Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (34): 5506-5512.doi: 10.3969/j.issn.2095-4344.2017.34.016
Previous Articles Next Articles
Complications associated with stent-assisted coil embolization of wide-neck intracranial aneurysms
- Department of Neurosurgery, General Hospital of Shenyang Military Command, Shenyang 110840, Liaoning Province, China
-
Received:2017-07-08Online:2017-12-08Published:2018-01-04 -
Contact:Gao Xu, M.D., Associate chief physician, Department of Neurosurgery, General Hospital of Shenyang Military Command, Shenyang 110840, Liaoning Province, China -
About author:Zhao Yu-long, Master, Department of Neurosurgery, General Hospital of Shenyang Military Command, Shenyang 110840, Liaoning Province, China -
Supported by:the National Natural Science Foundation of China, No. 81300990, 81671174, 81671313
CLC Number:
Cite this article
Zhao Yu-long, Zhang Hai-feng, Dong Yu-shu, Jiang Wei, Hao Guang-zhi, Liang Guo-biao, Gao Xu.
share this article
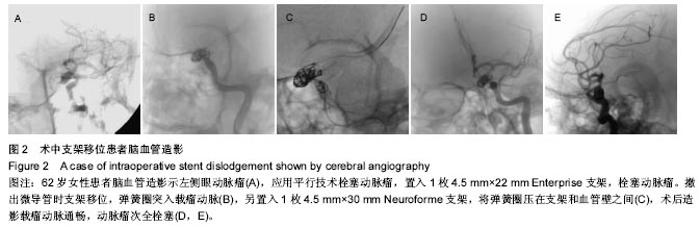
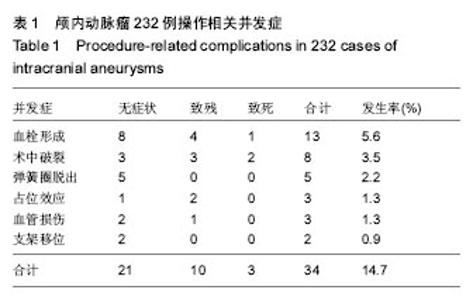
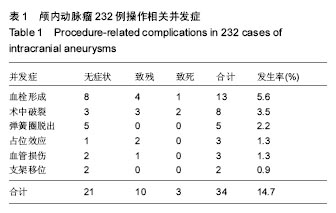
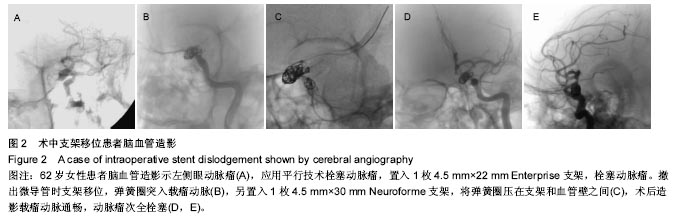
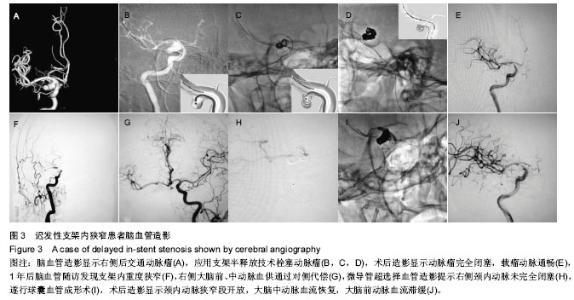
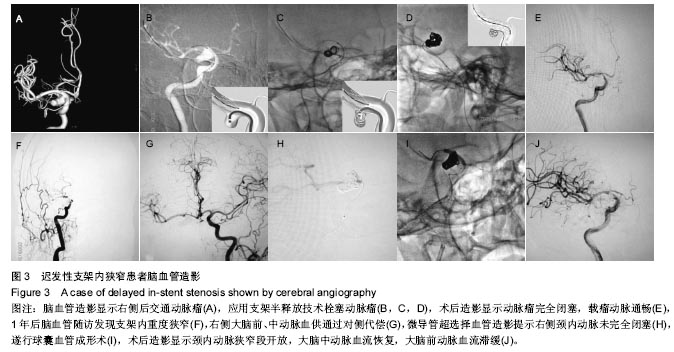
2.1.1 血栓形成 接受治疗的232例患者中,13例围手术期血栓并发症,9例为破裂动脉瘤,4例为未破裂动脉瘤。9例在术中发现,4例因术后出现缺血症状发现。9例患者经超选择溶栓和微导丝机械溶栓实现完全或部分再通。随访中8例患者完全恢复,2例患者遗留轻度神经功能障碍,2例患者偏瘫,生活不能自理。1例68岁老年女性死亡,该患者入院时Hunt-Hess分级Ⅰ级,诊断为左侧后交通动脉瘤,术后6 h出现左侧肢体肌力下降,MRI扫描显示左侧大脑半球大面积梗死,立即行脑血管造影显示支架远端血栓形成,左侧颈内动脉闭塞,抗凝、局部溶栓治疗无效,患者出现脑疝,最终行开颅减压手术,但未能挽救患者生命。 2.1.2 术中破裂 发生8例动脉瘤术中破裂,微导管穿出5例,弹簧圈穿出2例,1例由充盈球囊造成。3例后交通动脉瘤,2例眼动脉瘤,1例前交通动脉瘤,1例脉络膜前动脉瘤,1例基底动脉顶端动脉瘤。8例术中出血的动脉瘤均为破裂动脉瘤急性期,4例为栓塞微导管经支架网眼进入动脉瘤时所致。所有患者均立即给予鱼精蛋白中和肝素并迅速填塞弹簧圈直至出血停止。4例出血较多的患者(术后Fisher Ⅲ-Ⅳ级)行脑室外引流。5例导致不良后果发生,其中3例遗留神经功能障碍,2例死亡。 2.1.3 弹簧圈脱出 5例操作中发生弹簧圈脱出,其中4例为最后一个弹簧圈在解脱后部分环从支架网眼凸入载瘤动脉,1例为弹簧圈解旋进入载瘤动脉。该患者女性,71岁,双侧后交通动脉瘤,支架辅助栓塞第2个动脉瘤时输送第3枚弹簧圈致微导管头端退出动脉瘤,重新调整过程中弹簧圈解旋,后几个环干扰载瘤动脉血流,尝试多种方法撤回弹簧圈失败,遂将球囊导管送入导引导管,充盈球囊“挤住”弹簧圈的近端,同时撤回导引导管和球囊导管,将弹簧圈一级螺旋拉直至主动脉。所有患者均无临床症状。 2.1.4 占位效应 3例后交通大型动脉瘤术后出现动眼神经麻痹症状,考虑为大型动脉瘤填塞后占位效应所致。经激素治疗,1例患者完全恢复。 2.1.5 血管损伤 所有操作中出现3例血管损伤。其中2例为球囊颈内动脉虹吸段血管夹层,随访时自愈,无后遗症。另1例为67岁老年女性患者,行右侧后交通动脉瘤Neuroform支架辅助栓塞治疗,术后1 h出现意识朦胧,头CT显示右侧侧裂内约30 mL血肿,考虑为交换导丝所致的大脑中动脉损伤,立即行血肿清除术,术中未发生止血困难,患者出院时左侧肢体轻偏瘫,随访时生活自理。 2.1.6 支架移位 2例治疗中发生支架移位,1例由微导管经支架网眼送入动脉瘤所致,1例由撤回支架与血管壁之间的微导管所致。前者采用Neuroform支架,移位后仍覆盖瘤颈,顺利完成弹簧圈填塞,后者采用Enterprise支架,移位后弹簧圈部分凸入载瘤动脉,颈内动脉血流中断(颈内动脉床突上段动脉瘤),幸运的是支架释放后输送导管未撤回,立即送入另一个支架,并成功释放,将凸出部分弹簧圈压在支架与血管壁之间,血流完全恢复,无临床症状(图2)。"
