Chinese Journal of Tissue Engineering Research ›› 2016, Vol. 20 ›› Issue (43): 6521-6529.doi: 10.3969/j.issn.2095-4344.2016.43.020
Previous Articles Next Articles
Autogeneic iliac crest graft versus bone morphogenetic protein 2 in lumbar fusion: a Meta-analysis
- Department of Orthopedics, the Fourth Affiliated Hospital of China Medical University, Shenyang 110032, Liaoning Province, China
-
Received:2016-08-04Online:2016-10-21Published:2016-10-21 -
Contact:Zhang Zhi-yu, M.D., Associate chief physician, Associate professor, Department of Orthopedics, the Fourth Affiliated Hospital of China Medical University, Shenyang 110032, Liaoning Province, China -
About author:Zhang Hai-fei, Master, Attending physician, Department of Orthopedics, the Fourth Affiliated Hospital of China Medical University, Shenyang 110032, Liaoning Province, China
CLC Number:
Cite this article
Zhang Hai-fei, Zhang Zhi-yu, Cui Yan, Wang Feng, Ma Cheng-bin, Zhang Wei.
share this article
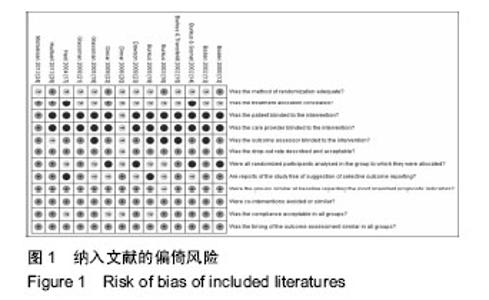
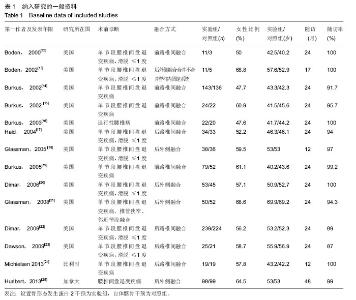
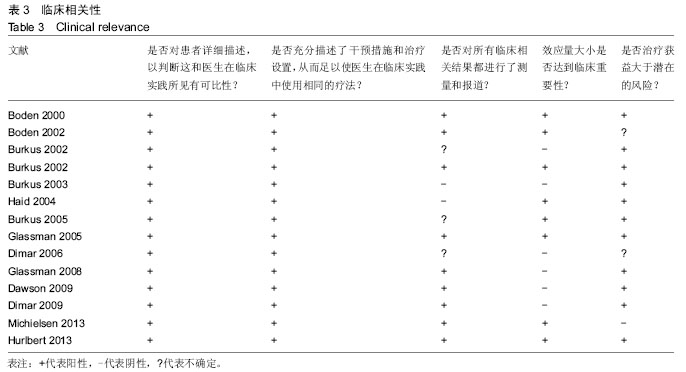
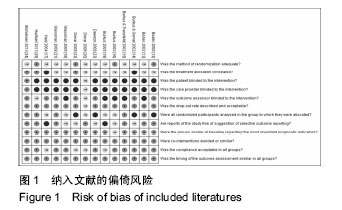
