Chinese Journal of Tissue Engineering Research ›› 2018, Vol. 22 ›› Issue (23): 3730-3735.doi: 10.3969/j.issn.2095-4344.0292
Previous Articles Next Articles
Diagnosis and treatment of inferior tibiofibular joint injury and screw fixation: advances and problems
Chen Hong-jun, Bi Zheng-gang
- Department of Orthopedics, the First Affiliated Hospital of Harbin Medical University, Harbin 150001, Heilongjiang Province, China
-
Online:2018-08-18Published:2018-08-18 -
Contact:Bi Zheng-gang, Chief physician, Doctoral supervisor, Department of Orthopedics, the First Affiliated Hospital of Harbin Medical University, Harbin 150001, Heilongjiang Province, China -
About author:Chen Hong-jun, Department of Orthopedics, the First Affiliated Hospital of Harbin Medical University, Harbin 150001, Heilongjiang Province, China
CLC Number:
Cite this article
Chen Hong-jun, Bi Zheng-gang. Diagnosis and treatment of inferior tibiofibular joint injury and screw fixation: advances and problems [J]. Chinese Journal of Tissue Engineering Research, 2018, 22(23): 3730-3735.
share this article
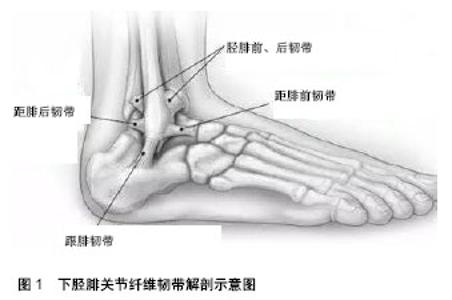
2.2 损伤机制对诊断的意义 下胫腓关节损伤在足球、橄榄球、曲棍球等球类运动员中较为常见,旋转暴力、剪切暴力以及肢体的接触均易导致下胫腓关节损伤。最常见的损伤机制是足旋前中立位遭受外旋力、距骨的翻转和足的过度背屈位[9]。 2.3 诊断方法 2.3.1 体格检查对判断下胫腓关节损伤有一定的局限性 临床工作中,单纯凭借体格检查确诊下胫腓关节损伤,结果并不可靠。因为疼痛、肿胀等症状都会影响判断,单纯通过体格检查判断下胫腓关节损伤误诊率可高达20%[10]。最传统的查体方式是触诊,相应部位压痛阳性可判断下胫腓前韧带或下胫腓后韧带损伤,二者相比,下胫腓前韧带损伤触诊结果相对可靠,阳性率可达70%[11]。 目前比较常用的体格检查包括Cotton试验、腓骨位移试验、小腿挤压试验和外旋试验。Cotton试验和腓骨位移试验可以判断下胫腓关节稳定性,这2种方法相比其他方法假阳性率较高,因为每一个医生对松弛的理解程度、体格检查时足踝摆放位置的准确性以及施加应力的大小和方向都因人而异[12]。小腿挤压试验用于判断下胫腓前韧带损伤,外旋试验用来判断下胫腓关节的损伤和三角韧带的损伤,二者被广泛认可[11]。de César等[13]对56例踝关节损伤患者的MRI和小腿挤压试验、外旋试验结果进行对比分析表明外旋试验和小腿挤压试验对诊断下胫腓关节损伤敏感性低,但特异性高。 除以上体格检查外,还有以下几种:①背屈挤压试验:适用于可耐受检查的踝关节扭伤患者,但阳性率仅为47%[11],而且没有明确的诊断价值,此方法可以用于康复锻炼,以降低症状复发率;②足跟重击试验:由Lindenfeld等[14]提出,这种方法适用于踝关节肿胀严重、无法准确触诊的患者和急性期极度不适无法配合完成背屈动作和外旋应力试验的患者,但是其缺点在于无法鉴别胫骨应力性骨折,而且其敏感性及特异性尚未得到证实;③交腿试验:由Kiter和Bozkurt[15]提出,此方法可自我检查判断下胫腓关节是否损伤,因数据过少无法证实其有效性而不建议被采用。 2.3.2 影像学检查相对更准确可靠 对于怀疑合并下胫腓关节损伤的患者,需常规行踝关节正侧位片、踝穴位片和负重位片,踝关节正侧位片应包含腓骨全长以排除Maisonneuve骨折,负重位片对下胫腓关节损伤的诊断价值更高,但是一般在急性损伤后患者无法配合完成负重位检查[16]。X射线片常用参考指标有3个:下胫腓净空间、内侧净空间和胫腓骨重叠区,其中下胫腓净空间结果最为可靠,因为拍摄角度对其结果影响较小,下胫腓净空间是指胫骨远端平台上方1 cm处的胫骨后结节外缘与腓骨内侧缘间距,大于6 mm或超过腓骨宽度的44%视为异常[17]。 其他常用影像学检查还有CT和MRI,CT主要用于显示骨性结构异常,一般不作为诊断下胫腓关节损伤的常规检查,但对于X射线无法准确判断是否有下胫腓关节撕脱骨折的患者应完善CT检查。Takao等[18]研究发现,X射线对诊断下胫腓关节损伤特异性可达100%,但敏感性差,而MRI对诊断下胫腓关节损伤敏感性和特异性均可近似或达到100%,因此怀疑下胫腓关节损伤的患者应尽快完善MRI检查。 2.3.3 术中透视和关节镜是必要的 Lui等[19]认为术中透视相比传统X射线检查敏感性更高,因为急性扭伤患者无法配合完成应力位检查,仅行踝关节正侧位片和踝穴位片易导致下胫腓关节损伤被漏诊,术中透视需在踝关节骨折得到良好复位、坚强固定后,施以hook试验,即以1枚骨钩在冠状面上向侧方牵拉腓骨远端,若腓骨向外侧移位或踝穴增宽考虑下胫腓关节损伤。 踝关节镜较术中透视更有优势,因为关节镜可以更直观的判断下胫腓韧带损伤情况。但有一定的局限性,无法良好探查骨间韧带及骨间膜等结构,而且价格昂贵,因此不作为常规检查项目。 2.4 病理分型对治疗的指导作用 见表1。"