2.2 蛛网膜下腔出血相关并发症 2.2.1 血管痉挛 尽管所有129例急性期破裂动脉瘤均给予足量尼莫地平和/或腰穿释放血性脑脊液,24例(18.6%)患者发生症状性血管痉挛。其中5例术中载瘤动脉闭塞(前交通动脉瘤1例,后交通动脉瘤2例,基底动脉瘤2例),术中立即超选择给予尼莫地平3 mg,罂粟碱30 mg,3例患者恢复良好,无临床症状,2例预后不良。58岁老年女性确诊基底动脉顶端动脉瘤行支架辅助栓塞术,术中基底动脉主干闭塞,立即经导引导管注射尼莫地平、罂粟碱等药物后血流恢复,术后患者出现意识障碍,MRI显示脑桥梗死,出院时患者仍意识朦胧,四肢肌力减弱,生活无法自理。另1例70岁老年男性患者,左侧颈内动脉床突上段动脉瘤(Hunt-Hess Ⅲ级),栓塞后造影发现左侧颈内动脉C2-3段痉挛变窄,立即给予抗血管痉挛药物,血管痉挛明显缓解。但术后24 h患者出现意识障碍,CT显示左侧大脑半球梗死,脑血管造影显示前、后循环广泛血管痉挛,急诊行开颅减压手术,术后意识逐渐恢复,但遗留右侧肢体偏瘫、失语。 2.2.2 脑积水 129例蛛网膜下腔出血患者中,9例(6.9%)因脑积水行脑室外引流手术。其中1例因出血量大死亡,其余8例恢复良好,临床随访没有需要接受脑室腹腔分流术的慢性脑积水患者。 2.3 随访并发症 2.3.1 支架对载瘤动脉的影响 155例患者(159个动脉瘤)接受脑血管造影随访,总体再通率为14.5%。接受造影随访的患者中2例证实支架内狭窄。1例为45岁男性患者,椎动脉梭形动脉瘤Neuroform支架辅助栓塞术后3个月随访发现约50%支架内狭窄,无临床症状,未给予外科处理,继续双抗治疗,术后12个月再次造影显示狭窄消失。另1例为65岁男性患者,右侧后交通动脉瘤,术中放置1枚4.5 mm×15 mm Neuroform支架于颈内动脉C1段,术后约1年患者出现左侧肢体无力,于术后13个月行脑血管造影,显示支架内90%狭窄,遂给予球囊血管内成形术,术后狭窄明显改善,患者症状消失(图3)。 1例患者术后6个月造影时发现开口被Neuroform支架覆盖的眼动脉闭塞,由于供血由颈外动脉分支代偿,患者无任何临床症状。 "
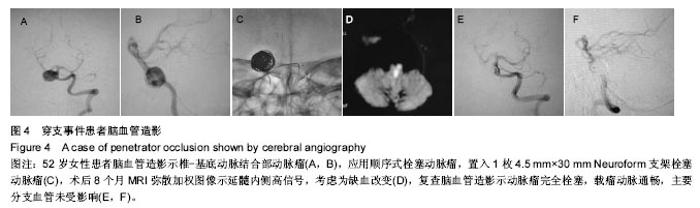
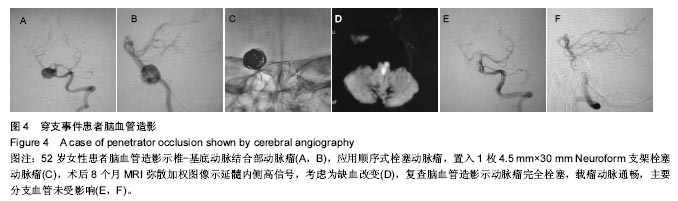
1例52岁女性患者术后8个月出现Déjérine综合征(图4)。该患者因椎-基底动脉结合部动脉瘤行支架辅助栓塞,主要症状表现为头晕、双侧深感觉障碍、右侧轻偏瘫。MRI扫描显示延髓内侧高信号。脑血管造影未发现支架内狭窄,考虑为支架内血管内皮细胞增生导致该段穿支血管闭塞。 2.3.2 出血性事件 随访中未发现治疗后动脉瘤再破裂出血。1例73岁老年男性后交通动脉瘤患者术后7个月死于对侧基底节区脑出血,该患者有20余年高血压病史,但术后抗血小板治疗是病情加重的原因之一。 2.4 急性血栓形成、术中动脉瘤破裂发生率比较 8例术中破裂、9例急性血栓事件发生在破裂动脉瘤,发生率分别为6.2%(8/129)和6.9%(9/129)。未破裂动脉瘤患者术中破裂和急性血栓事件发生率分别为0%和3.6%(4/110)。破裂动脉瘤组和未破裂动脉瘤组比较,术中破裂发生率差异有显著性意义(P=0.008);急性血栓事件发生率差异无显著性意义(P=0.256)。 2.5 患者预后 11例患者住院期间死亡,其中8例破裂动脉瘤患者(Hunt-Hess Ⅲ级4例,Ⅳ级3例,Ⅴ级1例)死于原发蛛网膜下腔出血,3例患者因操作相关并发症死亡。其余221例患者均接受临床随访,随访时间1-81个月(平均57.7个月)。无再出血病例发生。随访结果恢复良好(mRS 0分或1分)167例,较好(mRS 2分)38例,功能障碍(mRS 3分或4分)11例,5例患者痊愈出院后死于其他系统疾病。"
| [1]吴中学.合理选择脑血管病的治疗方法[J].中华神经外科杂志, 2006, 22(8) :453.[2]Higashida RT, Smith W, Gress D, et al. Intravascular stent and endovascular coil placement for a ruptured fusiform aneurysm of the basilar artery. Case report and review of the literature. J Neurosurg. 1997;87(6):944-949.[3]Wolstenholme J, Rivero-Arias O, Gray A, et al. Treatment pathways, resource use, and costs of endovascular coiling versus surgical clipping after aSAH. Stroke. 2008;39(1): 111-119.