纳入研究的基本特征见表1。 2.3 纳入研究的偏倚风险评价结果 纳入研究的偏倚风险评价结果见图2。 2.4 结局指标的网络关系图 各个结局指标的干预措施网络关系图见图3,图中各顶点代表各干预措施,线条代表两两比较是否发生,其中带箭头的实线代表含基本参数的直接比较,虚线代表不带参数的直接比较,未连接的干预之间代表仅为间接比较。本研究所涉及的干预措施一共是6种,分别是非手术治疗,包括2种治疗方法(吊带、8字绷带);手术治疗,包括4种治疗方法(锁定钢板、非锁定钢板、弹性髓内钉以及髓内针)。各个结局指标的网状关系图:Constant 评分的网状关系图(图3 a);DASH评分的网状关系图(图3b);不愈合率的网状关系图(图3c);骨折愈合时间的网状关系图(图3d);感染率的网状关系图(图3e)。"

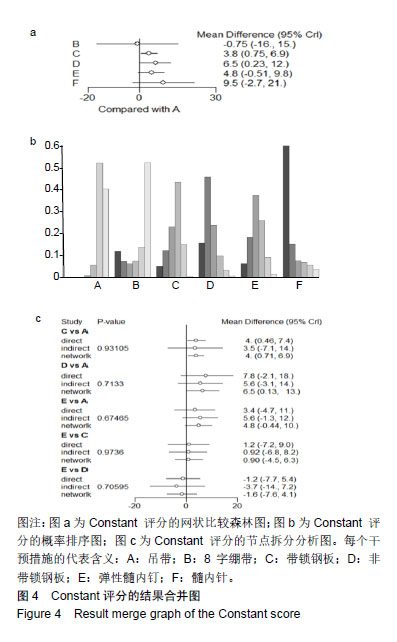
2.5 网状Meta分析结果 2.5.1 Constant 评分 Constant评分的网状比较结果:各干预措施与吊带相比的结果显示,8字绷带的Constant 评分结果无统计学差异[MD=-0.75,95%Cr(-16,15)];锁定钢板Constant 评分结果有统计学差异[MD=3.8,95%Cr(0.75,6.9)];非锁定钢板的Constant 评分结果有统计学差异[MD=6.5,95%Cr(0.23,12)];弹性髓内钉Constant 评分结果无统计学差异[MD=4.8,95%Cr(-0.51,9.8)];髓内针的Constant 评分结果无统计学差异[MD=9.5,95%Cr(-2.7,21)],见图4a。 网状分析结果显示,锁定钢板的Constant评分优于吊带,差异具有统计学意义[MD=3.845,95%Cr(0.747,6.887)];非锁定钢板的Constant评分优于吊带,差异具有统计学意义[MD=6.451,95%Cr(0.231,12.397)]。其余治疗方法Constant评分的比较结果都没有统计学差异,见表2右上。 Constant评分的概率排序:通过对排序图中的柱状图进行评估分析,将所涉及的干预措施进行概率排序,结果显示:按照优劣顺序为髓内针、非锁定钢板、弹性髓内钉、锁定钢板、吊带、8字绷带,见图4b。 Constant评分的节点拆分分析:通过节点拆分来评价锁骨中段移位性骨折的Constant评分不一致性,当P < 0.05时,说明各研究直接与间接比较结果间不一致。结果显示:当锁定钢板对比吊带时,P=0.931 05;当非锁定钢板对比吊带时,P=0.713 3;当弹性髓内钉对比吊带时,P=0.674 65;当弹性髓内钉对比锁定钢板时,P=0.973 6;当弹性髓内钉比较非锁定钢板时,P=0.705 95,见图4c。"

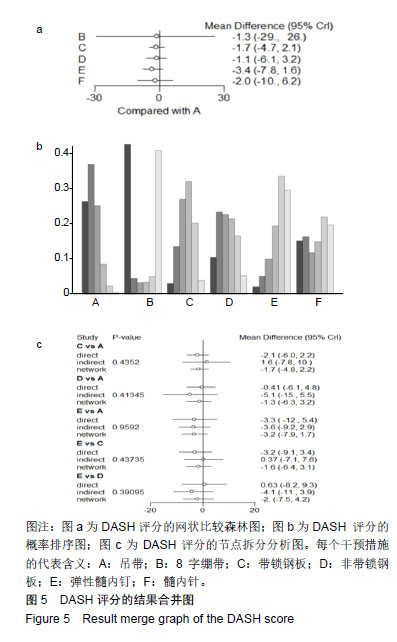
2.5.2 DASH评分 DASH评分的网状比较结果森林图:各干预措施与吊带相比的结果显示,8字绷带的DASH评分结果无统计学差异[MD=-1.3,95%Cr(-29,26)];锁定钢板的DASH评分结果无统计学差异[MD=-1.7,95%Cr(-4.7,2.1)];非锁定钢板的DASH评分结果无统计学差异[MD=-1.1,95%Cr(-6.1,3.2)];弹性髓内钉的DASH评分结果无统计学差异[MD=-3.4,95%Cr(-7.8,1.6)];髓内针的DASH评分结果无统计学差异[MD=-2.0,95%Cr(-10,6.2)],见图5a。 网状分析结果显示,不同干预措施治疗锁骨中段移位性骨折的DASH评分的两两比较结果显示,都没有统计学差异,见表2左下。 DASH评分的概率排序:通过对排序图中的柱状图进行评估分析,将所涉及的干预措施进行概率排序。由于8字绷带的95%Cr区间过大,导致其标准差较均数过大,因此8字绷带组无法进行DASH评分的排序。其余结果显示:优劣顺序为弹性髓内钉、髓内针、锁定钢板、吊带、非锁定钢板,见图5b。 DASH评分的节点拆分分析:通过节点拆分来评价锁骨中段移位性骨折的DASH评分不一致性,当P < 0.05时,说明各研究直接与间接比较结果间不一致。当锁定钢板对比吊带时,P=0.435 2;当非锁定钢板对比吊带时,P=0.413 45;当弹性髓内钉对比吊带时,P=0.959 2;当弹性髓内钉对比锁定钢板时,P=0.437 35;当弹性髓内钉对比非锁定钢板时,P=0.390 95,见图5c。"

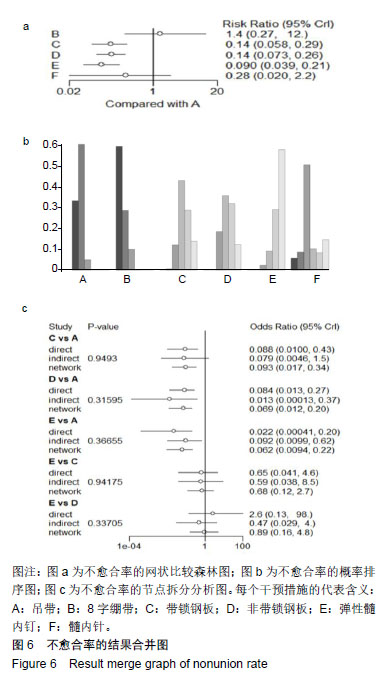
2.5.3 不愈合率 不愈合率的网状比较结果:各干预措施与吊带相比的结果显示,8字绷带的不愈合率结果无统计学差异[RR=1.4,95%Cr(0.27,12)];锁定钢板的不愈合率结果有统计学差异[RR=0.14,95%Cr(0.058,0.29)];非锁定钢板的不愈合率结果有统计学差异[RR=0.14,95%Cr(0.073,0.26)];弹性髓内钉的不愈合率结果有统计学差异[RR=0.090,95%Cr(0.039,0.21)];髓内针的不愈合率结果无统计学差异[RR=0.28,95%Cr(0.02,2.2)],见图6a。 网状分析结果显示,锁定钢板的不愈合率要优于吊带,差异具有统计学意义[logRR=1.958,95%Cr(1.248,2.845)];非锁定钢板的不愈合率要优于吊带,差异具有统计学意义[logRR=1.952,95%Cr(1.335,2.616)];弹性髓内钉的不愈合率要优于吊带,差异具有统计学意义[logRR=2.404,95%Cr(1.574,3.239)];锁定钢板的不愈合率要优于8字绷带,差异具有统计学意义[logRR=2.321,95%Cr(0.432,4.453)];非锁定钢板的不愈合率要优于8字绷带,差异具有统计学意义[logRR=2.294,95%Cr(0.727,4.27)];弹性髓内钉的不愈合率要优于8字绷带,差异具有统计学意义[logRR=2.803,95%Cr(0.821,4.816)]。