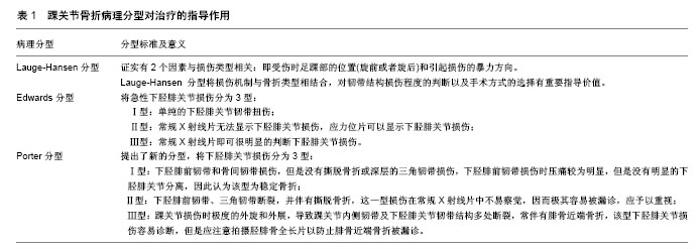
目前踝关节骨折常用的分型有Denis-Weber分型和Lauge-Hansen分型,相比Denis-Weber分型,Lauge-Hansen分型更详细的阐明了不同损伤机制、不同受伤体位、不同类型和程度暴力下的下胫腓关节损伤病理形态,因此以下主要对此分型进行赘述。该分型由Lauge-Hansen[20]于1950年首先提出,他在尸体的踝关节上进行实验,对样本施加不同类型和程度的暴力,然后对踝关节损伤情况进行记录,其证实有2个因素与损伤类型相关:受伤时足踝部的位置(旋前或者旋后)和引起损伤的暴力方向。Lauge-Hansen 分型将损伤机制与骨折类型相结合,对韧带结构损伤程度的判断以及手术方式的选择有重要指导价值。Warner等[21]通过大样本比较术前X射线、MRI和术中评估踝关节骨折中韧带损伤情况,认为 Lauge-Hansen分型可准确判断踝关节韧带损伤情况。术前根据Lauge-Hansen分型准确判断受伤机制,有助于术前计划、术中发现损伤结构,并进行手术修复处理。 Edwards等[22]将急性下胫腓关节损伤分为3型。Ⅰ型:单纯的下胫腓关节韧带扭伤;Ⅱ型:常规X射线片无法显示下胫腓关节损伤,应力位片可以显示下胫腓关节损伤;Ⅲ型:常规X射线片即可很明显的判断下胫腓关节损伤。 最近Porter[23]提出了新的分型,将下胫腓关节损伤分为3型。Ⅰ型:下胫腓前韧带和骨间韧带损伤,但是没有撕脱骨折或深层的三角韧带损伤,下胫腓前韧带损伤时压痛较为明显,但是没有明显的下胫腓关节分离,因此认为该型为稳定骨折;Ⅱ型:下胫腓前韧带、三角韧带断裂,并伴有撕脱骨折,这一型损伤在常规X射线片中不易察觉,Porter强调这一型损伤因其损伤程度较轻且不易察觉下胫腓关节失稳,因而极其容易被漏诊,应予以重视;Ⅲ型:踝关节损伤时极度的外旋和外展,导致踝关节内侧韧带及下胫腓关节韧带结构多处断裂,常伴有腓骨近端骨折(Maisonneuve fracture),该型下胫腓关节损伤容易诊断,但是应注意拍摄胫腓骨全长片以防止腓骨近端骨折被漏诊。 2.5 治疗 下胫腓关节损伤的治疗原则是恢复踝关节解剖关系,以获得良好的稳定性[24]。 2.5.1 非手术治疗 部分学者认为单纯韧带损伤的下胫腓关节损伤可以考虑选择非手术治疗,非手术治疗办法主要是以石膏或支具固定踝关节,固定3-6周,以给予下胫腓关节韧带结构充分的愈合时间。制动解除后即应开始康复锻炼,主要进行踝关节的主动和被动功能锻炼、肌肉肌力的训练和神经肌肉的支配以恢复正常步 态[25]。非手术治疗缺点在于术后复位不良的发生率较 高[26]。 2.5.2 手术治疗 手术治疗目前被广为认可,单纯修复损伤韧带不能完全恢复下胫腓关节的稳定性,还需通过复位腓骨骨折、胫骨骨折以及内踝骨折使下胫腓关节更加稳定。除了传统的下胫腓皮质骨螺钉,现在还有诸多固定方式可以选择,包括可吸收螺钉、Ilizarov环形外固定架、克氏针、弹性钢板、环扎钢丝以及锚钉等[27]。Monga等[28]调查发现95%以上的医生对于下胫腓关节损伤患者更倾向于使用传统的下胫腓皮质骨螺钉,因其被广泛认可但又存在诸多争议,故以下仅对此术式进行着重介绍。 (1)下胫腓皮质骨螺钉的使用指征:下胫腓皮质骨螺钉普遍应用于Lauge-Hansen分型的旋后外旋型、旋前外展型和旋前外旋型损伤,学者认为以下2种情况需使用下胫腓皮质骨螺钉:①高位腓骨骨折患者,即腓骨骨折线高于关节面>4.5 cm的骨折,因为腓骨高位骨折会损伤骨间膜,影响下胫腓关节稳定性;②术中Hook试验结果阳性的患者[29]。有研究认为合并外踝或内踝骨折且三角韧带完整的下胫腓关节损伤,外踝或内踝解剖复位后,可不使用皮质骨螺钉固定下胫腓关节[30];合并后踝骨折的下胫腓关节损伤,下胫腓后韧带可能尚未断裂且与骨折块相连,此时只需将后踝解剖复位即可。 (2)下胫腓皮质骨螺钉直径的选择:目前医生更青睐于使用3.5 mm和4.5 mm皮质骨螺钉,螺钉直径的选择主要根据医生的经验和喜好[31]。Hansen等[32]通过实验证实单枚4.5 mm皮质骨螺钉在抗剪切应力方面较单枚3.5 mm皮质骨螺钉更有优势。Markolf等[33]的实验研究表明,2枚3.5 mm皮质骨螺钉与2枚4.5 mm皮质骨螺钉在对抗腓骨移位无明显差异。亦有学者认为4.5 mm皮质骨螺钉发生螺钉断裂及螺钉松动的风险比3.5 mm皮质骨螺钉低,而且螺钉断裂高发期为术后3-6个月,此时韧带结构已经愈合[34]。由此可见,4.5 mm皮质骨螺钉较3.5 mm皮质骨螺钉更优,但同时也应根据患者骨骼直径选择合适直径的螺钉。 (3)下胫腓皮质骨螺钉数量的选择:Wikeroy等[35]进行了一项前瞻性试验,实验组使用1枚4.5 mm皮质骨螺钉、穿过4层皮质,术后2个月取出,对照组使用2枚 3.5 mm皮质骨螺钉、穿过3层皮质,不予以取出,随访8年,对影像学资料以及关节功能进行对比分析,结果表明二者差异无显著性意义。Jordan等[36]对86例踝关节骨折内固定患者术后3个月的影像学资料进行统计分析,结果表明使用1枚4.5 mm皮质骨螺钉与使用2枚 4.5 mm皮质骨螺钉对患者预后无明显影响。