Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (14): 2266-2273.doi: 10.3969/j.issn.2095-4344.2017.14.022
Previous Articles Next Articles
Three-dimensional printing technology preparation of bone tissue engineering scaffold materials in bone defect repair
Dang Ying1, Li Yue2, Li Rui-yu3, Wu Li-ping4, Guo Ya-jing5, Song Rui-jia1
- 1 Xingtai Medical College, Xingtai 054000, Hebei Province, China; 2 Department of Applied Psychology, Chengde Medical University, Chengde 067000, Hebei Province, China; 3 Second Affiliated Hospital of Xingtai Medical College, Xingtai 054000, Hebei Province, China; 4 Xingtai People’s Hospital of Hebei Medical University, Xingtai 054001, Hebei Province, China; 5Shanxi Boai Hospital, Taiyuan 030001, Shanxi Province, China
-
Received:2017-03-09Online:2017-05-18Published:2017-06-10 -
Contact:Li Rui-yu, Professor, Chief physician, Master’s supervisor, Second Affiliated Hospital of Xingtai Medical College, Xingtai 054000, Hebei Province, China -
About author:Dang Ying, Master, Lecturer, Xingtai Medical College, Xingtai 054000, Hebei Province, China -
Supported by:the Funded Project of Hebei Provincial Administration of Traditional Chinese Medicine, No. 2012068
CLC Number:
Cite this article
Dang Ying, Li Yue, Li Rui-yu, Wu Li-ping, Guo Ya-jing, Song Rui-jia. Three-dimensional printing technology preparation of bone tissue engineering scaffold materials in bone defect repair[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(14): 2266-2273.
share this article
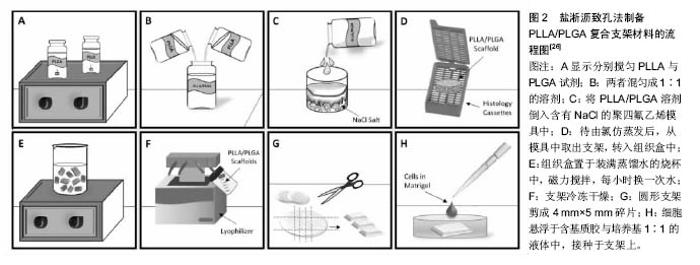
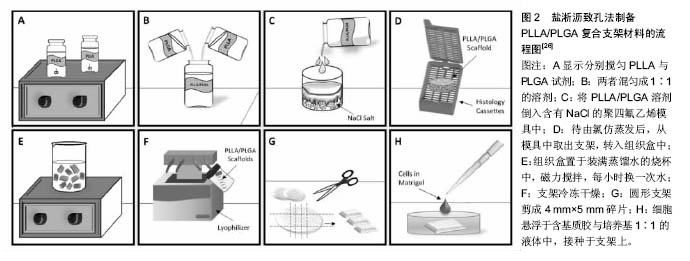
2.1 骨组织工程支架材料 骨组织工程是未来骨修复的发展方向,它用可生物降解的材料制造与骨骼形状和物理性能相似的、疏松多孔的人工骨支架作为新骨生长成型的载体,可以诱导成骨细胞生长并为新骨生长提供条件。其中人工骨支架的制造尤为重要。3D打印技术打破了传统的加工模式,不再以去除材料为主,而是一种基于逐层累加方式发展起来的先进制造技术。由于具有快速性和高度柔性的优点,在骨支架制造方面有广泛的应用前景。采用3D打印技术可以实现个性化定制人工骨。3D打印技术能够根据不同患者需要,快速精确制备适合不同患者的个性化生物医用高分子材料,并能同时对材料的微观结构进行精确控制[20-23]。因此,这种新兴的医用高分子材料制备技术在未来生物医学应用尤其是骨组织工程应用中具有独特的优势。 聚合物骨组织工程支架材料是由一种单体经聚合反应而成的产物,分子具有重复的结构单位。目前可用作骨组织工程支架材料的聚合物包括人工合成和天然来源的聚合物。天然可降解聚合物包括胶原蛋白、纤维素、聚糖、甲壳素、壳聚糖及其衍生物等;人工合成的聚合物包括聚羟基酸酯类、聚己内酯、聚氰基丙烯酸酯等。然而,高质量的胶原蛋白提纯成本高,并且需要去除末端肽以降低抗其原性,所以价格昂贵,这是材料难以推广应用的原因之一。此外,传统胶原海绵支架是将胶原溶解,通过戊二醛等交联剂进行交联重建得到的,而戊二醛会随着胶原支架在体内降解后释放,这可能会对机体产生毒性。因此,目前世界范围内迫切需要成本较低、生物活性高、可实现体内骨组织重建和初始强度高的高性能骨组织工程支架材料。 现今,人们在研制各种聚合物含氧化物、含过氧化氢化合物及含羰基的化合物。高分子聚合物是由一种或几种结构单元主要以共价键连接起来的高分子量的化合物,也称高聚物、高分子化合物、大分子化合物等。这种高聚物在阳光照射下会光解成低分子的有机物并能被生物进一步降解而成无害物。降解速度是高分子聚合物最重要的指标,影响此类聚合物降解速度的因素有聚合物相对分子量、结晶形态、材料组成、分子结构、玻璃转变温度、亲水性、几何形态、合成方式、加工条件以及酶、介质的pH值、微生物、超声波、电磁等外部因素。聚合物的分子量越大,其降解速度越慢[24-27]。一般聚L-乳酸较聚DL-乳酸易达到高分子量,力学强度较高,而较多应用于骨科内固定材料,但聚L-乳酸生物相容性一般,缓慢降解后易出现并发症。 用左旋聚乳酸,聚羟基乙酸等可降解吸收性高分子材料加工而成的纤维状支架材料和海绵状支架材料在软骨组织工程中已获得广泛应用。但这类支架材料存在着弹性模量低,受力时易变形,容易导致种子细胞损伤和降解吸收时间过长等缺陷。聚乳酸是具有良好的生物相容性和生物降解特性的聚合物,被广泛用于骨组织工程支架的研发中[28-31](图1)。