其余治疗方法不愈合率的比较结果都没有统计学差异,见表3左下。 不愈合率的概率排序:通过对排序图中的柱状图进行评估分析,将所涉及的干预措施进行概率排序,结果显示:优劣顺序为弹性髓内钉、非锁定钢板、锁定钢板、髓内针、吊带、8字绷带,见图6b。 不愈合率的节点拆分分析:通过节点拆分来评价锁骨中段移位性骨折的不愈合率不一致性,当P < 0.05时,说明各研究直接与间接比较结果间不一致。当锁定钢板对比吊带时,P=0.949 3;当非锁定钢板对比吊带时,P=0.315 95;当弹性髓内钉对比吊带时,P=0.366 55;当弹性髓内钉对比锁定钢板时,P=0.941 75;当弹性髓内钉对比非锁定钢板时,P=0.337 05,见图6c。"

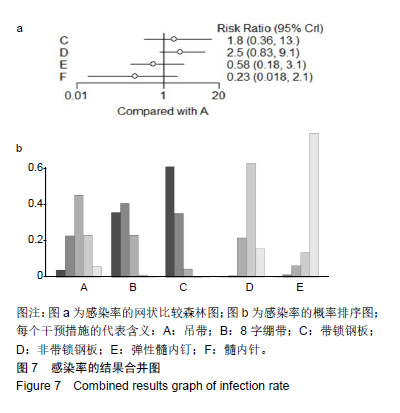
2.5.4 感染率 感染率的网状比较结果:各干预措施与吊带相比的结果显示,锁定钢板所发生的感染率无统计学差异[RR=1.8,95%Cr(0.36,13)];非锁定钢板所发生的感染率无统计学差异[RR= 2.5,95%Cr(0.83,9.1)];弹性髓内钉所发生的感染率无统计学差异[RR=0.58,95%Cr(0.18,3.1)];髓内针所发生的感染率无统计学差异[RR=0.23,95%Cr (0.018,2.1)],见图7a。 网状分析结果显示,弹性髓内钉的感染率要优于锁定钢板,差异具有统计学意义[logRR=-1.109,95%Cr(-2.267,-0.203)];弹性髓内钉的感染率要优于非锁定钢板,差异具有统计学意义[logRR=-1.371,95%Cr(-2.497,-0.24)];髓内针的感染率要优于锁定钢板,差异具有统计学意义[logRR=-2.116,95%Cr(-4.163,-0.121)];髓内钉的感染率要优于非锁定钢板,差异具有统计学意义[logRR=-2.269,95%Cr(-4.657,-0.739)]。其余治疗方法感染率的比较结果都没有统计学差异,见表3右上。 感染率的概率排序:通过对排序图中的柱状图进行评估分析,将所涉及的干预措施进行概率排序,结果显示:优劣顺序为髓内针、弹性髓内钉、锁定钢板、非锁定钢板、吊带,见图7b。"

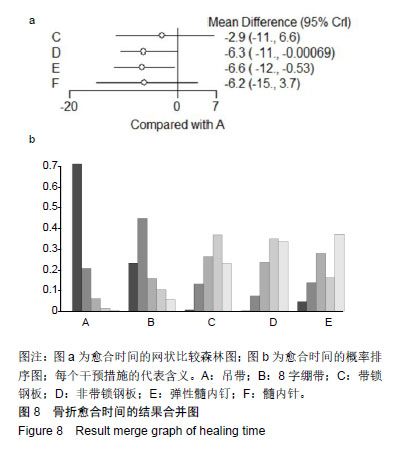
2.5.5 骨折愈合时间 骨折愈合时间的网状比较结果:各干预措施与吊带相比的结果显示,锁定钢板的愈合时间无统计学差异[MD=-2.9,95%Cr(-11,6.6)];非锁定钢板的愈合时间有统计学差异[MD=-6.3,95%Cr(-11,-0.000 69)];弹性髓内钉的愈合时间有统计学差异[MD=-6.6,95%Cr(-12,-0.53)];髓内针的愈合时间无统计学差异[MD=-6.2,95%Cr(-15,3.7)],见图8a。 骨折愈合时间的概率排序:通过对排序图中的柱状图进行评估分析,将所涉及的干预措施进行概率排序,结果显示:优劣顺序为髓内针、非锁定钢板、弹性髓内钉、锁定钢板、吊带,见图8b。"
| [1] Burnham JM, Kim DC, Kamineni S. Midshaft Clavicle Fractures: A Critical Review. Orthopedics. 2016;39(5):e814-e821. [2] Pang EQ, Zhang S, Harris A, et al. Treatment Trends in Older Adults With Midshaft Clavicle Fractures. J Hand Surg Am. 2017;42(11):875-882. [3] van der Meijden OA, Gaskill TR, Millett PJ. Treatment of clavicle fractures: current concepts review. J Shoulder Elbow Surg. 2012;21(3): 423-429. [4] Bravman JT, Vidal AF. Midshaft clavicle fractures: are surgical indications changing?. Orthopedics. 2009;32(12):909-913. [5] Hoogervorst P, Appalsamy A, Meijer D, et al. Does altering projection of the fractured clavicle change treatment strategy?. J Shoulder Elbow Surg. 2019;28(3):e65-e70. [6] Wang XH, Guo WJ, Li AB, et al. Operative versus nonoperative treatment for displaced midshaft clavicle fractures: a meta-analysis based on current evidence. Clinics (Sao Paulo). 2015;70(8):584-592. [7] Ahmed AF, Salameh M, AlKhatib N, et al. Open Reduction and Internal Fixation Versus Nonsurgical Treatment in Displaced Midshaft Clavicle Fractures: A Meta-Analysis. J Orthop Trauma. 