因此,在下胫腓关节相对稳定的前提下应尽量减少使用下胫腓皮质骨螺钉的数量。 (4)下胫腓皮质骨螺钉穿过皮质层数:多项生物力学实验对比分析结果表明螺钉穿过3层皮质还是4层皮质对负重情况无明显影响[33,37]。Hoiness等[38]对术后患者随访1年发现螺钉穿过3层皮质与螺钉穿过4层皮质对患者术后疼痛情况及功能预后无明显影响,Moore等[39]前瞻性实验结果表明螺钉穿过3层皮质与穿过4层皮质对术后发生螺钉断裂、螺钉松动以及复位不良等并发症概率无明显影响。 (5)下胫腓皮质骨螺钉的位置:AO创伤学会建议下胫腓皮质骨螺钉应置于胫骨远端平台上方2.0-3.0 cm处,各枚螺钉应与胫骨远端平台平行[40]。Kukreti等[41]认为下胫腓皮质骨螺钉置于胫骨远端平台上方2 cm、 3 cm与5 cm差异无显著性意义。 (6)下胫腓皮质骨螺钉的取出:对于下胫腓皮质骨螺钉是否应该予以常规取出、螺钉取出时间以及应该在下胫腓皮质骨螺钉取出之前还是之后进行功能锻炼尚未达成共识。早在1989年就有学者进行生物力学试验,标本下胫腓关节完整性良好,于标本胫骨远端平台上方 3 cm处旋入1枚4.5 mm皮质骨螺钉并穿过4层皮质,对比分析螺钉置入前后踝关节活动功能,结果表明螺钉对踝关节的背伸及跖屈无明显影响,但是对距骨的旋转有一定影响[42]。关于下胫腓皮质骨螺钉应在术后6周还是12周取出亦存在争议,术后6周取出下胫腓皮质骨螺钉降低了内固定物失效的风险,但是下胫腓关节再分离的风险明显增高[43]。Hsu等[44]回顾性分析52例患者,对比分析术后常规取出下胫腓皮质骨螺钉的患者与术后6,12,16周以后下胫腓皮质骨螺钉发生断裂的患者的术后功能,结果差异无显著性意义。Hamid等[45]认为螺钉断裂相比螺钉完整或者常规取出对下胫腓关节功能有积极影响。Miller等[46]进行了一项前瞻性研究,25例踝关节骨折伴下胫腓联合损伤患者均使用锁定接骨板及相同皮质骨螺钉,皮质骨螺钉穿过皮质层数相同,术后允许患者正常负重,仅3例患者出现并发症,1例出现螺钉断裂,2例出现螺钉松动,术后4个月常规取出所有内固定物,内固定物取出后踝关节活动度及功能评分得到明显改善。术后螺钉不取出会导致螺钉松动、螺钉断裂以及疼痛不适等并发症,取出螺钉需二次手术,导致不必要的花销及一系列并发症,如感染、下胫腓关节再分离、在取出过程中螺钉断裂等并发症,取出螺钉后相关并发症发生率高达22.4%[47]。因此,松动或断裂的螺钉无需取出,螺钉完整者应于负重前予以取出,同时使用其他内固定物的患者需于骨折愈合后予以一并取出。 2.6 术后并发症 2.6.1 复位不良 解剖复位对下胫腓关节损伤术后良好功能的恢复以及避免创伤性关节炎的发生至关重 要[48-49],然而下胫腓关节复位不良却十分常见,发生率为25.5%-52%[50-54]。Sagi等[50]对下胫腓螺钉关节损伤患者切开复位内固定以及闭合复位内固定术后复位不良发生率进行对比研究,发现闭合复位内固定术后复位不良发生率高达44%,而切开复位内固定术后复位不良发生率仅15%,复位不良患者的功能预后与下胫腓关节韧带结构愈合良好患者的功能预后相差甚远。术中应力位透视等也可以明显降低下胫腓关节复位不良发生率[53]。 2.6.2 肥胖患者和周围神经病变患者 肥胖患者和周围神经病变患者的内植物相关并发症发生率较高。Mendelsohn等[55]通过对比发现肥胖患者与体质量正常患者在下胫腓关节损伤严重程度相同情况下,肥胖患者复位不良发生率高达15%,而体质量正常患者复位不良发生率仅1.8%。Wukich等[56]发现糖尿病患者下胫腓关节损伤术后畸形愈合、骨不连发生率是非糖尿病患者的3.4倍,Charcot关节病患者下胫腓关节损伤术后内植物相关并发症发生率更高。Perry等[57]提出周围神经病变患者的下胫腓关节损伤腓骨骨折块较大时,使用腓骨金属接骨板可以降低内植物相关并发症发生率。 2.6.3 异位骨化 Taylor等[58]随访研究发现术后异位骨化发生率高达50%,异位骨化会导致下胫腓关节韧带结构骨性愈合,进而引发疼痛或关节反常活动等并发症。Droog等[59]认为异位骨化在踝关节损伤并发症中发生率较高,但对踝关节活动功能影响较小,并不影响患者日常活动,因此无需二次手术处理。 "

| [1] Bartonicek J. Anatomy of the tibiofibular syndesmosis and its clinical relevance. Surg Radiol Anat.2003; 25:379-386.[2] Beumer A,van Hemert WL,Swierstra BA,et al.A biomechanical evaluation of the tibiofibular and tibiotalar ligaments of the ankle. Foot Ankle Int. 2003;5: 426-429.[3] Porter DA. Ligamentous injuries of the foot and ankle. In: Fitzgerald RH, Kaufer H, Malkani AL, editors. Orthopaedics. St. Louis: Mosby, 2002.[4] Brosky T, Nyland J, Nitz A, et al. The ankle ligaments: consideration of syndesmotic injury and implications for rehabilitation. J Orthop Sports Phys Ther. 1995;21:197-205.