为改善聚乳酸作为骨组织工程支架材料降解速率过快、亲水性差和降解产物呈酸性等缺点,李立华等[32]研究制备了一系列高孔隙率的聚乳酸/壳聚糖三维多孔复合支架材料,通过软骨细胞培养、动物皮下和肌肉植入试验对其进行了生物相容性研究,软骨细胞培养试验表明软骨细胞能在复合支架材料贴附增殖,材料无明显毒性;植入试验结果显示纯聚乳酸在体内2个月左右已经降解吸收,失去力学强度,复合材料3个月后仍能保持一定的力学强度和形状,而且组织切片也同时表明复合材料的炎症反 应远远低于纯聚乳酸材料。 生物陶瓷以其较高的机械强度、极佳的生物相容性、内部良好的三维空隙结构、生物可降解性以及可促进干细胞向成骨细胞分化与增殖等优点,骨组织工程成为理想的人工支架材料。磷酸钙是一种具有良好的骨传导性能、成骨性能及可控降解性能的新型多孔生物陶瓷材料,主要包括含硅羟基磷灰石和含硅磷酸三钙[33-35]。在骨组织工程中,磷酸钙是较为理想的骨替代材料。磷酸钙自身不具有成骨性能,这是作为骨支架材料的一大缺憾,有待更深入研究。有学者比较了生物活性陶瓷和生物降解陶瓷材料的特点和应用范围,并介绍了它们在降解性、力学强度等方面的研究。在这些材料中,聚磷酸钙生物陶瓷是作为骨组织工程支架比较新型的材料,其有望使降解速率可控,且有可能达到所需的机械强度,已经引起了广泛的关注。为修复创伤及病理因素导致的骨缺损,骨组织工程是一项迅速发展、不断革新的课题。随着近些年骨组织工程技术的发展,陶瓷支架的制作方法不断涌现并日趋成熟。高空隙率生物陶瓷支架是骨组织工程中的研究热点,但其陶瓷本身的脆性和高空隙率带来的强度差等问题限制了其在临床中的应用。随着陶瓷工艺的进步,一些增强补韧的方法应运而生,主要包括纤维增韧、晶须增韧、颗粒增韧、复合增韧、自增韧等,这些方法使陶瓷材料的强度和韧性有了较大提高[36-37]。 金属材料是目前临床骨科中应用最广泛的生物材料之一,其中金属钛及镁在骨组织工程支架方面的应用日趋成熟。镁是人体中不可缺少的矿质元素之一,在体内可逐渐降解生成镁离子,并被周围肌体组织吸收或通过体液排出体外;镁的密度与人体骨密度极为接近;镁的弹性模量与人骨非常接近,可以有效减少应力屏蔽效应。因此,很多研究人员提出将多孔镁金属作为一种新型的骨组织工程支架材料。镁及其合金由于具有良好的生物学特性、力学相容性以及可降解性,有望作为一种新型骨组织工程支架材料。金鑫鑫等[38]通过实验结果证实纯镁材料和镁合金材料无细胞毒性和遗传毒性,无急性全身毒性,而不产生溶血现象,与细胞复合后,具有良好的生物相容性。镁及其合金是一类很有应用前景的新型生物可降解医学材料。镁的化学性质活泼,采用粉末冶金等传统方法制备多孔镁存在一定的技术难度。而根据骨组织结构的特点,利用金属材料优良的可加工性能,有研究提出采用机械打孔加工技术制备直孔、连通型多孔镁金属[39]。该方法的优点是制备出的多孔镁合金支架不仅其孔的形状为圆柱形、孔隙均匀、孔与孔之间相互贯通,更重要的是其孔隙率、孔径及孔的排布等参数易于调节。 钛金属具有良好的力学性能和弹性模量,抗腐蚀性好,生物相容性高,已逐步被应用于临床。钛金属及钛金属复合材料作为骨科替代材料适用于成骨细胞的外环境,不仅能提高植入材料与周围骨组织的整合性,还能增强成骨细胞的功能性,促进骨组织再形成,植入材料多由钛及其合金制成。传统植入材料均表现出不同程度上的物理学及生物学性能缺陷。相比而言,钛金属材料具有较好的弹性模量、较高的摩擦系数以及优良的生物相容性、骨再生能力[40-43]。有学者认为传统方法修复损伤的骨组织工程支架材料常遇到组织相容性不佳,材料不足,无法随个体生长等问题,极大降低修复体的应用效果,而钛作为骨组织工程支架材料具有操作简便,排斥反应小,可任意塑形,植入后能与宿主骨形成紧密的骨性结合,且有一定的固定支持作用,从而能获得满意的骨缺损修复。众多研究证实钛金属及其合金作为骨组织工程支架材料适用于成骨细胞的外环境,不仅能提高植入材料与周围骨组织的整合性,还能增强成骨细胞的功能性,促进骨组织再形成[44-46]。因此,随着材料制作工艺的日趋成熟,钛金属在骨科临床应用的中早期治疗效果令人鼓舞,可能会为未来骨科学发展带来深远的影响。 传统的生物材料包括生物陶瓷、玻璃、金属和高分子材料,因为不具有生物活性,对骨组织进行修复之后,会产生许多固有的问题,如结合差、磨损、腐蚀,特别是无法形成具有生物功能的骨组织,难以从根本上解决患者的痛苦和实现缺损部位的功能。复合支架材料具有良好的生物相容性和骨组织修复能力,可以真正实现骨组织体内重建,是一种有应用前景的骨组织工程支架材料[47-50]。聚磷酸钙、聚右旋乳酸支架材料具有高的孔隙率,孔隙率在80%-93%之间,压缩模量比纯聚乳酸支架的压缩模量有了明显提高,具有可控的降解性能,能为细胞的培养提供三维空间环境。有研究结果提示聚磷酸钙纤维增强聚右旋乳酸支架复合材料的力学性能和生物降解特性基本满足软骨组织工程的要求,故可用作软骨组织工程支架材料。羟基磷灰石复合材料具有良好的生物活性和骨传导性,是目前骨科临床上对骨骼进行修复的重要替换材料,但其机械性能不理想,韧性差,不能很好的符合骨组织修复支架材料的要求。聚己内酯和聚乳酸是被美国食品药物管理局认证的用于骨组织工程修复的材料,具有良好的生物相容性和可降解性能。然而,单一材料很难满足骨组织工程各方面的要求,因此通过加入无机材料羟基磷灰石改善支架材料的生物活性。同样聚乳酸和磷酸钙陶瓷都是骨组织工程中常用的可降解生物材料。前者是人工合成的多聚物,在体内降解时间较长,可起到临时支架的作用,不同结构的聚乳酸又有不同的生物特性;后者生物活性好,亲和性高,但是脆性大,抗折强度低。两者的复合物在一定程度上弥补了各自的不足,能成为新型的骨组织工程支架材料[51-53]。聚乳酸纳米纤维模仿了骨中有机基质胶原纤维的形态,但由于聚乳酸呈疏水性,缺乏细胞识别位点,因而限制了聚乳酸纳米纤维支架进一步的应用。有研究使用天然生物活性材料卵磷脂作为改性剂,通过共混的方式引入到支架内部,改善聚乳酸纳米纤维支架的亲水性和细胞相容性[54]。 2.2 3D打印技术 3D打印技术是一种新型技术,能将数字信号转化为物理实体。3D打印技术的原理是原料供给装置送出的粉末被加工平台上的滚筒铺撤成一层很薄的原料,喷嘴喷出黏接剂,使层层粉末相黏形成实物模型。经过几十年的发展,目前已经开发出多种3D打印技术路径,从大类上划分为挤出成型、粒状物料成型、光聚合成型和其他成型几大类。 光聚合成型主要包括光固化、数字光处理、聚合物喷射,其中光固化快速成型技术的原理是液态光敏树脂经紫外激光在计算机控制下跟踪层状截面轨迹的逐点扫描,产生光聚合反应,从而发生同化,层层固化堆积 形成实物。早期的光固化形式是利用光能的化学和热作用可使液态树脂材料产生变化的原理,对液态树脂进行有选择地光固化,就可以在不接触的情况下制造所需的三维实体模型,利用这种光固化的技术进行逐层成形的方法,称之为光固化立体印刷。光固化立体印刷技术是国内外公认的一种应用前景最为广阔、技术最成熟、发展最迅速、研究最深入的成型方法[55-56]。