Chinese Journal of Tissue Engineering Research ›› 2016, Vol. 20 ›› Issue (1): 70-77.doi: 10.3969/j.issn.2095-4344.2016.01.013
Previous Articles Next Articles
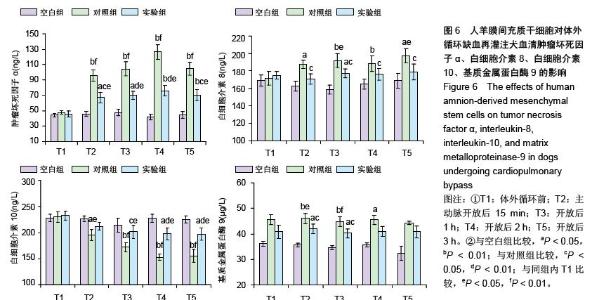
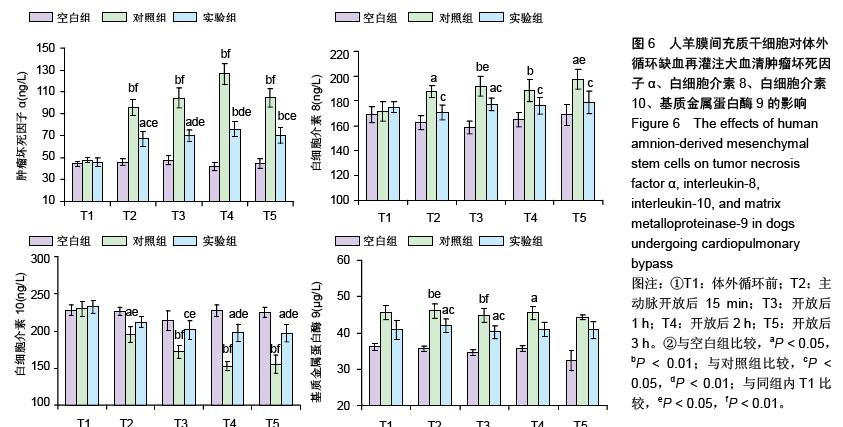
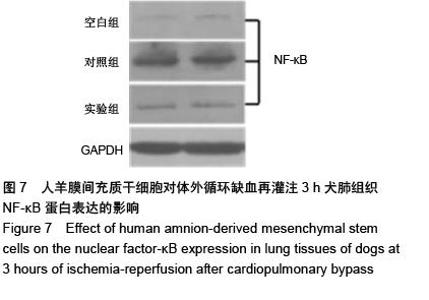
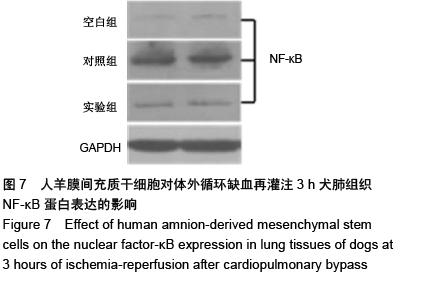
Transplantation of human amnion-derived mesenchymal stem cells alleviates ischemia-reperfusion-induced acute lung injury after cardiopulmonary bypass
Qiang Yong1, Liang Gui-you2, Yu Li-mei3, Qi Bin3, Gao Zhen-yu4
- 1Department of Cardiothoracic Surgery, Nanjing General Hospital of Nanjing Military Command, Nanjing 210002, Jiangsu Province, China; 2Department of Cardiothoracic Surgery, Affiliated Hospital of Zunyi Medical University, Zunyi 563000, Guizhou Province, China; 3Key Laboratory of Cell Engineering in Guizhou Province, Affiliated Hospital of Zunyi Medical University, Zunyi 563000, Guizhou Province, China; 4Surgical Animal Experiment Center, Zunyi Medical University, Zunyi 563000, Guizhou Province, China
-
Received:2015-11-15Online:2016-01-01Published:2016-01-01 -
Contact:Liang Gui-you, M.D., Professor, Master’s supervisor, Department of Cardiothoracic Surgery, Affiliated Hospital of Zunyi Medical University, Zunyi 563000, Guizhou Province, China -
About author:Qiang Yong, Master, Attending physician, Department of Cardiothoracic Surgery, Nanjing General Hospital of Nanjing Military Command, Nanjing 210002, Jiangsu Province, China -
Supported by:the Scientific Tackle Key Project of Guizhou Province, No. [2014]3022; the Scientific Tackle Key Project of Zunyi City, No. [2013]38
CLC Number:
Cite this article
Qiang Yong, Liang Gui-you, Yu Li-mei, Qi Bin, Gao Zhen-yu. Transplantation of human amnion-derived mesenchymal stem cells alleviates ischemia-reperfusion-induced acute lung injury after cardiopulmonary bypass[J]. Chinese Journal of Tissue Engineering Research, 2016, 20(1): 70-77.