[5] Taylor DC, Bassett Iii FH. Syndesmosis ankle sprains: diagnosing the injury and aiding recovery. Phys Sportsmed. 1993;21:39-46.[6] Kjaer MKM, Magnusson P, Engebretsen L, et al. Sports injury: regional considerations. Diagnosis and treatment. Textbook of sports medicine. Oxford: Blackwell Science Ltd, 2003:540-551.[7] Bloemers FW, Bakker FC. Acute ankle syndesmosis injury in athletes. Eur J Trauma. 2006;32:350-356.[8] Evans JM, Schucany WG. Radiological evaluation of a high ankle sprain. Proceedings (Baylor University Medical Center). 2006;19: 402e405.[9] Scranton PE. Isolated syndesmotic injuries: diastasis of the ankle in the athlete. Tech Foot Ankle Surg. 2002;1:88-93.[10] Van Heest TJ, Lafferty PM. Injuries to the ankle syndesmosis. J Bone Joint Surg Am. 2014;96:603-613.[11] Alonso A, Khoury L, Adams R. Clinical tests for ankle syndesmosis injury: reliability and prediction of return to function. J Orthop Sports Phys Ther. 1998;27(4):276-284.[12] Beumer A, Swierstra BA, Mulder PG. Clinical diagnosis of syndesmotic ankle instability: evaluation of stress tests behind the curtains. Acta Orthop Scand. 2002;73(6):667-669.[13] de César PC, Avila EM, de Abreu MR. Comparison of magnetic resonance imaging to physical examination for syndesmotic injury after lateral ankle sprain. Foot Ankle Int. 2011;32(12):1110-1114.[14] Lindenfeld T, Parikh S. Clinical tip: heel-thump test for syndesmotic ankle sprain. Foot Ankle Int. 2005;26(5):406-408.[15] Kiter E, Bozkurt M. The crossed-leg test for examination of ankle syndesmosis injuries. Foot Ankle Int. 2005;26(2):187-188.[16] Lin CF, Gross ML, Weinhold P. Ankle syndesmosis injuries: anatomy, biomechanics, mechanism of injury, and clinical guidelines for diagnosis and intervention. J Orthop Sports Phys Ther. 2006;36(6): 372-384.[17] Press CM, Gupta A, Hutchinson MR. Management of ankle syndesmosis injuries in the athlete. Curr Sports Med Reports. 2009; 8(5):228-233.[18] Takao M, Ochi M, Oae K, et al. Diagnosis of a tear of the tibiofibular syndesmosis. The role of arthroscopy of the ankle. Bone Joint J. 2003;85(3):324-329.[19] Lui TH, Ip KY, Chow HT. Comparison of radiologic and arthroscopic diagnoses of distal tibiofibular syndesmosis disruption in acute ankle fracture.Arthroscopy. 2005;21(11):1370.[20] Lauge-Hansen N. Fractures of the ankle. II. Combined experimentalsurgical and experimental-roentgenologic investigations. Arch Surg. 1950; 60: 957e85.