它不仅具有制造周期短、材料利用率接近100%的优点还可以成型复杂、精密零件,且快速可靠、无污染、制造成本低。但用该方法制成的零件的精度却一直难以提高,严重地困扰着整个制造业,限制了该技术的实际应用和推广。 粒状物成型技术路径主要包括电子束熔化成型、选择性激光烧结、三维打印、选择性激光烧结等。 选择性激光烧结是一种采用二氧化碳激光器将混合粉末进行选择性烧结,并层层堆积形成三维实体的工艺方法。选择性激光烧结是3D快速成型技术中应用最为广泛的加工方式之一,利用激光将粉末材料熔合成固体物,其独特的工艺原理特别适合于加工医学上使用的具有多孔状结构的骨组织仿生支架。选择性激光烧结法的原理就像一点点堆积材料,通过粉末材料金属粉末或非金属粉末的层层堆积,二维的平面图形就能被堆叠出立体结构。选择性激光烧结技术作为3D打印技术中的关键一环,近年来引起各国重视[57-58]。相比光固化成型法,选择性激光烧结法的一个明显优势在于,由于是利用固体原料,所以对于悬空的物件不需要额外的支撑物。然而也不能一概而论选择性激光烧结法已经能完全取代光固化成型法了,较好的表面抛光和精确度是光固化成型法它的特点,两种技术各有优劣,在选择之前需根据不同应用方式明确需要的是什么样的材料。作为最广泛使用塑料材质,尼龙材料的众多用途,是使选择性激光烧结技术发展的重要基石。选择性激光烧结技术的一个先决条件是,材料必须能够以细微粉末的形式获得。丁冉等[59]采用选择性激光烧结法制作的多孔钛合金支架展现了良好的体外相容性,能够有利于长段骨缺损的修复,不仅能够避免应力遮挡现象,且具有良好的骨传导性,此研究就选择性激光烧结法在制作医学物理模型和制作修复人下颌骨缺损的个性化钛植入体支架方面作了初步的探索,为选择性激光烧结法在医学领域的广泛应用奠定了基础。同样借助三坐标激光扫描仪对人体牙齿完成三维外型仿生建模,采用选择性激光烧结技术成型具有与人骨支架结构较为一致的多孔金属人工骨支架试样,研究了成型工艺对试样结构特性的影响规律,为个体化人工骨仿生制造技术的研究奠定了良好的基础[60]。 挤出成型主要代表技术路径为熔融沉积成型,其基本思路是在计算机控制下将热塑性材料层层堆积成形。熔融沉积成型是目前应用最为广泛的3D打印技术,具有制造成本低、制件后期处理难度小、设备轻巧环保等特点。由于熔融沉积成型工艺高效环保的特点迎合了快速成型技术走向民用的发展趋势,因此,自主开发一套结构简单,功能稳定的熔融沉积成型快速成型设备必然具有很大的商业价值。对于3D打印而言,材料是关键所在,熔融沉积成型技术路径涉及的材料主要包括成型材料和支撑材料。成型材料是利用熔融沉积成型技术实现3D打印的载体,对其黏度、熔融温度、黏结性、收缩率等方面均有较高的要求,主要为热塑性材料,包括树脂、聚乳酸、人造橡胶、石蜡等[61]。支撑材料是在3D打印过程中对成型材料起到支撑作用的部分,在打印完成后,支撑材料需要进行剥离,因此也要求其具有一定的性能,目前采用的支撑材料一般为水溶性材料,即在水中能够溶解,方便剥离。 与光固化立体印刷、选择性激光烧结技术等成熟3D打印技术相比,熔融沉积成型技术具有自己的特点,总体来说,由于在加工过程中不涉及激光技术,整体设备体积较小,耗材获取较为容易,打印成本也相对较低,因此熔融沉积成型技术路径是面向个人的3D打印的首选技术,通过采用熔融沉积成型技术的3D打印,设计人员可以在很短的时间内设计并制作出产品原型,并通过实体对产品原型进行改进,与传统的计算机建模相比,能够真实的将实物展现在设计人员的面前[62-63]。然而其存在的缺点是成型时间较长,且在成型过程中需要加入支撑材料,在打印完成后要进行剥离,对于一些复杂构件来说,剥离存在一定的困难。随着技术的进步,一些采用3D打印厂家已经推出了不需要支撑材料的机型,该缺点正在被逐步克服。 其他技术包括激光熔覆快速制造技术、熔丝制造、 融化压模、分层实体制造等。分层实体制造是以箔材和纸等为原料,根据零件分层形态进行切割,然后将所获得的层片黏接成实体,因此也称为叠层实体制造。3D打印技术颠覆了目前制造业现状,显示出巨大潜力正引起世界科技及产业变革,尤其是在医学领域的应用,其个性化、高仿生、精密制造等特点将给医疗产品带来全新的制造手段和工艺[64-65]。3D打印技术作为一项前沿性技术,已逐步渗入到临床诊疗过程中。影像学、数字化医学、材料医学和组织工程学的快速发展,不断促进着3D打印技术在整形外科领域内的创新和拓展。不仅如此,3D打印技术也在基础研究方面广泛开展。目前,3D打印技术已被应用于软骨、血管、皮瓣等研究领域。最近的研究显示3D打印技术由于具有快速性和高度柔性的优点,在骨组织工程支架制造方面有广泛的应用前景。 "
| [1]Drosse I, Volkmer OE, Capanna R, et al. Tissue engineering for bone defect healing: an update on a multi-component approach. Injury. 2008;39 Suppl 2:S9-20. [2]Xing J, Jin H, Hou T, et al. Establishment of a bilateral femoral large segmental bone defect mouse model potentially applicable to basic research in bone tissue engineering.J Surg Res. 2014;192(2):454-463. [3]Boos AM, Arkudas A, Kneser U, et al. Bone tissue engineering for bone defect therapy. Handchir Mikrochir Plast Chir. 2010;42(6):360-368. [4]Wang C, Wang Z, Li A, et al. Repair of segmental bone-defect of goat's tibia using a dynamic perfusion culture tissue engineering bone.J Biomed Mater Res A. 2010;92(3): 1145-1153. [5]van der Pol U, Mathieu L, Zeiter S, et al. Augmentation of bone defect healing using a new biocomposite scaffold: an in vivo study in sheep. Acta Biomater. 