share this article
| [1] Sevuk U, Cakil N, Altindag R, et al. Relationship between nadir hematocrit during cardiopulmonary bypass and postoperative hyperglycemia in nondiabetic patients. Heart Surg Forum. 2014;17(6):E302-307.
[2] Engels M, Bilgic E, Pinto A, et al. A cardiopulmonary bypass with deep hypothermic circulatory arrest rat model for the investigation of the systemic inflammation response and induced organ damage. J Inflamm (Lond). 2014;11:26.
[3] Ranucci M, Isgrò G, Carlucci C, et al. Central venous oxygen saturation and blood lactate levels during cardiopulmonary bypass are associated with outcome after pediatric cardiac surgery. Crit Care. 2010;14(4):R149.
[4] Chen H, Cheng ZB, Yu RG. Procalcitonin as a predictor of moderate to severe acute respiratory distress syndrome after cardiac surgery with cardiopulmonary bypass: a study protocol for a prospective cohort study. BMJ Open. 2014; 4(10):e006344.
[5] Nakamura H, Yamaguchi H, Amano A, et al. Venovenous extracorporeal membrane oxygenation is effective against post-cardiotomy acute respiratory failure in adults. Gen Thorac Cardiovasc Surg. 2013;61(7):402-408.
[6] Cheng C, Li S, Wang Y, et al. Ischemic postconditioning alleviates lung injury and maintains a better expression of aquaporin-1 during cardiopulmonary bypass.Chin Med J (Engl). 2014;127(23):4012-4018.
[7] Dolkart O, E A, S S, et al. Temporal determination of lung NO system and COX-2 upregulation following ischemia-reperfusion injury. Exp Lung Res. 2014;40(1):22-29.
[8] Gu YJ, Boonstra PW, Graaff R, et al. Pressure drop, shear stress, and activation of leukocytes during cardiopulmonary bypass: a comparison between hollow fiber and flat sheet membrane oxygenators.Artif Organs. 2000;24(1):43-48.
[9] Banz Y, Rieben R, Zobrist C, et al. Addition of dextran sulfate to blood cardioplegia attenuates reperfusion injury in a porcine model of cardiopulmonary bypass. Eur J Cardiothorac Surg. 2008;34(3):653-660.
[10] Liakopoulos OJ, Schmitto JD, Kazmaier S, et al. Cardiopulmonary and systemic effects of methylprednisolone in patients undergoing cardiac surgery. Ann Thorac Surg. 2007;84(1):110-118.
[11] Warren O, Darzi A, Athanasiou T. What is the role of leukocyte depletion in cardiac surgery.Heart Lung Circ. 2007;16(5): 398-399.
[12] Eisses MJ, Velan T, Aldea GS, et al. Strategies to reduce hemostatic activation during cardiopulmonary bypass. Thromb Res. 2006;117(6):689-703.
[13] Williams GD, Ramamoorthy C, Chu L, et al. Modified and conventional ultrafiltration during pediatric cardiac surgery: clinical outcomes compared. J Thorac Cardiovasc Surg. 2006;132(6):1291-1298.