[21] Warner SJ, Garner MR, Hinds RM, et al. Correlation between the Lauge-Hansen Classification and ligament injuries in ankle fractures. J Orthop Trauma. 2015;29(12);574-578.[22] Edwards GS Jr, De Lee JC. Ankle diastasis without fracture. Foot Ankle. 1984;4(6):305-312.[23] Porter DA. Evaluation and treatment of ankle syndesmosis injuries. Instr Course Lect. 2009;58:575-581.[24] Egol KA, Dolan R, Koval KJ. Functional outcome of surgery for fractures of the ankle. A prospective, randomised comparison of management in a cast or a functional brace. J Bone Joint Surg Br. 2000;82:246-249.[25] Amendola A, Williams G, Foster D. Evidence-based approach to treatment of acute traumatic syndesmosis (high ankle) sprains. Sports Med Arthrosc. 2006;14:232-236.[26] Gardner MJ, Graves ML, Higgins TF, et al. Technical considerations in the treatment of syndesmotic injuries associated with ankle fractures. J Am Acad Orthop Surg. 2015;23(8):510-518.[27] Mp VDB, Raven EE. Current concepts review: operative techniques for stabilizing the distal tibiofibular syndesmosis. Foot Ankle Int. 2007; 28(12):1302-1308. [28] Monga P, Kumar A, Simons A, et al. Management of distal tibio-fibular syndesmotic injuries: a snapshot of current practice.. Acta Orthopaedica Belgica. 2008;74(3):365-369.[29] Fallat L, Grimm DJ, Saracco JA. Sprained ankle syndrome: prevalence and analysis of 639 acute injuries.J Foot Ankle Surg. 1998;37:280-285.[30] van den Bekerom MP, Lamme B, Hogervorst M, et al. Which ankle fractures require syndesmotic stabilization? J Foot Ankle Surg. 2007; 46(6):456-463.[31] Magan A, Golano P, Maffulli N, et al. Evaluation and management of injuries of the tibiofibular syndesmosis. Br Med Bull. 2014;111(1): 101-115.[32] Hansen M, Le L, Wertheimer S, et al. Syndesmosis fixation: analysis of shear stress via axial load on 3.5-mm and 4.5-mm quadricortical syndesmotic screws. J Foot Ankle Surg. 2006;45(2):65-69.[33] Markolf KL, Jackson SR, McAllister DR. Syndesmosis fixation using dual 3.5 mm and 4.5 mm screws with tricortical and quadricortical purchase: a biomechanical study. Foot Ankle Int. 2013;34(5):734-739.[34] Stuart K, Panchbhavi VK. The fate of syndesmotic screws. Foot Ankle Int. 2011;32(5):S519-525.[35] Wikeroy AK, Hoiness PR, Andreassen GS, et al. No difference in functional and radiographic results 8.4 years after quadricortical compared with tricortical syndesmosis fixation in ankle fractures. J Orthop Trauma. 2010;24(1):17-23.