2018;32(7):e276-e283. [8] Rehn CH, Kirkegaard M, Viberg B, et al. Operative versus nonoperative treatment of displaced midshaft clavicle fractures in adults: a systematic review. Eur J Orthop Surg Traumatol. 2014;24(7):1047-1053. [9] Woltz S, Krijnen P, Schipper IB. Plate Fixation Versus Nonoperative Treatment for Displaced Midshaft Clavicular Fractures: A Meta-Analysis of Randomized Controlled Trials. J Bone Joint Surg Am. 2017;99(12): 1051-1057. [10] Liu J, Srivastava K, Washington T, et al. Cost-Effectiveness of Operative Versus Nonoperative Treatment of Displaced Midshaft Clavicle Fractures: A Decision Analysis. J Bone Joint Surg Am. 2019;101(1):35-47. [11] Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions (Version 5. 1. 0). Available at: http://handbook.cochrane.org. [12] Ahrens PM, Garlick NI, Barber J, et al. The Clavicle Trial: A Multicenter Randomized Controlled Trial Comparing Operative with Nonoperative Treatment of Displaced Midshaft Clavicle Fractures. J Bone Joint Surg Am. 2017;99(16):1345-1354. [13] Andrade-Silva FB, Kojima KE, Joeris A, et al. Single, superiorly placed reconstruction plate compared with flexible intramedullary nailing for midshaft clavicular fractures: a prospective, randomized controlled trial. J Bone Joint Surg Am. 2015;97(8):620-626. [14] Assobhi JE. Reconstruction plate versus minimal invasive retrograde titanium elastic nail fixation for displaced midclavicular fractures. J Orthop Traumatol. 2011;12(4):185-192. [15] Bhardwaj A, Sharma G, Patil A, et al. Comparison of plate osteosynthesis versus non-operative management for mid-shaft clavicle fractures-A prospective study. Injury. 2018;49(6):1104-1107. [16] Calbiyik M, Ipek D, Taskoparan M. Prospective randomized study comparing results of fixation for clavicular shaft fractures with intramedullary nail or locking compression plate. Int Orthop. 2017;41(1): 173-179. [17] Chen QY, Kou DQ, Cheng XJ, et al. Intramedullary nailing of clavicular midshaft fractures in adults using titanium elastic nail. Chin J Traumatol. 