2010;6(9):3755-3762. [6]Sathy BN, Watson BM, Kinard LA, et al. Bone Tissue Engineering with Multilayered Scaffolds-Part II: Combining Vascularization with Bone Formation in Critical-Sized Bone Defect. Tissue Eng Part A. 2015;21(19-20):2495-2503. [7]Cunniffe GM, Vinardell T, Murphy JM, et al. Porous decellularized tissue engineered hypertrophic cartilage as a scaffold for large bone defect healing. Acta Biomater. 2015;23:82-90. [8]Tayton E, Purcell M, Smith JO, et al. The scale-up of a tissue engineered porous hydroxyapatite polymer composite scaffold for use in bone repair: an ovine femoral condyle defect study.J Biomed Mater Res A. 2015;103(4):1346-1356. [9]Moshiri A, Shahrezaee M, Shekarchi B, et al. Three-Dimensional Porous Gelapin-Simvastatin Scaffolds Promoted Bone Defect Healing in Rabbits. Calcif Tissue Int. 2015;96(6):552-564. [10]Pan Z, Duan P, Liu X, et al. Effect of porosities of bilayered porous scaffolds on spontaneous osteochondral repair in cartilage tissue engineering. Regen Biomater. 2015;2(1):9-19. [11]Kido HW, Tim CR, Bossini PS, et al. Porous bioactive scaffolds: characterization and biological performance in a model of tibial bone defect in rats.J Mater Sci Mater Med. 2015;26(2):74.[12]Cheng N, Dai J, Cheng X, et al. Porous CaP/silk composite scaffolds to repair femur defects in an osteoporotic model. J Mater Sci Mater Med. 2013;24(8):1963-1975. [13]Pati F, Song TH, Rijal G, et al. Ornamenting 3D printed scaffolds with cell-laid extracellular matrix for bone tissue regeneration. Biomaterials. 2015;37:230-241. [14]Zhang W, Lian Q, Li D, et al. [Cartilage repair and subchondral bone reconstruction based on three-dimensional printing technique]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2014; 28(3):318-324.[15]Xu N, Wei F, Liu X, et al. Reconstruction of the Upper Cervical Spine Using a Personalized 3D-Printed Vertebral Body in an Adolescent With Ewing Sarcoma. Spine (Phila Pa 1976). 2016; 41(1):E50-54. [16]Tarafder S, Koch A, Jun Y, et al. Micro-precise spatiotemporal delivery system embedded in 3D printing for complex tissue regeneration.Biofabrication. 2016;8(2):025003. [17]Carrel JP, Wiskott A, Scherrer S, et al. Large Bone Vertical Augmentation Using a Three-Dimensional Printed TCP/HA Bone Graft: A Pilot Study in Dog Mandible. Clin Implant Dent Relat Res. 2016;18(6):1183-1192.[18]Mozdzen LC, Rodgers R, Banks JM, et al. Increasing the strength and bioactivity of collagen scaffolds using customizable arrays of 3D-printed polymer fibers. Acta Biomater. 2016;33:25-33. [19]Chia HN, Wu BM.Recent advances in 3D printing of biomaterials.J Biol Eng. 2015;9:4.[20]Luo Y, Zhai D, Huan Z, et al.Three-Dimensional Printing of Hollow-Struts-Packed Bioceramic Scaffolds for Bone Regeneration. ACS Appl Mater Interfaces. 