[36] Jordan TH, Talarico RH, Schuberth JM. The radiographic fate of the syndesmosis after trans-syndesmotic screw removal in displaced ankle fractures. J Foot Ankle Surg. 2011;50(4):407-412.[37] Nousiainen MT, McConnell AJ, Zdero R, et al. The influence of the number of cortices of screw purchase and ankle position in Weber C ankle fracture fixation. J Orthop Trauma. 2008;22(7):473-478.[38] Hoiness P, Stromsoe K. Tricortical versus quadricortical syndesmosis fixation in ankle fractures: a prospective, randomized study comparing two methods of syndesmosis fixation. J Orthop Trauma. 2004;18: 331-337.[39] Moore JA, Shank JR, Morgan SJ, et al. Syndesmosis fixation: a comparison of three and four cortices of screw fixation without hardware removal. Foot Ankle Int. 2006;27(8):567-572.[40] Hahn DM, Colton CL. Malleolar fractures. In: Rüedi TP, Murphy WM (ed). AO Principles of Fracture Management, New York: Thieme, 2000: 559-581.[41] Kukreti S, Faraj A, Miles JN. Does position of syndesmotic screw affect functional and radinterosseous ligamentogical outcome in ankle fractures? Injury. 2005;36:1121-1124.[42] Needleman RL, Skrade DA, Stiehl JB. Effect of the syndesmotic screw on ankle motion. Foot Ankle. 1989;10(1):17-24.[43] Van Heest TJ, Lafferty PM. Injuries to the ankle syndesmosis. J Bone Joint Surg Am. 2014;96:603-613.[44] Hsu YT, Wu CC, Lee WC, et al. Surgical treatment of syndesmotic diastasis: emphasis on effect of syndesmotic screw on ankle function. Int Orthop. 2011;35(3):359-364.[45] Hamid N, Loeffler BJ, Braddy W, et al. Outcome after fixation of ankle fractures with an injury to the syndesmosis: the effect of the syndesmosis screw. J Bone Joint Surg Br. 2009;91:1069-1073.[46] Miller AN, Paul O, Boraiah S, et al. Functional outcomes after syndesmotic screw fixation and removal. J Orthop Trauma. 2010;24(1): 12-16.[47] Schepers T. Complications of syndesmotic screw removal. Foot Ankle Int. 2011.[48] Weening B, Bhandari M. Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma. 2005;19(2):102-108.[49] Lloyd J, Elsayed S, Hariharan K, et al. Revisiting the concept of talar shift in ankle fractures. Foot Ankle Int. 2006;27(10):793-796.[50] Sagi HC, Shah AR, Sanders RW. The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. J Orthop Trauma. 2012 l;26(7):439-443.[51] Song D, Lanzi J, Groth A, et al. The effect of syndesmosis screw removal on the reduction of the distal tibiofibular joint [abstract]. Read at the Annual Meeting of the American Academy of Orthopaedic Surgeons; 2012; San Francisco, CA. Paper no. 617.