[4]Yahia AM, Gordon V, Whapham J, et al. Complications of Neuroform stent in endovascular treatment of intracranial aneurysms. Neurocrit Care. 2008;8(1):19-30.[5]Qian Z, Feng X, Kang H, et al. Ruptured Wide-Necked Aneurysms: Is Stent-Assisted Coiling During Posthemorrhage Days 4-10 Safe and Efficient. World Neurosurg. 2017;101: 137-143.[6]Lv X, Li Y, Jiang C, et al. Potential advantages and limitations of the Leo stent in endovascular treatment of complex cerebral aneurysms. Eur J Radiol. 2011;79(2):317-322.[7]张亮,吕明,李佑祥,等. 支架辅助栓塞颅内宽颈动脉瘤手术相关出血性与缺血性并发症的危险因素分析[J].中国微侵袭神经外科杂志, 2016,21(2):49-52.[8]Liang G, Gao X, Li Z, et al. Neuroform stent-assisted coiling of intracranial aneurysms: a 5 year single-center experience and follow-up. Neurol Res. 2010;32(7):721-727.[9]Yahia AM, Latorre J, Gordon V, et al. Thromboembolic events associated with Neuroform stent in endovascular treatment of intracranial aneurysms. J Neuroimaging. 2010;20(2):113-117.[10]Murayama Y, Nien YL, Duckwiler G, et al. Guglielmi detachable coil embolization of cerebral aneurysms: 11 years' experience. J Neurosurg. 2003;98(5):959-966.[11]Mericle RA, Lanzino G, Wakhloo AK, et al. Stenting and secondary coiling of intracranial internal carotid artery aneurysm: technical case report. Neurosurgery. 1998; 43(5):1229-1234.[12]Park HK, Horowitz M, Jungreis C, et al. Periprocedural morbidity and mortality associated with endovascular treatment of intracranial aneurysms.AJNR Am J Neuroradiol. 2005;26(3):506-514.[13]Linzey JR, Griauzde J, Guan Z, et al. Stent-assisted coiling of cerebrovascular aneurysms: experience at a large tertiary care center with a focus on predictors of recurrence. J Neurointerv Surg. 2016 Oct 3. [Epub ahead of print][14]Sekhon LH, Morgan MK, Sorby W, et al. Combined endovascular stent implantation and endosaccular coil placement for the treatment of a wide-necked vertebral artery aneurysm: technical case report. Neurosurgery. 1998;43(2): 380-383.[15]Lubicz B, Collignon L, Raphaeli G, et al. Solitaire stent for endovascular treatment of intracranial aneurysms: immediate and mid-term results in 15 patients with 17 aneurysms. J Neuroradiol. 2010;37(2):83-88.[16]Fiorella D, Albuquerque FC, Woo H, et al. Neuroform In-stent Stenosis: Incidence, Natural History and Treatment Strategies. Neurosurgery. 2006;59(1):34-42.