2.2 纳入研究的方法学质量 方法学质量评价的结果见图1。在纳入的14项研究中,有9项满足低偏倚风险标准[12-15,21-25];4项研究满足充分的随机化方法[12,16,22,25],只有2项研究同时具备充分的随机和分配隐藏[22,25];7项研究是否充分随机和分配隐藏不清[13,15,18-20,21,23]。因为手术性质决定各研究对患者或手术者进行盲法不太可能实现,所以只有7项研究对评价融合结果的研究者进行了盲法[12,14,17,21-24];而1项研究,为了减少手术干预不同所带来的潜在偏倚,直到手术进行到需要移植物时才公布随机方案,所以这项研究被认为对干预者进行了盲法[24]。 大多数研究提供了对退出或失访的充分描述,以及能够达到随访结局测量的最低标准,而在这些研究中只有Burkus等[19]的研究进行长期随访。 虽然进行了全面的检索,但依然无法获得各研究已出版或注册的计划书。在这些情况下,很难判断是否存在临床结果的报告偏倚。但7个研究报告了所有4个主要结果(融合率、临床结果、并发症和再手术率),被认为已达到了这个标准[12-13,15,20-21,24-25]。"
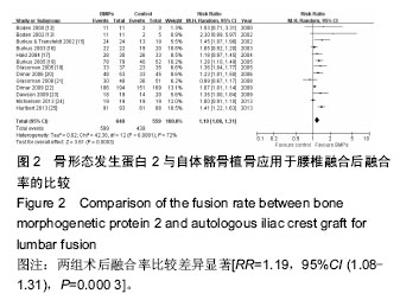
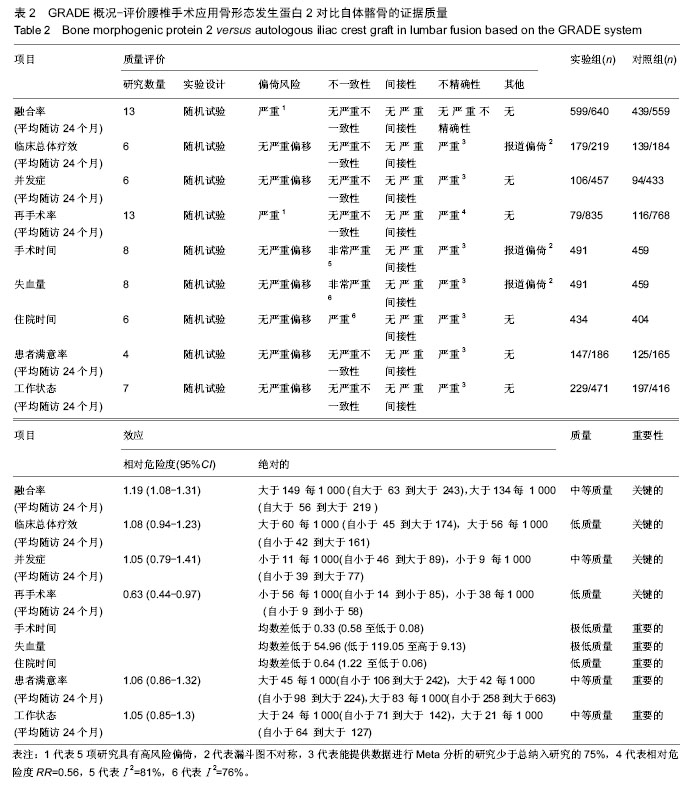
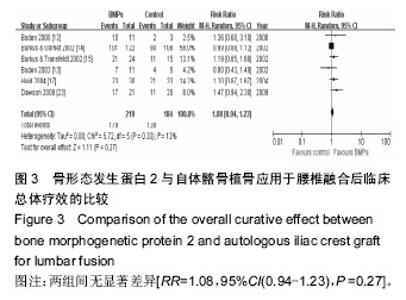
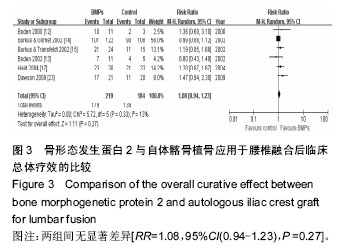
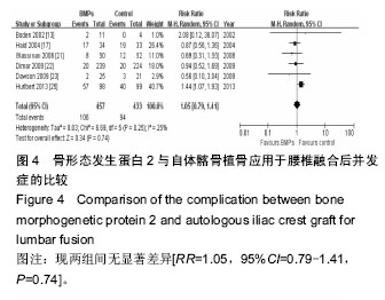
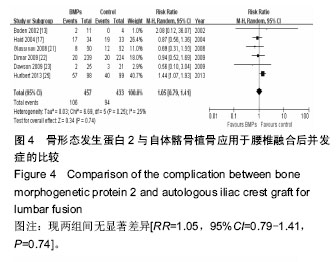
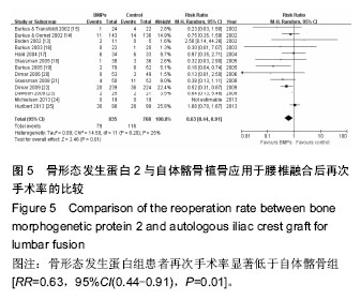
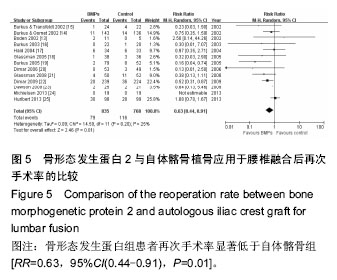
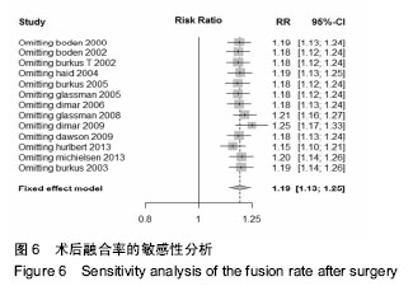
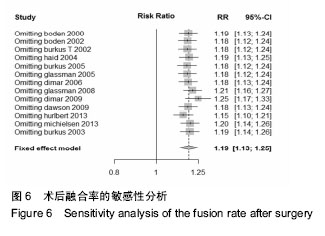
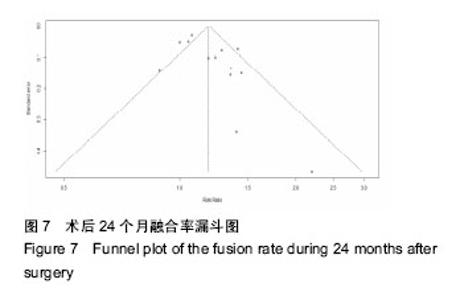
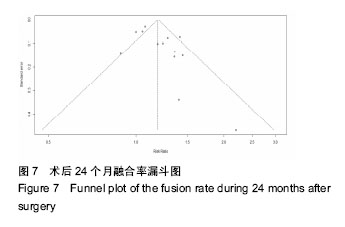
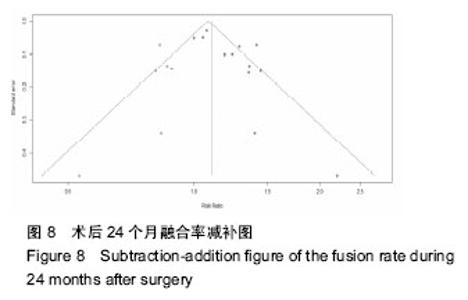
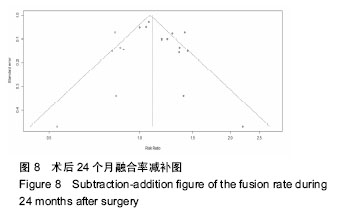
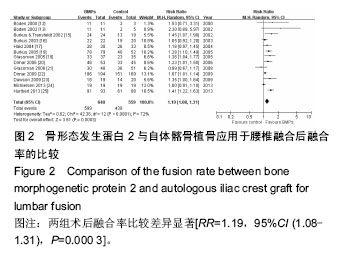