[52] Gardner MJ, Demetrakopoulos D, Briggs SM, et al. Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot Ankle Int. 2006;27(10): 788-792.[53] Miller AN, Carroll EA, Parker RJ, et al. Direct visualization for syndesmotic stabilization of ankle fractures. Foot Ankle Int. 2009;30(5): 419-426.[54] Marmor M, Hansen E, Han HK, et al. Limitations of standard fluoroscopy in detecting rotational malreduction of the syndesmosis in an ankle fracture model. Foot Ankle Int. 2011;32(6):616-622.[55] Mendelsohn ES, Hoshino CM, Harris TG, et al. The effect of obesity on early failure after operative syndesmosis injuries. J Orthop Trauma. 2013;27(4): 201-206.[56] Wukich DK, Kline AJ. The management of ankle fractures in patients with diabetes. J Bone Joint Surg Am. 2008;90(7):1570-1578.[57] Perry MD, Taranow WS, Manoli A 2nd, et al. Salvage of failed neuropathic ankle fractures: use of large-fragment fibular plating and multiple syndesmotic screws. J Surg Orthop Adv. 2005;14(2):85-91.[58] Taylor DC, Englehardt DL, Bassett FH 3rd. Syndesmosis sprains of the ankle. The influence of heterotopic ossification. Am J Sports Med. 1992;20(2):146-150.[59] Droog R,Verhage SM. Incidence and clinical relevance of tibiofibular synostosis in fractures of the ankle which have been treated surgically. Bone Joint J. 2015;97-B:945-949. |
| [1] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [2] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [3] | Xu Dongzi, Zhang Ting, Ouyang Zhaolian. The global competitive situation of cardiac tissue engineering based on patent analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 807-812. |
| [4] | Wu Zijian, Hu Zhaoduan, Xie Youqiong, Wang Feng, Li Jia, Li Bocun, Cai Guowei, Peng Rui. Three-dimensional printing technology and bone tissue engineering research: literature metrology and visual analysis of research hotspots [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 564-569. |
| [5] | Chang Wenliao, Zhao Jie, Sun Xiaoliang, Wang Kun, Wu Guofeng, Zhou Jian, Li Shuxiang, Sun Han. Material selection, theoretical design and biomimetic function of artificial periosteum [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 600-606. |
| [6] | Liu Fei, Cui Yutao, Liu He. Advantages and problems of local antibiotic delivery system in the treatment of osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 614-620. |