2011;14(5):269-276. [18] Ersen A, Atalar AC, Birisik F, et al. Comparison of simple arm sling and figure of eight clavicular bandage for midshaft clavicular fractures: a randomised controlled study. Bone Joint J. 2015;97-B(11):1562-1565. [19] Ferran NA, Hodgson P, Vannet N, et al. Locked intramedullary fixation vs plating for displaced and shortened mid-shaft clavicle fractures: a randomized clinical trial. J Shoulder Elbow Surg. 2010;19(6):783-789. [20] Hulsmans MH, van Heijl M, Houwert RM, et al. High Irritation and Removal Rates After Plate or Nail Fixation in Patients With Displaced Midshaft Clavicle Fractures. Clin Orthop Relat Res. 2017;475(2): 532-539. [21] Lee YS, Huang HL, Lo TY, et al. Surgical treatment of midclavicular fractures: a prospective comparison of Knowles pinning and plate fixation. Int Orthop.2008;32(4):541-545. [22] Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89(1): 1-10. [23] van der Meijden OA, Houwert RM, Hulsmans M, et al. Operative treatment of dislocated midshaft clavicular fractures: plate or intramedullary nail fixation? A randomized controlled trial. J Bone Joint Surg Am. 2015;97(8):613-619. [24] Melean PA, Zuniga A, Marsalli M, et al. Surgical treatment of displaced middle-third clavicular fractures: a prospective, randomized trial in a working compensation population. J Shoulder Elbow Surg. 2015;24(4): 587-592. [25] Narsaria N, Singh AK, Arun GR, et al. Surgical fixation of displaced midshaft clavicle fractures: elastic intramedullary nailing versus precontoured plating. J Orthop Traumatol. 2014;15(3):165-171. [26] Qvist AH, Vaesel MT, Jensen CM, et al. Plate fixation compared with nonoperative treatment of displaced midshaft clavicular fractures: a randomized clinical trial. Bone Joint J. 2018;100-B(10):1385-1391. [27] Robinson CM, Goudie EB, Murray IR, et al. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: a multicenter, randomized, controlled trial. J Bone Joint Surg Am. 2013;95(17):1576-1584. [28] Saha P, Datta P, Ayan S, et al. Plate versus titanium elastic nail in treatment of displaced midshaft clavicle fractures: A comparative study. Indian J Orthop.2014;48(6):587-593. [29] Smekal V, Irenberger A, Struve P, et al. Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures-a randomized, controlled, clinical trial. J Orthop Trauma. 2009; 23(2):106-112. [30] Smekal V, Irenberger A, Attal RE, et al. Elastic stable intramedullary nailing is best for mid-shaft clavicular fractures without comminution: results in 60 patients. Injury.2011;42(4):324-329. [31] Tamaoki M, Matsunaga FT, Costa A, et al. Treatment of Displaced Midshaft Clavicle Fractures: Figure-of-Eight Harness Versus Anterior Plate Osteosynthesis: A Randomized