2.4 定量数据的Meta分析 13项研究比较了两组术后融合率(实验组599例患者,对照组439例)[12-13,15-25],组间差异显著[RR=1.19,95%CI(1.08-1.31),P=0.000 3],但研究间存在明显异质性(Ⅰ2=72%),见图2。6项研究提供了关于临床总体疗效的数据(实验组219例,对照组184例)[12-15,17,23],Meta分析发现两组间无显著差异[RR=1.08,95%CI(0.94-1.23),P=0.27],且各组没有异质性(Ⅰ2=13%),见图3。关于并发症,合并了6项研究的数据,包括实验组457例及对照组433例患者,结果显示两组并没有显著差异[RR=1.05,95%CI=0.79-1.41,P=0.74],且各组没有异质性(Ⅰ2=25%),见图4。13项研究比较了两组的再次手术率[13-25],共包括实验组835例及对照组768例患者,结果显示,实验组患者再次手术率显著低于对照组[RR=0.63,95%CI(0.44-0.91),P=0.01], 且各组没有异质性(Ⅰ2=25%),见图5。8项研究比较了两组手术时间[12-13,18,21-25],结果显示,实验组手术时间短于对照组[MD=-0.33,95%CI(-0.58,-0.08),P=0.009], 但各研究间异质性较大(Ⅰ2 = 81%)。而且这8项研究也比较了两组术中出血量,但结果表明在术中出血量上两组并没有显著差别[MD=-54.96,95%CI(119.05,9.13),P=0.09], 各组异质性依然较大(Ⅰ2=76%)。6项研究比较了两组平均住院日[12-13,21-23,25],结果无差异[MD=-0.64,95%CI(-1.12,-0.06),P =0.03],但各组间异质性较大(Ⅰ2 =76%)。4项研究比较了两组术后患者满意度[13-15,17],分析结果显示无统计学差异[RR=1.06,95%CI(0.86,1.32),P=0.58],各组间存在轻度异质性(Ⅰ2 =44%)。7项研究比较了两组术后24个月时患者的工作状态[12,14-15,17,20,22-23],结果显示两组无统计学差异(RR=1.05,95%CI(0.85,1.30),P =0.63)。组间存在轻度异质性(Ⅰ2=38%)。"
| [1]Arrington ED,Smith WJ,Chambers HG,et al. Complications of iliac crest bone graft harvesting.Clin Orthop Relat Res.1996;329:300-309.
