Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (15): 3897-3905.doi: 10.12307/2026.695
Previous Articles Next Articles
Comparison of Zero-profile self-stabilizing fusion devices and traditional plate fusion systems in treatment of single-level cervical spondylosis
Wang Jianru1, 2, Ma Jikun3, Qi Junjie1, Jiang Zilong1, Sun Yunlong2, Chen Longwei2, Jiang Lianghai2, Wei Jianwei2, Liu Haifei2
- 1School of Clinical Medicine, Shandong Second Medical University, Weifang 261000, Shandong Province, China; 2Department of Spine Surgery, Eastern District of Qingdao Municipal Hospital, Qingdao 266000, Shandong Province, China; 3Department of Spinal Trauma Surgery, Jiaozhou Central Hospital of Qingdao, Qingdao 266000, Shandong Province, China
-
Accepted:2025-06-17Online:2026-05-28Published:2025-11-06 -
Contact:Liu Haifei, MD, Chief physician, Department of Spine Surgery, Eastern District of Qingdao Municipal Hospital, Qingdao 266000, Shandong Province, China -
About author:Wang Jianru, Master candidate, School of Clinical Medicine, Shandong Second Medical University, Weifang 261000, Shandong Province, China; Department of Spine Surgery, Eastern District of Qingdao Municipal Hospital, Qingdao 266000, Shandong Province, China
CLC Number:
Cite this article
Wang Jianru, Ma Jikun, Qi Junjie, Jiang Zilong, Sun Yunlong, Chen Longwei, Jiang Lianghai, Wei Jianwei, Liu Haifei. Comparison of Zero-profile self-stabilizing fusion devices and traditional plate fusion systems in treatment of single-level cervical spondylosis[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(15): 3897-3905.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
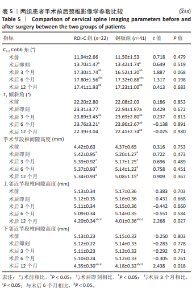
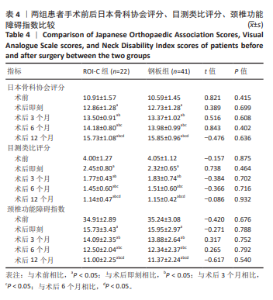
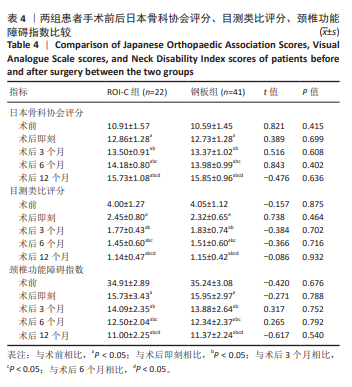
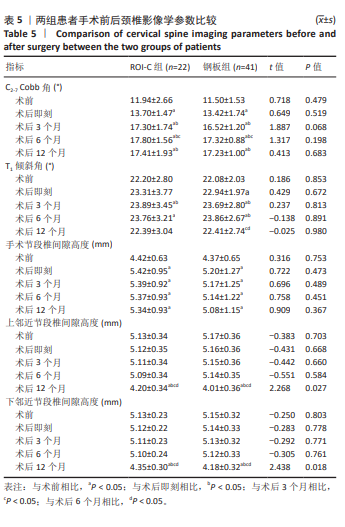
2.6 手术前后影像学评估 两组患者术后C2-7 Cobb角、T1倾斜角,椎间隙高度均较术前显著改善,两组组内不同时间点的C2-7 Cobb角、T1倾斜角,椎间隙高度比较存在显著差异(P < 0.001),而不同分组之间的评分差异无显著性意义(P > 0.05),并且两组在不同时间点的趋势也无显著差异(P > 0.05)。 ROI-C组术后即刻、术后3,6,12个月的C2-7 Cobb角、手术节段椎间隙高度及术后3,6个月的T1倾斜角较术前均显著增加;术后3,6,12个月的C2-7 Cobb角、术后3个月的T1倾斜角均较术后即刻明显增加;术后6个月的C2-7 Cobb角较术后3个月明显增加,差异有显著性意义(P < 0.05)。钢板组术后即刻、术后3,6,12个月的C2-7 Cobb角、手术节段椎间隙高度及术后即刻、术后3,6个月的T1倾斜角均较术前明显增加;与术后即刻相比,钢板组术后3,6,12个月的C2-7 Cobb角及术后3,6个月的T1倾斜角均明显增加;术后6个月的C2-7 Cobb角较术后3个月明显增加,术后12个月的T1倾斜角较术后3个月明显减小;术后12个月的T1倾斜角较术后6个月明显减小,差异有显著性意义(P < 0.05)。见表5。"
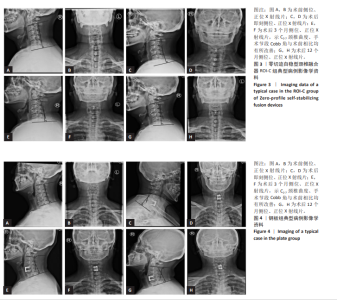
2.7 术后并发症评估 2.7.1 吞咽困难情况分析 在ROI-C组中,术后出现吞咽困难的病患数为4例,占该组总数的18%(4/22),此症状在术后3个月内自行缓解。相比之下,钢板组术后发生吞咽困难的患者较多,共计14例,发生率为34%(14/41);术后3个月时,钢板组内仍有7例(17%)患者持续存在吞咽困难;至术后6个月的随访时,这些患者的吞咽困难症状均得到显著改善或消失。统计结果显示,两组间在术后吞咽困难的发生率上未见显著性差异(χ2=1.788,P=0.181);ROI-C组术后3个月吞咽困难发生率显著低于钢板组(Fisher确切概率法P=0.041)。 2.7.2 邻近节段退变情况分析 ROI-C组与钢板组患者在术后3,6个月的时间点上,均未报告有邻近节段退变发生。术后12个月,ROI-C组中观察到邻近节段退变病例1例,占比5%(1/22);而钢板组内则出现3例邻近节段退变,占比7%(3/41),两组差异无显著性意义(χ2=0.029,P=0.866)。 两组术后12个月的上邻近节段和下邻近节段椎间隙高度均较术后即刻明显降低,但钢板组邻近椎间隙高度下降程度较ROI-C组明显增高,差异有显著性意义(P < 0.05)。两组间术前、术后即刻、术后3,6,12个月的C2-7 Cobb角、T1倾斜角、椎间隙高度相比差异均无显著性意义(P > 0.05)。 2.8 植入物与宿主的生物相容性 术后6个月时,ROI-C组出现1例未融合(5%),钢板组出现1例(2%);术后12个月时两组患者全部获得融合,两组间无明显差异(P < 0.05)。两组术后均未出现植入物周围感染、过敏反应、免疫反应及排斥反应。部分患者(ROI-C组3例、钢板组9例)术后出现体温轻度升高(小于38 ℃),在术后3 d内均得到恢复。术后各时间节点均未发现植入物破损、松动、脱落。 2.9 典型病例 影像学资料见图3,4。"