| [7] | Li Xiaozhuang, Duan Hao, Wang Weizhou, Tang Zhihong, Wang Yanghao, He Fei. Application of bone tissue engineering materials in the treatment of bone defect diseases in vivo [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 626-631. |
| [8] | Zhang Zhenkun, Li Zhe, Li Ya, Wang Yingying, Wang Yaping, Zhou Xinkui, Ma Shanshan, Guan Fangxia. Application of alginate based hydrogels/dressings in wound healing: sustained, dynamic and sequential release [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 638-643. |
| [9] | Chen Jiana, Qiu Yanling, Nie Minhai, Liu Xuqian. Tissue engineering scaffolds in repairing oral and maxillofacial soft tissue defects [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 644-650. |
| [10] | Xing Hao, Zhang Yonghong, Wang Dong. Advantages and disadvantages of repairing large-segment bone defect [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 426-430. |
| [11] | Chen Siqi, Xian Debin, Xu Rongsheng, Qin Zhongjie, Zhang Lei, Xia Delin. Effects of bone marrow mesenchymal stem cells and human umbilical vein endothelial cells combined with hydroxyapatite-tricalcium phosphate scaffolds on early angiogenesis in skull defect repair in rats [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3458-3465. |
| [12] | Wang Hao, Chen Mingxue, Li Junkang, Luo Xujiang, Peng Liqing, Li Huo, Huang Bo, Tian Guangzhao, Liu Shuyun, Sui Xiang, Huang Jingxiang, Guo Quanyi, Lu Xiaobo. Decellularized porcine skin matrix for tissue-engineered meniscus scaffold [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3473-3478. |
| [13] | Mo Jianling, He Shaoru, Feng Bowen, Jian Minqiao, Zhang Xiaohui, Liu Caisheng, Liang Yijing, Liu Yumei, Chen Liang, Zhou Haiyu, Liu Yanhui. Forming prevascularized cell sheets and the expression of angiogenesis-related factors [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3479-3486. |
| [14] | Liu Chang, Li Datong, Liu Yuan, Kong Lingbo, Guo Rui, Yang Lixue, Hao Dingjun, He Baorong. Poor efficacy after vertebral augmentation surgery of acute symptomatic thoracolumbar osteoporotic compression fracture: relationship with bone cement, bone mineral density, and adjacent fractures [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3510-3516. |
| [15] | Liu Liyong, Zhou Lei. Research and development status and development trend of hydrogel in tissue engineering based on patent information [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3527-3533. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||