[14] Manuelpillai U, Moodley Y, Borlongan CV, et al. Amniotic membrane and amniotic cells: potential therapeutic tools to combat tissue inflammation and fibrosis. Placenta. 2011;32 Suppl 4:S320-325.
[15] Chang CJ, Yen ML, Chen YC, et al. Placenta-derived multipotent cells exhibit immunosuppressive properties that are enhanced in the presence of interferon-gamma. Stem Cells. 2006;24(11):2466-2477.
[16] Banas RA, Trumpower C, Bentlejewski C, et al. Immunogenicity and immunomodulatory effects of amnion-derived multipotent progenitor cells. Hum Immunol. 2008;69(6):321-328.
[17] Dominici M, Le Blanc K, Mueller I, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8(4):315-317.
[18] Bailo M, Soncini M, Vertua E, et al. Engraftment potential of human amnion and chorion cells derived from term placenta. Transplantation. 2004;78(10):1439-1448.
[19] 丛姗,白立恒,李岩,等.人羊膜间充质干细胞移植对CCl4诱导的小鼠损伤肝HGF、SIRT-1、α-SMA及P27kip1表达的影响[J].中国生物化学与分子生物学报, 2015, 31(3):292-300.
[20] Zhao P, Ise H, Hongo M, et al. Human amniotic mesenchymal cells have some characteristics of cardiomyocytes. Transplantation. 2005;79(5):528-535.
[21] Kim J, Kang HM, Kim H, et al. Ex vivo characteristics of human amniotic membrane-derived stem cells. Cloning Stem Cells. 2007;9(4):581-594.
[22] Kim J, Lee Y, Kim H, et al. Human amniotic fluid-derived stem cells have characteristics of multipotent stem cells. Cell Prolif. 2007;40(1):75-90.
[23] Han K, Lee JE, Kwon SJ, et al. Human amnion-derived mesenchymal stem cells are a potential source for uterine stem cell therapy. Cell Prolif. 2008;41(5):709-725.
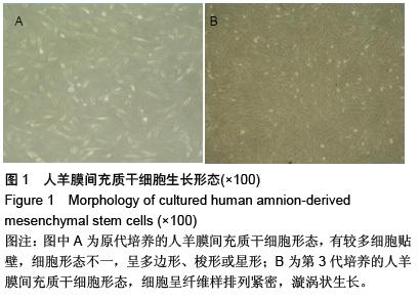
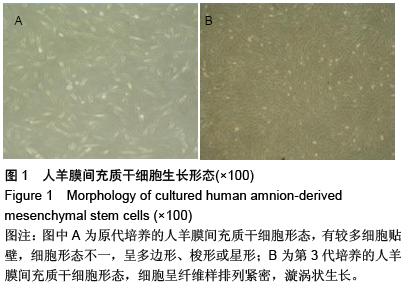
[24] 丛姗,宋瑾,张惠娟,等.人羊膜间充质干细胞(hAMSCs)的分离、体外培养及诱导分化[J]. 农业生物技术学报,2015,23(1): 20-31.
[25] Gibbon JH Jr. Application of a mechanical heart and lung apparatus to cardiac surgery.Minn Med. 1954;37(3): 171-185.
[26] 张贺,王承利,王洋,等.犬体外循环模型建立及麻醉处理[J].中国比较医学杂志,2010,20(10):44-47.
[27] Halter J, Steinberg J, Fink G, et al. Evidence of systemic cytokine release in patients undergoing cardiopulmonary bypass. J Extra Corpor Technol. 2005;37(3):272-277.
[28] Zhou E, Li Y, Wei Z, et al. Schisantherin A protects lipopolysaccharide-induced acute respiratory distress syndrome in mice through inhibiting NF-κB and MAPKs signaling pathways. Int Immunopharmacol. 2014;22(1): 133-140.