| 1] LIN T, SHANGGUAN Z, XIAO Z, et al. Whether the potential degree of cervical instability and cervical muscle degeneration in patients with cervical spondylosis radicular affect the efficacy of cervical traction. Sci Rep. 2024;14(1):20467. [2] GERDHEM L, VLACHOGIANNIS P, GERDHEM P, et al. Cage only or cage with plate fixation in anterior cervical discectomy and fusion surgery - analysis of a national multicenter dataset. Spine J. 2025;25(5):947-955. [3] SU XJ, CHEN XY, DAI JF, et al. Hybrid fixation versus conventional cage-plate construct in 3-level ACDF: Introduce the “seesaw theory” of stand-alone cage. Clin Neurol Neurosurg. 2023;233:107941. [4] ZAIDI SE, VENKATRAMAN V, SYKES DAW, et al. Clinical and Radiographic Outcomes for Patients with Cervical Adjacent Segment Disease Treated with Anterior Cervical Discectomy and Fusion with Integrated Interbody Spacers. World Neurosurg. 2023;180:e514-e522. [5] BYDON M, XU R, MACKI M, et al. Adjacent Segment Disease after Anterior Cervical Discectomy and Fusion in a Large Series. Neurosurgery. 2014;74(2):139-146. [6] SONG D, DENG Z, FENG T, et al. The clinical efficacy of anterior cervical discectomy and fusion with ROI-C device vs. plate-cage in managing traumatic central cord syndrome. Front Surg. 2023;9:1055317. [7] WANG Z, ZHU X, WANG Z, et al. Zero-P and ROI-C implants versus traditional titanium plate with cage to treat cervical spondylotic myelopathy: clinical and radiological results with 5 years of follow-up. BMC Musculoskelet Disord. 2023;24(1):539. [8] BICHENG X, JIANGUANG S, SHILEI H, et al. Efficacy comparison of zero profile intervertebral fusion and stand alone interbody cage combined with cage titanium plate construct in treatment of two segment skip cervical spondylosis. Zhonghua Yi Xue Za Zhi. 2022;102(19):1450-1457. [9] 李玉伟, 王海蛟, 严晓云, 等. 颈前路减压零切迹椎间融合器与钉板系统内固定治疗脊髓型颈椎病的疗效比较[J]. 中华骨科杂志, 2015,35(11):1136-1141. [10] SCHOLZ M, REYES PM, SCHLEICHER P, et al. A new stand-alone cervical anterior interbody fusion device: Biomechanical comparison with established anterior cervical fixation devices. Spine. 2009;34(2):156-160. [11] 许洁慧,郝志娜,朴京京,等. 择时穴位刺激对脑卒中后吞咽障碍患者的影响[J].实用临床医药杂志,2021,25(17):70-75. [12] DAI L, QIN C, GUO P, et al. Comparison of anterior cervical diskectomy with fusion (ACDF) and laminoplasty treating multilevel cervical spondylotic myelopathy with developmental canal stenosis: a retrospective study. J Orthop Surg Res. 2024;19(1):29. [13] SUK KS, JIMENEZ KA, JO JH, et al. Anterior Plate-Screws and Lower Postoperative T1 Slope Affect Cervical Allospacer Failures in Multi-Level ACDF Surgery: Anterior Versus Posterior Fixation. Global Spine J. 2023;13(1):89-96. [14] TANG L, CHEN Y, WANG F, et al. Safety and efficacy of day anterior cervical discectomy and fusion procedure for degenerative cervical spondylosis: a retrospective analysis. BMC Musculoskelet Disord. 