[2]Urist MR.Bone Formation by autoinduction. Science. 1965;150:893-899.
[3]Celeste AJ,Iannazzi JA,Taylor RC,et al.Identification of transforming growth factor beta family members present in bone-inductive protein purified from bovine bone.Proc Natl Acad Sci USA. 1990;87: 9843-9847.
[4]Furlan AD,Pennick V,Bombardier C,et al.2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group.Spine (Phila Pa 1976). 2009;34:1929-1941.
[5]Higgins JPT,Green S.Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0[updated March 2011].The Cochrane Collaboration.2011.
[6]DerSimonian R,Laird N. Meta-analysis in clinical trials. Control Clin Trials.1986;7:177-188.
[7]Egger M,Smith GD,Schneider M,et al.Bias in meta-analysis detected by a simple, graphical test. BMJ.1997;315(7109):629-634.
[8]Begg CB,Mazumdar M.Operating characteristics of a rank correlation test for publication bias.Biometrics. 1994;50(4):1088-1101.
[9]Egger M,Smith GD.Bias in location and selection of studies.BMJ.1998;316:61-66.
[10]Duval S,Tweedie R.Trim and fill: a simple funnel-plot based method of testing and adjusting for publication bias in meta-analysis.Biometrics. 2000;56(2): 455-463.
[11]Sutton AJ,Duval SJ,Tweedie RL,et al.Empirical assessment of effect of publication bias on meta-analyses.BMJ.2000;320(7249):1574-1577.
[12]Boden SD,Zdeblick TA,Sandhu HS,et al.The use of rhBMP-2 in interbody fusion cages. Definitive evidence of osteoinduction in humans: a preliminary report. Spine(Phila Pa 1976).2000;25(3):376-381.
[13]Boden SD,Kang J,Sandhu H,et al.Use of recombinant human bone morphogenetic protein-2 to achieve posterolateral lumbar spine fusion in humans: a prospective, randomized clinical pilot trial:2002 Volvo Award in clinical studies.Spine(Phila Pa 1976). 2002; 27(23):2662-2673.
[14]Burkus JK,Gornet MF,Dickman CA,et al.Anterior lumbar interbody fusion using rhBMP-2 with tapered interbody cages.J Spinal Disord Tech. 2002;15:337-349.
[15]Burkus JK,Transfeldt EE,Kitchel SH,et al.Clinical and radiographic outcomes of anterior lumbar interbody fusion using recombinant human bone morphogenetic protein-2.Spine(Phila Pa 1976). 2002;27:2396-2408.
[16]Burkus JK,Dorchak JD,Sanders DL.Radiographic assessment of interbody fusion using recombinant human bone morphogenetic protein type 2.Spine(Phila Pa 1976).2003;28:372-377.
[17]Haid RW Jr,Branch CL Jr,Alexander JT,et al.Posterior lumbar interbody fusion using recombinant human bone morphogenetic protein type 2 with cylindrical interbody cages.Spine J.2004;4(5):527-538.
[18]Glassman SD,Dimar JR,Carreon LY,et al.Initial fusion rates with recombinant human bone morphogenetic protein-2/compression resistant matrix and a hydroxyapatite and tricalcium phosphate/collagen carrier in posterolateral spinal fusion.Spine(Phila Pa 1976).2005;30(15):1694-1698.
[19]Burkus JK,Sandhu HS,Gornet MF,et al.Use of rhBMP-2 in combination with structural cortical allografts: clinical and radiographic outcomes in anterior lumbar spinal surgery.J Bone Joint Surg Am. 2006;87(6):1205-1212.
[20]Dimar JR,Glassman SD,Burkus KJ,et al.Clinical outcomes and fusion success at 2 years of single-level instrumented posterolateral fusions with recombinant human bone morphogenetic protein-2/compression resistant matrix versus iliac crest bone graft.Spine (Phila Pa 1976).2006;31(22):2534-2539.