[29] Shembade N, Harhaj NS, Liebl DJ, et al. Essential role for TAX1BP1 in the termination of TNF-alpha-, IL-1- and LPS-mediated NF-kappaB and JNK signaling. EMBO J. 2007;26(17):3910-3922.
[30] Karlsson H, Samarasinghe S, Ball LM, et al. Mesenchymal stem cells exert differential effects on alloantigen and virus-specific T-cell responses. Blood. 2008;112(3):532-541.
[31] Miyazawa T, Matsumoto K, Ohmichi H, et al. Protection of hippocampal neurons from ischemia-induced delayed neuronal death by hepatocyte growth factor: a novel neurotrophic factor. J Cereb Blood Flow Metab. 1998;18(4): 345-348.
[32] Matsumoto K, Nakamura T. Hepatocyte growth factor: renotropic role and potential therapeutics for renal diseases. Kidney Int. 2001;59(6):2023-2038.
[33] Sharma HS. Neuroprotective effects of neurotrophins and melanocortins in spinal cord injury: an experimental study in the rat using pharmacological and morphological approaches. Ann N Y Acad Sci. 2005;1053:407-421.
[34] Fares RC, Gomes Jde A, Garzoni LR, et al. Matrix metalloproteinases 2 and 9 are differentially expressed in patients with indeterminate and cardiac clinical forms of Chagas disease. Infect Immun. 2013;81(10):3600-3608.
[35] Välimäki J, Uusitalo H. Matrix metalloproteinases (MMP-1, MMP-2, MMP-3 and MMP-9, and TIMP-1, TIMP-2 and TIMP-3) and markers for vascularization in functioning and non-functioning bleb capsules of glaucoma drainage implants. Acta Ophthalmol. 2015;93(5):450-456.
[36] Toufaily C, Charfi C, Annabi B, et al. A Role for the Cavin-3/Matrix Metalloproteinase-9 Signaling Axis in the Regulation of PMA-Activated Human HT1080 Fibrosarcoma Cell Neoplastic Phenotype. Cancer Growth Metastasis. 2014; 7:43-51.
[37] Petrovska-Cvetkovska D, Dolnenec-Baneva N, Nikodijevik D, et al. Correlative study between serum matrix metalloproteinase 9 values and neurologic deficit in acute, primary, supratentorial, intracerebral haemorrhage. Prilozi. 2014;35(2):39-44.
[38] Wang C, Li D, Qian Y, et al. Increased matrix metalloproteinase-9 activity and mRNA expression in lung injury following cardiopulmonary bypass. Lab Invest. 2012; 92(6):910-916.
[39] Eichler W, Bechtel JF, Schumacher J, et al. A rise of MMP-2 and MMP-9 in bronchoalveolar lavage fluid is associated with acute lung injury after cardiopulmonary bypass in a swine model. Perfusion. 2003;18(2):107-113.
[40] Bours V, Bentires-Alj M, Hellin AC, et al. Nuclear factor-kappa B, cancer, and apoptosis. Biochem Pharmacol. 2000;60(8): 1085-1089.
[41] Xiao W. Advances in NF-kappaB signal ling transduction and transcription. Cell Mol Immunology. 2004;1(6):425-435.