Controlled Trial. J Bone Joint Surg Am. 2017;99(14):1159-1165. [32] Virtanen KJ, Remes V, Pajarinen J, et al. Sling compared with plate osteosynthesis for treatment of displaced midshaft clavicular fractures: a randomized clinical trial. J Bone Joint Surg Am. 2012;94(17):1546-1553. [33] Woltz S, Stegeman SA, Krijnen P, et al. Plate Fixation Compared with Nonoperative Treatment for Displaced Midshaft Clavicular Fractures: A Multicenter Randomized Controlled Trial. J Bone Joint Surg Am. 2017; 99(2):106-112. [34] Zehir S, Zehir R, Sahin E, et al. Comparison of novel intramedullary nailing with mini-invasive plating in surgical fixation of displaced midshaft clavicle fractures. Arch Orthop Trauma Surg. 2015;135(3):339-344. [35] George DM, McKay BP, Jaarsma RL. The long-term outcome of displaced mid-third clavicle fractures on scapular and shoulder function: variations between immediate surgery, delayed surgery, and nonsurgical management. J Shoulder Elbow Surg.2015;24(5):669-676. [36] Rosa N, Marta M, Vaz M, et al. Recent developments on intramedullary nailing: a biomechanical perspective. Ann N Y Acad Sci. 2017;1408(1): 20-31. [37] Naveen BM, Joshi GR, Harikrishnan B. Management of mid-shaft clavicular fractures: comparison between non-operative treatment and plate fixation in 60 patients. Strategies Trauma Limb Reconstr. 2017; 12(1):11-18. [38] Ozkul B, Saygili MS, Dincel YM, et al. Comparative Results of External Fixation, Plating, or Nonoperative Management for Diaphyseal Clavicle Fractures. Med Princ Pract. 2017;26(5):458-463. [39] McKee MD, Pedersen EM, Jones C, et al. Deficits following nonoperative treatment of displaced midshaft clavicular fractures. J Bone Joint Surg Am. 2006;88(1):35-40. [40] van der Linde RA, Beetz I, van Helden SH. Plating for midshaft clavicular fractures: The impact on quality of life and functional outcome. Injury. 2017;48(12):2778-2783. [41] Mirzatolooei F. Comparison between operative and nonoperative treatment methods in the management of comminuted fractures of the clavicle. Acta Orthop Traumatol Turc. 2011;45(1):34-40. [42] Gausden EB, Villa J, Warner SJ, et al. Nonunion After Clavicle Osteosynthesis: High Incidence of Propionibacterium acnes. J Orthop Trauma. 