| [1]李川云.改变不良生活方式对心血管疾病的防治作用[J].中国医药指南,2009,7(2):33-34.
[2]颜芳,蔡乐,陶杰,等.心血管疾病经济负担的研究现状及问题[J].中国慢性病预防与控制, 2009,17(5):547-549.
[3]孟凡涛,王超.改革开放以来我国青少年体质健康问题的回顾展望[J].体育成人教育学刊, 2010,26(2):28-31.
[4]胡大一.WCC/ESC 2006会议主题:心血管疾病和人口老龄化[J].中国心血管病研究杂志, 2006,4(10):721-723.
[5]朱宁.老年心血管疾病患者合并焦虑抑郁的现状及处理[J].医学与哲学(B), 2012,33(6):17-19.
[6]史振宇,王玉琦,赵静.从一个教学医院分析血管疾病的现状[J].中国临床医学,2002,9(5):585-586.
[7]陈忠,吴庆华,唐小斌,等.腋-腋动脉人工血管转流术在血管外科疾病53例中的应用[J].中华普通外科杂志, 2002, 17(1):15-16.
[8]Ricco JB,Cau J,Marchand C,等.支架人工血管修复治疗胸主动脉疾病:1999—2001年间法国全国性独立研究的结果[J].世界核心医学期刊文摘(心脏病学分册), 2006, 2(5):60-61.
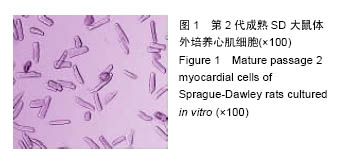
[9]王腾,唐其柱,甘文云,等.大鼠心肌细胞的分离技术和电生理鉴定[J].科技导报, 2009,27(3):80-82.
[10]范治斌,杜森,谷文峰,等.大鼠心肌细胞分离纯化方法的改良[J].上海畜牧兽医通讯, 2009,54(2):44-45.
[11]关欣,李应东,马海彦,等.新生大鼠心肌细胞原代培养分离方法的改进[J].中西医结合心脑血管病杂志, 2009,7(1): 54-55.
[12]姜大春,何国祥,刘建平,等.新生SD大鼠心肌细胞分离培养的快速简单方法及鉴定[J].西南国防医药, 2009,19(4): 390-392.
[13]李少彬,闫玉生,李辉,等.等离子体磺酸化丝素蛋白膜聚四氟乙烯复合小口径人工血管的制备[J].中国组织工程研究与临床康复,2010,14(8):1357-1360.
[14]马艳,岳秀丽,刘萌,等.肝素/聚乙烯醇凝胶灌注修饰的小口径膨体聚四氟乙烯人工血管(英文)[J].中国组织工程研究与临床康复,2008,12(14):2773-2776.
[15]廖月,郭金英,廖洁.聚四氟乙烯人造血管动静脉内瘘术后并发症的护理[J].现代临床护理, 2011,10(8):44-45.
[16]Albanese A,Barbucci R,Belleville J,et al.In vitro biocompatibility evaluation of a heparinizable material (PUPA), based on polyurethane and poly(amido-amine) components.Biomaterials.1994;15(2):129-136.
[17]李少彬,闫玉生,李辉,等.等离子体磺酸化丝素蛋白膜聚四氟乙烯复合小口径人工血管体外的实验研究[J].南方医科大学学报,2010,30(9):2100-2103.
[18]陈胜杰.壳寡糖—细菌纤维素的制备及体外生物相容性评价[D].海南大学,2012.
[19]杨健,田丰,陈世谦,等.壳聚糖结构对凝血作用的研究[J].医疗卫生装备, 2003,24(S1):110-112.
[20]鲁险锋,高扬,赵国梁,等.纳米粉体改性聚酯抗凝血性能的研究: 2004年中国纳米技术应用研讨会[C].中国北京, 2004.
[21]伏鹏.钛合金/聚氨酯涂层的构建及生物相容性研究[D].华中科技大学,2011.
[22]李媛,王小慧,庄远,等.不同表面化学修饰金纳米棒的血液相容性[J].国际药学研究杂志, 2013,40(2):228-232.
[23]杨朝竣,张韻慧,冯靖,等.枫香叶挥发油抗炎及其凝血作用以及化学成分的研究[J].食品工业科技, 2013,35(4): 76-79.
[24]李辉,陈群清,李少彬,等.改良小口径人工血管的血液相容性研究[J].中国医学创新, 2013,6(15):10-12.
[25]缐萍.几种抗凝血化合物的合成及抗凝血机理的研究[D].西北师范大学,2011.
[26]佃少娜,伍善广,李桃,等.肺靶向红霉素明胶微球的安全性评价[J].中国药房,2008,19(4):261-263.
[27]薛金玉,杨杏芬,杨颖,等.红细胞溶血实验替代兔眼刺激性实验检测农药眼刺激性初步研究[J].中国职业医学, 2010, 37(6):469-471.
[28]毛志刚,陈朝辉,韩宏光.人工血管材料生物相容性和血液相容性的研究与分析[J].中国组织工程研究, 2012, 16(16): 2981-2988.
[29]都姣娇,苏红宁,齐淑静.附子主要成分对大鼠心肌细胞的毒性分析[J].首都食品与医药, 2015,22(24):93-94.
[30]罗佳.化学性缺氧对原代培养大鼠心肌细胞葡萄糖转运蛋白的影响[D].中国医科大学, 2007.
[31]胡淑婷.慢性心衰大鼠心肌细胞钙调控异常及药物干预的研究[D].第二军医大学,2011.
[32]陈冲,焦宁,靖景艳,等.台盼蓝拒染法、MTT法、CCK-8法在研究As_2O_3细胞毒性作用中的意义[J].中国医药导报,2013,10(12):24-26.
[33]支添添,周舟,韩成云,等.台盼蓝染色鉴定拟南芥sdl1突变体的细胞死亡[J].作物研究, 2013,27(3):217-218.
[34]马强,丁银娣,曲迪,等.伊红、台盼蓝检测河蟹精子存活率的比较[J].动物学杂志, 2007,42(4):65-69.
[35]施小凤,傅晋翔,朱彦,等.乳酸脱氢酶、羟丁酸脱氢酶检测在巨幼细胞性贫血诊治中的意义[J].苏州大学学报(医学版),2009,29(6):1179-1181.
[36]孙景春,艾清,张玲,等.乳酸脱氢酶同工酶1(LD1)在诊断儿童心肌细胞损伤中的应用[J].中国实验诊断学, 2009, 13(1):81-82.
[37]洪庆涛,宋岳涛,唐一鹏,等. 细胞培养液乳酸脱氢酶漏出率的比色测定及其应用[J].细胞生物学杂志, 2004,26(1): 89-92. |