[42] Fei XJ, Zhu LL, Xia LM, et al. Acanthopanax senticosus attenuates inflammation in lipopolysaccharide-induced acute lung injury by inhibiting the NF-κB pathway. Genet Mol Res. 2014;13(4):10537-10544. |
| [1] | Jiang Tao, Ma Lei, Li Zhiqiang, Shou Xi, Duan Mingjun, Wu Shuo, Ma Chuang, Wei Qin. Platelet-derived growth factor BB induces bone marrow mesenchymal stem cells to differentiate into vascular endothelial cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3937-3942. |
| [2] | Chen Yang, Huang Denggao, Gao Yuanhui, Wang Shunlan, Cao Hui, Zheng Linlin, He Haowei, Luo Siqin, Xiao Jingchuan, Zhang Yingai, Zhang Shufang. Low-intensity pulsed ultrasound promotes the proliferation and adhesion of human adipose-derived mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3949-3955. |
| [3] | Zhang Lishu, Liu Anqi, He Xiaoning, Jin Yan, Li Bei, Jin Fang. Alpl gene affects the therapeutic effect of bone marrow mesenchymal stem cells on ulcerative colitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3970-3975. |
| [4] | Ruan Guangping, Yao Xiang, Liu-Gao Miyang, Cai Xuemin, Li Zian, Pang Rongqing, Wang Jinxiang, Pan Xinghua. Umbilical cord mesenchymal stem cell transplantation for traumatic systemic inflammatory response syndrome in tree shrews [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3994-4000. |
| [5] | Mo Jianling, He Shaoru, Feng Bowen, Jian Minqiao, Zhang Xiaohui, Liu Caisheng, Liang Yijing, Liu Yumei, Chen Liang, Zhou Haiyu, Liu Yanhui. Forming prevascularized cell sheets and the expression of angiogenesis-related factors [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3479-3486. |
| [6] | Chen Lei, Zheng Rui, Jie Yongsheng, Qi Hui, Sun Lei, Shu Xiong. In vitro evaluation of adipose-derived stromal vascular fraction combined with osteochondral integrated scaffold [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3487-3492. |
| [7] | Wei Qin, Zhang Xue, Ma Lei, Li Zhiqiang, Shou Xi, Duan Mingjun, Wu Shuo, Jia Qiyu, Ma Chuang. Platelet-derived growth factor-BB induces the differentiation of rat bone marrow mesenchymal stem cells into osteoblasts [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 2953-2957. |
| [8] | Chen Xiao, Guo Zhi, Chen Lina, Liu Xuanyong, Zhang Yihuizhi, Li Xumian, Wang Yueqiao, Wei Liya, Xie Jing, Lin Li. Factors affecting the mobilization and collection of autologous peripheral blood hematopoietic stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 2958-2962. |
| [9] | Guo Zhibin, Wu Chunfang, Liu Zihong, Zhang Yuying, Chi Bojing, Wang Bao, Ma Chao, Zhang Guobin, Tian Faming. Simvastatin stimulates osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 2963-2968. |
| [10] | Li Congcong, Yao Nan, Huang Dane, Song Min, Peng Sha, Li Anan, Lu Chao, Liu Wengang. Identification and chondrogenic differentiation of human infrapatellar fat pad derived stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 2976-2981. |
| [11] | Gao Yuanhui, Xiang Yang, Cao Hui, Wang Shunlan, Zheng Linlin, He Haowei, Zhang Yingai, Zhang Shufang, Huang Denggao. Comparison of biological characteristics of adipose derived mesenchymal stem cells in Wuzhishan inbreed miniature pigs aged two different months [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 2988-2993. |
| [12] | Cao Yang, Zhang Junping, Peng Li, Ding Yi, Li Guanghui. Isolation and culture of rabbit aortic endothelial cells and biological characteristics [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 3000-3003. |
| [13] | Dai Min, Wang Shuai, Zhang Nini, Huang Guilin, Yu Limei, Hu Xiaohua, Yi Jie, Yao Li, Zhang Ligang. Biological characteristics of hypoxic preconditioned human amniotic mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 3004-3008. |
| [14] | Qin Yanchun, Rong Zhen, Jiang Ruiyuan, Fu Bin, Hong Xiaohua, Mo Chunmei. Chinese medicine compound preparation inhibits proliferation of CD133+ liver cancer stem cells and the expression of stemness transcription factors [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 3016-3023. |
| [15] | Dai Yaling, Chen Lewen, He Xiaojun, Lin Huawei, Jia Weiwei, Chen Lidian, Tao Jing, Liu Weilin. Construction of miR-146b overexpression lentiviral vector and the effect on the proliferation of hippocampal neural stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 3024-3030. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||