2015;7(43): 24377-24383. [21]Kao CT, Lin CC, Chen YW, et al. Poly(dopamine) coating of 3D printed poly(lactic acid) scaffolds for bone tissue engineering. Mater Sci Eng C Mater Biol Appl. 2015;56:165-173.[22]Inzana JA, Olvera D, Fuller SM, et al. 3D printing of composite calcium phosphate and collagen scaffolds for bone regeneration. Biomaterials. 2014;35(13):4026-4034. [23]Ge Z, Tian X, Heng BC, et al. Histological evaluation of osteogenesis of 3D-printed poly-lactic-co-glycolic acid (PLGA) scaffolds in a rabbit model. Biomed Mater. 2009;4(2):021001. [24]Wang DX, He Y, Bi L, et al. Enhancing the bioactivity of Poly(lactic-co-glycolic acid) scaffold with a nano-hydroxyapatite coating for the treatment of segmental bone defect in a rabbit model. Int J Nanomedicine. 2013;8: 1855-1865. [25]Wu DJ, Hao AH, Zhang C, et al. [Promoting of angiogenesis and osteogenesis in radial critical bone defect regions of rabbits with nano-hydroxyapatite/collagen/PLA scaffolds plus endothelial progenitor cells]. Zhonghua Yi Xue Za Zhi. 2012; 92(23):1630-1634. [26]Niu X, Fan Y, Liu X, et al. Repair of bone defect in femoral condyle using microencapsulated chitosan, nanohydroxyapatite/collagen and poly(L-lactide)-based microsphere-scaffold delivery system. Artif Organs. 2011; 35(7):E119-128.[27]Wei A, Liu S, Peng H, et al. [An experimental study on repairing bone defect with composite of beta-tricalcium phosphate-hyaluronic acid-type I collagen-marrow stromal cells]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2005; 19(6):468-472[28]Zhou R, Xu W, Chen F, et al.Amorphous calcium phosphate nanospheres/polylactide composite coated tantalum scaffold: facile preparation, fast biomineralization and subchondral bone defect repair application. Colloids Surf B Biointerfaces. 2014;123:236-245.[29]Bodakhe S, Verma S, Garkhal K, et al. Injectable photocrosslinkable nanocomposite based on poly(glycerol sebacate) fumarate and hydroxyapatite: development, biocompatibility and bone regeneration in a rat calvarial bone defect model. Nanomedicine (Lond). 2013;8(11):1777-1795. [30]Wu DJ, Hao AH, Zhang C, et al. [Promoting of angiogenesis and osteogenesis in radial critical bone defect regions of rabbits with nano-hydroxyapatite/collagen/PLA scaffolds plus endothelial progenitor cells]. Zhonghua Yi Xue Za Zhi. 2012; 92(23):1630-1634.[31]Bertoldi C, Zaffe D, Consolo U. Polylactide/polyglycolide copolymer in bone defect healing in humans. Biomaterials. 2008;29(12):1817-1823.[32]李立华,焦延鹏,李志忠,等.聚乳酸壳聚糖复合支架材料的生物相容性研究[J].中国生物医学工程学报究,2005,24(4):504-506.[33]Zhou R, Xu W, Chen F, et al.Amorphous calcium phosphate nanospheres/polylactide composite coated tantalum scaffold: facile preparation, fast biomineralization and subchondral bone defect repair application.Colloids Surf B Biointerfaces. 2014;123:236-245.