2017;31(4):229-235. [43] Chen YF, Wei HF, Zhang C, et al. Retrospective comparison of titanium elastic nail (TEN) and reconstruction plate repair of displaced midshaft clavicular fractures. J Shoulder Elbow Surg. 2012;21(4):495-501. [44] Hussain N, Sermer C, Prusick PJ, et al. Intramedullary Nailing Versus Plate Fixation for the Treatment Displaced Midshaft Clavicular Fractures: A Systematic Review and Meta-Analysis. Sci Rep. 2016;6:34912. [45] Calbiyik M, Zehir S, Ipek D. Minimally invasive implantation of a novel flexible intramedullary nail in patients with displaced midshaft clavicle fractures. Eur J Trauma Emerg Surg. 2016;42(6):711-717. [46] Wang J, Meng XH, Guo ZM, et al. Interventions for treating displaced midshaft clavicular fractures: a Bayesian network meta-analysis of randomized controlled trials. Medicine (Baltimore). 2015;94(11):e595. [47] Turner T, Green S, Tovey D, et al. Producing Cochrane systematic reviews-a qualitative study of current approaches and opportunities for innovation and improvement. Syst Rev. 2017;6(1):147. |
| [1] | Zhou Jihui, Li Xinzhi, Zhou You, Huang Wei, Chen Wenyao. Multiple problems in the selection of implants for patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1440-1445. |
| [2] | Zhan Fangbiao, Cheng Jun, Zou Xinsen, Long Jie, Xie Lizhong, Deng Qianrong. Intraoperative intravenous application of tranexamic acid reduces perioperative bleeding in multilevel posterior spinal surgery: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 977-984. |
| [3] | Xiang Feifan, Ye Junwu, Zhang Xihai, Ge Jianhua, Tang Lian, Yang Yunkang. Comparison of three different internal fixation methods in treatment of ipsilateral femoral neck and shaft fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 403-408. |
| [4] | Li Yanle, Yue Xiaohua, Wang Pei, Nie Weizhi, Zhang Junwei, Tan Yonghai, Jiang Hongjiang. Intramedullary nail fixation versus plate fixation in the treatment of displaced midshaft clavicular fractures in adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 471-476. |
| [5] | Zhang Degang, Liu Dong, Li Peng, Wang Zhaolin, Zhang Kai, Zhang Xinjun. Short-term follow-up of elastic intramedullary nail and plate in the treatment of displaced middle clavicle type B fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3860-3864. |
| [6] | Yang Wei, Chen Zehua, Yi Zhiyong, Huang Xudong, Han Qingmin, Zhang Ronghua. Effectiveness of intra-articular injection of hyaluronic acid versus placebo in the treatment of early and mid-stage knee osteoarthritis: a Meta-analysis based on randomized, double-blind, controlled, clinical trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(23): 3760-3766. |