[21]Glassman SD,Carreon LY,Djurasovic M,et al. RhBMP-2 versus iliac crest bone graft for lumbar spine fusion: a randomized, controlled trial in patients over 60 years of age.Spine(Phila Pa 1976). 2008;33(26):2843-2849.
[22]Dimar JR 2nd,Glassman SD,Burkus JK,et al.Clinical and radiographic analysis of an optimized rhBMP-2 formulation as an autograft replacement in posterolateral lumbar spine arthrodesis.J Bone Joint Surg Am.2009;91(6):1377-1386.
[23]Dawson E,Bae HW,Burkus JK,et al.Recombinant human bone morphogenetic protein-2 on an absorbable collagen sponge with an osteoconductive bulking agent in posterolateral arthrodesis with instrumentation.A prospective randomized trial.J Bone Joint Surg Am.2009;91(7):1604-1613.
[24]Michielsen J,Sys J,Rigaux A,et al.The effect of recombinant human bone morphogenetic protein-2 in single-level posteriorlumbar interbody arthrodesis.J Bone Joint Surg Am.2013;95(10):873-880.
[25]Hurlbert RJ,Alexander D,Bailey S,et al.rhBMP-2 for posterolateral instrumented lumbar fusion: a multicenter prospective randomized controlled trial. Spine(Phila Pa 1976).2013;38:2139-2148.
[26]An H,Boden SD,Kang J,et al.Summary statement: emerging techniques for treatment of degenerative lumbar disc disease. Spine(Phila Pa 1976).2003;28(15 Suppl):S24-S25.
[27]Poynton AR,Lane JM.Safety profile for the clinical use of bone morphogenetic proteins in the spine. Spine (Phila Pa 1976).2002;27:S40-48.
[28]Benglis D,Wang MY,Levi AD.A comprehensive review of the safety profile of bone morphogenetic protein in spine surgery.Neurosurgery.2008;62(5 Suppl 2): ONS423-431.
[29]Carragee EJ,Hurwitz EL,Weiner BK.A critical review of recombinant human bone morphogenetic protein-2 trials in spinal surgery: emerging safety concerns and lessons learned.Spine J.2011;11(6):471-491.
[30]Mussano F,Ciccone G,Ceccarelli M,et al.Bone morphogenetic proteins and bone defects: a systematic review.Spine(Phila Pa 1976). 2007;32:824-830.
[31]Papakostidis C,Kontakis G,Bhandari M,et al.Efficacy of autologous iliac crest bone graft and bone morphogenetic proteins for posterolateral fusion of lumbar spine: a meta-analysis of the results. Spine(Phila Pa 1976). 2008;33(19):E680-692.
[32]Agarwal R,Williams K,Umscheid CA,et al. Osteoinductive bone graft substitutes for lumbar fusion: a systematic review.J Neurosurg Spine.2009; 11(11): 729-740.
[33]Donell S,Garrison K,Shemilt I,et al.Bone Morphogenetic Protein-2 for Spinal Fusion: Meta-analysis of Randomised Controlled Trials.UEA Website. Available:http://www.uea.ac.uk/~wo158 /BMP-2%20for%20SF%20-%20Meta-analysis%20of%20RCTs.pdf. Accessed Dec 12,2013.
[34]Blumenthal SL,Gill K.Can lumbar spine radiographs accurately determine fusion in postoperative patients? Correlation of routine radiographs with a second surgical look at lumbar fusions.Spine(Phila Pa 1976). 1993;18(9):1186-1189.
[35]Mroz TE,Wang JC,Hashimoto R,et al.Complications related to osteobiologics use in spine surgery: a systematic review.Spine(Phila Pa 1976). 2010;35(20): S86-104.
[36]Fu R,Selph S,McDonagh M,et al.Effectiveness and harms of recombinant human bone morphogenetic protein-2 in spine fusion: a systematic review and meta-analysis.Ann Intern Med.2013;158(12):890-902.
[37]Simmonds MC,Brown JV,Heirs MK,et al.Safety and effectiveness of recombinant human bone morphogenetic protein-2 for spinal fusion: a meta-analysis of individual-participant data.Ann Intern Med.2013;158(12):877-889.
[38]Carragee EJ,Hurwitz EL,Weiner BK.A critical review of recombinant human bone morphogenetic protein-2 trials in spinal surgery: emerging safety concerns and lessons learned.Spine J.2011;11: 471-491.