[34]Lee JH, Ryu MY, Baek HR, et al. Fabrication and evaluation of porous beta-tricalcium phosphate/hydroxyapatite (60/40) composite as a bone graft extender using rat calvarial bone defect model. Scientific World J. 2013;2013:481789. [35]Peng J, Wen C, Wang A, et al. Micro-CT-based bone ceramic scaffolding and its performance after seeding with mesenchymal stem cells for repair of load-bearing bone defect in canine femoral head. J Biomed Mater Res B Appl Biomater. 2011;96(2):316-325. [36]Balçik C, Tokdemir T, Senköylü A, et al. Early weight bearing of porous HA/TCP (60/40) ceramics in vivo: a longitudinal study in a segmental bone defect model of rabbit.Acta Biomater. 2007;3(6):985-996. [37]Nitzsche H, Lochmann A, Metz H, et al. Fabrication and characterization of a biomimetic composite scaffold for bone defect repair. J Biomed Mater Res A. 2010;94(1):298-307. [38]金鑫鑫,耿芳,谭丽丽,等.纯镁及镁合金材料用于骨组织工程的初步研究[J].沈阳药科大学学报,2008,25(S1):133.[39]龚明明.骨组织工程支架用新型多孔镁的力学性能分析[D].中国科学院金属研究所,2008.[40]Bénichou L, Caillot A, Veyssière A, et al. Bicortical reconstruction of a large calvarial bone defect with Hydroset? osteoconductive cement and titanium mesh. A preliminary study. Rev Stomatol Chir Maxillofac Chir Orale. 2014;115(6):377-381. [41]Sumida T, Otawa N, Kamata YU, et al. Custom-made titanium devices as membranes for bone augmentation in implant treatment: Clinical application and the comparison with conventional titanium mesh. J Craniomaxillofac Surg. 2015; 43(10):2183-2188. [42]Zhang M, Wang GL, Zhang HF, et al. Repair of segmental long bone defect in a rabbit radius nonunion model: comparison of cylindrical porous titanium and hydroxyapatite scaffolds.Artif Organs. 2014;38(6):493-502.[43]Yang J, Chen HJ, Zhu XD, et al. Enhanced repair of a critical-sized segmental bone defect in rabbit femur by surface microstructured porous titanium.J Mater Sci Mater Med. 2014; 25(7):1747-1756.[44]Tang ZY, Li P, Cha XF. [Short-term effects on reconstruction of Paprosky type III severe acetabulum bone defect with tantalum metal block]. Zhongguo Gu Shang. 2015;28(12): 1137-1140. [45]Zhang M, Wang GL, Zhang HF, et al. Repair of segmental long bone defect in a rabbit radius nonunion model: comparison of cylindrical porous titanium and hydroxyapatite scaffolds. Artif Organs. 2014;38(6):493-502. [46]Guo Z, Iku S, Mu L, et al. Implantation with new three-dimensional porous titanium web for treatment of parietal bone defect in rabbit. Artif Organs. 2013;37(7):623-628. [47]Kawai T, Suzuki O, Matsui K, et al. Octacalcium phosphate collagen composite facilitates bone regeneration of large mandibular bone defect in humans. J Tissue Eng Regen Med. 2015. [48]Zhou R, Xu W, Chen F, et al. Amorphous calcium phosphate nanospheres/polylactide composite coated tantalum scaffold: facile preparation, fast biomineralization and subchondral bone defect repair application. Colloids Surf B Biointerfaces. 2014;123:236-245.