| [7] | Xu Weilong, Zuo Yuan, Xin Daqi, He Chenyang, Zhao Peng, Shi Ming, Zhou Boyuan, Liu Yating, Zhao Yan. Selection of modeling methods for acute compressive spinal cord injury: a network Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(23): 3767-3772. |
| [8] | Fu Panfeng, Shang Wei, Kang Zhe, Deng Yu, Zhu Shaobo. Efficacy of anterolateral minimally invasive approach versus traditional posterolateral approach in total hip arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3409-3415. |
| [9] | Ren Xingyu, Zhang Yi, Xu Haoran, Fan Bin, Dai Shifeng, Liang Chunyu. Meta-analysis of the postoperative effects of robot-assisted unicompartmental knee arthroplasty versus conventional surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3416-3422. |
| [10] | Wang Yanjiao, Wang Rui, Sun Luning. Bankart pepair versus Bristow-Latarjet procedure for recurrent anterior instability of the shoulder: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3423-3430. |
| [11] | Xu Hui, Kang Bingxin, Zhong Sheng, Gao Chenxin, Zhao Chi, Qiu Guowei, Sun Songtao, Xie Jun, Xiao Lianbo, Shi Qi. Pressing local acupoints plus adjustion of the knee joint in a sitting position for treating knee osteoarthritis: a randomized controlled trial [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(2): 216-221. |
| [12] | Xia Wenshen, He Renjiao, Ai Jinwei, Wang Jun, Li Desheng, Pei Bin. Stem cell transplantation for diabetic patients with lower-extremity arterial disease: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 3110-3116. |
| [13] | Li Haifeng, Liu Yu, Yin Qudong, Sun Zhenzhong, Rui Yongjun, Gu Sanjun. Risk of complications of early postoperative weight-bearing after internal fixation of intracapsular femoral neck fractures: 2-year follow-up [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2875-2880. |
| [14] | Yuan Jiaqin, Luan Fujun, Chen Yangfan, Deng Yi, Li Bo. Meta-analysis of bipolar and unipolar hemiarthroplasties for displaced femoral neck fracture in the elderly patients [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2915-2922. |
| [15] | Zhong Yuanming, Fu Xiaopeng, Xu Wei, Zhao Qingrui, Huang Yong, Ye Weiquan. Nicardipine controlled hypotension applied to perioperative blood loss in orthopedics: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2930-2937. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||