[39]Yale School of Medicine. Available: http://medicine.yale.edu/core/projects/yodap/datasharing/ medtronic/463_158787_YorkrhBMP2FinalReport. pdf.Accessed Dec 12,2013. |
| [1] | Zhan Fangbiao, Cheng Jun, Zou Xinsen, Long Jie, Xie Lizhong, Deng Qianrong. Intraoperative intravenous application of tranexamic acid reduces perioperative bleeding in multilevel posterior spinal surgery: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 977-984. |
| [2] | Li Yanle, Yue Xiaohua, Wang Pei, Nie Weizhi, Zhang Junwei, Tan Yonghai, Jiang Hongjiang. Intramedullary nail fixation versus plate fixation in the treatment of displaced midshaft clavicular fractures in adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 471-476. |
| [3] | Tang Xiaokai, Li Weiming. Role and mechanism of Nel-like molecule-1 in promoting bone fusion after spinal fusion [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3914-3920. |
| [4] | Yang Wei, Chen Zehua, Yi Zhiyong, Huang Xudong, Han Qingmin, Zhang Ronghua. Effectiveness of intra-articular injection of hyaluronic acid versus placebo in the treatment of early and mid-stage knee osteoarthritis: a Meta-analysis based on randomized, double-blind, controlled, clinical trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(23): 3760-3766. |
| [5] | Wang Yanjiao, Wang Rui, Sun Luning. Bankart pepair versus Bristow-Latarjet procedure for recurrent anterior instability of the shoulder: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3423-3430. |
| [6] | Xu Hui, Kang Bingxin, Zhong Sheng, Gao Chenxin, Zhao Chi, Qiu Guowei, Sun Songtao, Xie Jun, Xiao Lianbo, Shi Qi. Pressing local acupoints plus adjustion of the knee joint in a sitting position for treating knee osteoarthritis: a randomized controlled trial [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(2): 216-221. |
| [7] | Xia Wenshen, He Renjiao, Ai Jinwei, Wang Jun, Li Desheng, Pei Bin. Stem cell transplantation for diabetic patients with lower-extremity arterial disease: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 3110-3116. |
| [8] | Zhong Yuanming, Fu Xiaopeng, Xu Wei, Zhao Qingrui, Huang Yong, Ye Weiquan. Nicardipine controlled hypotension applied to perioperative blood loss in orthopedics: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2930-2937. |
| [9] | Yin Yuhui, Zhan Jiawen, Wang Shangquan, Shao Chenchen, Zhou Liang. Meta-analysis of acupuncture combined with massage in the treatment of knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(17): 2719-2726. |
| [10] | Chen Jiang, Li Jinyu, Zheng Chenying, Bai Chunxiao, Zhang Fan, Liu Chuyin, Zhao Xueqian, Yuan Qiaomei, Di Xueshi, Kang Shengqian, Jia Yusong . Changes in sagittal parameters of cervical spine after double-segment artificial cervical disc replacement and anterior cervical discectomy and fusion [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(15): 2341-2346. |
| [11] | Song Min, Lu Chao, Chen Jin, Wu Gaoyi, Li Congcong, Li Anan, Ye Guozhu, Lin Wenzheng, Cai Yuning, Liu Wengang, Xu Weipeng. Application of tourniquet affects thickness of bone cement penetration in total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1917-1923. |
| [12] | Wang Xin, Lin Xiaodong, Liu Hongliang, Huang Zexin, Xu Shuchai, Chen Bojian. Fixed-bearing prosthesis versus mobile-bearing prosthesis during total knee arthroplasty for different follow-up periods: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1924-1929. |
| [13] | Huang Yong, Zhu Weimin, Lu Wei, Ouyang Kan, Peng Liangquan, Liu Haifeng, Li Hao, Feng Wenzhe, Xu Jian, Zhong Mingjin, Chen Kang, Li Ying, Deng Zhenhan. Safety of steroid-containing cocktail periarticular injection after knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(9): 1449-1456. |
| [14] | Deng Jinman, Fang Guanjun, Wang Yu, Ding Shaobo. Efficacy and characteristics of parecoxib and celecoxib in the treatment of pain after orthopedic surgery: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(9): 1471-1476. |
| [15] | Liu Yongpan, Gong Xiaofang. Effects of dexmedetomidine on perioperative brain protection in patients undergoing craniocerebral surgery under inhalation anesthesia with sevoflurane: a randomized controlled study [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(35): 5688-5694. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||