[49]Nitzsche H, Lochmann A, Metz H, et al. Fabrication and characterization of a biomimetic composite scaffold for bone defect repair.J Biomed Mater Res A. 2010;94(1):298-307. [50]Zhang H, Fu QW, Sun TW, et al. Amorphous calcium phosphate, hydroxyapatite and poly(d,l-lactic acid) composite nanofibers: Electrospinning preparation, mineralization and in vivo bone defect repair. Colloids Surf B Biointerfaces. 2015; 136:27-36. [51]Zhou R, Xu W, Chen F, et al. Amorphous calcium phosphate nanospheres/polylactide composite coated tantalum scaffold: facile preparation, fast biomineralization and subchondral bone defect repair application.Colloids Surf B Biointerfaces. 2014;123:236-245.[52]Kawai T, Echigo S, Matsui K, et al. First clinical application of octacalcium phosphate collagen composite in human bone defect.Tissue Eng Part A. 2014;20(7-8):1336-1341. [53]Zhou L, Hu CJ, Xu GP, et al. In vitro and in vivo study of calcium polyphosphate fiber/calcium phosphate cement/micromorselized bone composite for bone defect repair. J Biomed Mater Res B Appl Biomater. 2012;100(5):1190-1197. [54]潘洋.聚乳酸/卵磷脂复合骨组织工程支架的制备及其性能研究[D].华南理工大学,2014.[55]Wang Q, Xia Q, Wu Y, et al. 3D-Printed Atsttrin-Incorporated Alginate/Hydroxyapatite Scaffold Promotes Bone Defect Regeneration with TNF/TNFR Signaling Involvement. Adv Healthc Mater. 2015;4(11):1701-1708. [56]Seitz H, Rieder W, Irsen S, et al. Three-dimensional printing of porous ceramic scaffolds for bone tissue engineering. J Biomed Mater Res B Appl Biomater. 2005;74(2):782-788.[57]Warnke PH, Seitz H, Warnke F, et al. Ceramic scaffolds produced by computer-assisted 3D printing and sintering: characterization and biocompatibility investigations. J Biomed Mater Res B Appl Biomater. 2010;93(1):212-217. [58]Inzana JA, Olvera D, Fuller SM, et al. 3D printing of composite calcium phosphate and collagen scaffolds for bone regeneration. Biomaterials. 2014;35(13):4026-4034. [59]丁冉,吴志宏,邱贵兴,等.选择性激光烧结技术的多孔钛合金支架的骨组织工程学观察[J].中华医学杂志, 2014,94(19):1499-1502.[60]朱明兵.基于选择性激光烧结仿生人工骨的研究[D].陕西科技大学,2011.[61]Lin KF, He S, Song Y, et al. Low-Temperature Additive Manufacturing of Biomimic Three-Dimensional Hydroxyapatite/Collagen Scaffolds for Bone Regeneration. ACS Appl Mater Interfaces. 2016;8(11):6905-6916.[62]Pilipchuk SP, Monje A, Jiao Y, et al. Integration of 3D Printed and Micropatterned Polycaprolactone Scaffolds for Guidance of Oriented Collagenous Tissue Formation In Vivo. Adv Healthc Mater. 2016r;5(6):676-687. [63]Reed S, Lau G, Delattre B, et al. Macro- and micro-designed chitosan-alginate scaffold architecture by three-dimensional printing and directional freezing. Biofabrication. 2016;8(1): 015003. [64]Reichert JC, Epari DR, Wullschleger ME, et al. Establishment of a preclinical ovine model for tibial segmental bone defect repair by applying bone tissue engineering strategies. Tissue Eng Part B Rev. 2010;16(1):93-104.[65]Bakker AD, Schrooten J, van Cleynenbreugel T, et al. Quantitative screening of engineered implants in a long bone defect model in rabbits. Tissue Eng Part C Methods. 2008; 14(3):251-260. |