[17]Shin YS, Kim BM, Suh SH, et al. Wingspan stenting for intracranial atherosclerotic stenosis: clinical outcomes and risk factors for in-stent restenosis. Neurosurgery. 2013; 72(4):596-604.[18]Biondi A, Janardhan V, Katz JM, et al. Neuroform stent-assisted coil embolization of wide-neck intracranial aneurysms: strategies in stent deployment and midterm follow-up. Neurosurgery. 2007;61(3):460-468.[19]Dos Santos Souza MP, Agid R, Willinsky RA, et al. Microstent-assisted coiling for wide-necked intracranial aneurysms. Can J Neurol Sci. 2005;32(1):71-81.[20]Park HK, Horowitz M, Jungreis C, et al. Periprocedural morbidity and mortality associated with endovascular treatment of intracranial aneurysms. AJNR Am J Neuroradiol. 2005;26(3):506-514.[21]Murayama Y, Malisch T, Guglielmi G, et al. Incidence of cerebral vasospasm after endovascular treatment of acutely ruptured aneurysms: report on 69 cases. J Neurosurg. 1997; 87(6):830-835.[22]Gruber A, Ungersböck K, Reinprecht A, et al. Evaluation of cerebral vasospasm after early surgical and endovascular treatment of ruptured intracranial aneurysms. Neurosurgery. 1998;42(2):258-267.[23]Rabinstein AA, Pichelmann MA, Friedman JA, et al. Symptomatic vasospasm and outcomes following aneurysmal subarachnoid hemorrhage: a comparison between surgical repair and endovascular coil occlusion. J Neurosurg. 2003; 98(2):319-325.[24]Mu SQ, Yang XJ, Li YX, et al. Endovascular treatment of wide-necked intracranial aneurysms using of "remodeling technique" with the HyperForm balloon. Chin Med J (Engl). 2008;121(8):725-729.[25]梁晓东,王子亮,李天晓,等. 支架辅助栓塞颅内未破裂动脉瘤三种抗血小板方案围手术期并发症发生率比较[J]. 中华放射学杂志, 2016, 5(7): 531-536.[26]Katsaridis V, Papagiannaki C, Violaris C. Embolization of acutely ruptured and unruptured wide-necked cerebral aneurysms using the neuroform2 stent without pretreatment with antiplatelets: a single center experience. AJNR Am J Neuroradiol. 2006;27(5):1123-1128. |
| [1] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [2] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [3] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [4] | He Yunying, Li Lingjie, Zhang Shuqi, Li Yuzhou, Yang Sheng, Ji Ping. Method of constructing cell spheroids based on agarose and polyacrylic molds [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 553-559. |