| [1] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [2] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [3] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [4] | He Yunying, Li Lingjie, Zhang Shuqi, Li Yuzhou, Yang Sheng, Ji Ping. Method of constructing cell spheroids based on agarose and polyacrylic molds [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 553-559. |
| [5] | He Guanyu, Xu Baoshan, Du Lilong, Zhang Tongxing, Huo Zhenxin, Shen Li. Biomimetic orientated microchannel annulus fibrosus scaffold constructed by silk fibroin [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 560-566. |
| [6] | Yang Feng, Zhao Qian, Zhang Shixuan, Zhao Tienan, Feng Bo. Effectiveness and safety of rapamycin combined with CD133 antibody stent in preventing vascular restenosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 579-584. |
| [7] | Chen Xiaoxu, Luo Yaxin, Bi Haoran, Yang Kun. Preparation and application of acellular scaffold in tissue engineering and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 591-596. |
| [8] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [9] | Shen Jiahua, Fu Yong. Application of graphene-based nanomaterials in stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 604-609. |
| [10] | Zhang Tong, Cai Jinchi, Yuan Zhifa, Zhao Haiyan, Han Xingwen, Wang Wenji. Hyaluronic acid-based composite hydrogel in cartilage injury caused by osteoarthritis: application and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 617-625. |
| [11] | Li Hui, Chen Lianglong. Application and characteristics of bone graft materials in the treatment of spinal tuberculosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 626-630. |
| [12] | Gao Cangjian, Yang Zhen, Liu Shuyun, Li Hao, Fu Liwei, Zhao Tianyuan, Chen Wei, Liao Zhiyao, Li Pinxue, Sui Xiang, Guo Quanyi. Electrospinning for rotator cuff repair [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 637-642. |
| [13] | Guan Jian, Jia Yanfei, Zhang Baoxin , Zhao Guozhong. Application of 4D bioprinting in tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 446-455. |
| [14] | Liu Jiali, Suo Hairui, Yang Han, Wang Ling, Xu Mingen. Influence of lay-down angles on mechanical properties of three-dimensional printed polycaprolactone scaffolds [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2612-2617. |
| [15] | Huang Bo, Chen Mingxue, Peng Liqing, Luo Xujiang, Li Huo, Wang Hao, Tian Qinyu, Lu Xiaobo, Liu Shuyun, Guo Quanyi . Fabrication and biocompatibility of injectable gelatin-methacryloyl/cartilage-derived matrix particles composite hydrogel scaffold [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2600-2606. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||