| [5] | He Guanyu, Xu Baoshan, Du Lilong, Zhang Tongxing, Huo Zhenxin, Shen Li. Biomimetic orientated microchannel annulus fibrosus scaffold constructed by silk fibroin [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 560-566. |
| [6] | Yang Feng, Zhao Qian, Zhang Shixuan, Zhao Tienan, Feng Bo. Effectiveness and safety of rapamycin combined with CD133 antibody stent in preventing vascular restenosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 579-584. |
| [7] | Chen Xiaoxu, Luo Yaxin, Bi Haoran, Yang Kun. Preparation and application of acellular scaffold in tissue engineering and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 591-596. |
| [8] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [9] | Shen Jiahua, Fu Yong. Application of graphene-based nanomaterials in stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 604-609. |
| [10] | Zhang Tong, Cai Jinchi, Yuan Zhifa, Zhao Haiyan, Han Xingwen, Wang Wenji. Hyaluronic acid-based composite hydrogel in cartilage injury caused by osteoarthritis: application and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 617-625. |
| [11] | Li Hui, Chen Lianglong. Application and characteristics of bone graft materials in the treatment of spinal tuberculosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 626-630. |
| [12] | Gao Cangjian, Yang Zhen, Liu Shuyun, Li Hao, Fu Liwei, Zhao Tianyuan, Chen Wei, Liao Zhiyao, Li Pinxue, Sui Xiang, Guo Quanyi. Electrospinning for rotator cuff repair [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 637-642. |
| [13] | Guan Jian, Jia Yanfei, Zhang Baoxin , Zhao Guozhong. Application of 4D bioprinting in tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 446-455. |
| [14] | Liu Jiali, Suo Hairui, Yang Han, Wang Ling, Xu Mingen. Influence of lay-down angles on mechanical properties of three-dimensional printed polycaprolactone scaffolds [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2612-2617. |
| [15] | Huang Bo, Chen Mingxue, Peng Liqing, Luo Xujiang, Li Huo, Wang Hao, Tian Qinyu, Lu Xiaobo, Liu Shuyun, Guo Quanyi . Fabrication and biocompatibility of injectable gelatin-methacryloyl/cartilage-derived matrix particles composite hydrogel scaffold [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2600-2606. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||