2024;25(1):223. [15] MESREGAH MK, BAKER M, YOON C, et al. Radiographic Risk Factors for Adjacent Segment Disease Following Anterior Cervical Discectomy and Fusion (ACDF): A Systematic Review and Meta-Analysis. Global Spine J. 2024;14(7):2183-2200. [16] BURKE CJ, SAMIM M, BABB JS, et al. Utility of a 2D kinematic HASTE sequence in magnetic resonance imaging assessment of adjacent segment degeneration following anterior cervical discectomy and fusion. Eur Radiol. 2024;34(2):1113-1122. [17] GAO H, TIAN Z, WANG Y, et al. Comparison study of anterior cervical zero-profile fusion cage (ROI-C) and traditional titanium plate plus fusion technique for the treatment of spinal cord type cervical spondylosis. Medicine. 2023;102(50):e36651. [18] 任杭岭,宋娜,徐大霞,等. 不同融合装置对脊髓型颈椎病前路椎管减压融合后颈椎矢状位参数的影响[J]. 中国组织工程研究,2024, 28(33):5375-5381. [19] VISCONTI MJ, ALENTADO VJ, MCFATRIDGE IM, et al. A comparison of dysphagia rates between long-segment anterior versus posterior cervical fusion. J Neurosurg Spine. 2024;41(5):628-638. [20] SHEN B, GAO Z, WANG B, et al. Relationship between intervertebral disc height and post operative dysphagia secondary to single-level anterior cervical discectomy and fusion- a retrospective study. BMC Musculoskelet Disord. 2024;25(1):369. [21] ALSOOF D, PERRY J, YANG DS, et al. Risk of Dysphagia and Dysphonia in Patients With Prior Thyroidectomy Undergoing Anterior Cervical Discectomy and Fusion. Global Spine J. 2024;14(2):494-502. [22] OPSENAK R, SNOPKO P, SUTOVSKY J, et al. Incidence and severity of dysphagia after anterior cervical discectomy and fusion with zero-profi le spacer: prospective study with 3-years follow-up. Bratisl Lek Listy. 2023;124(12):879-885. [23] LU H, WANG C, LI R, et al. Comparison of the long-term efficacy of ROI-C and conventional cage-plate in treatment of spinal cord injury without fracture or dislocation: a retrospective study. BMC Musculoskelet Disord. 2024;25(1):848. [24] YOSHIZAWA A, NAKAGAWA K, YOSHIMI K, et al. Analysis of swallowing function after anterior/posterior surgery for cervical degenerative disorders and factors related to the occurrence of postoperative dysphagia. Spine J. 2023;23(4):513-522. [25] TSALIMAS G, EVANGELOPOULOS DS, BENETOS IS, et al. Dysphagia as a Postoperative Complication of Anterior Cervical Discectomy and Fusion. Cureus. 2022;14(7):e26888. [26] RAI V, SHARMA V, KUMAR M, et al. A systematic review of risk factors and adverse outcomes associated with anterior cervical discectomy and fusion surgery over the past decade. J Craniovertebr Junction Spine. 2024;15(2):141-152. [27] HILIBRAND AS, CARLSON GD, PALUMBO MA, et al. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999;81(4):519-528. [28] LIU Y, WANG H, LI X, et al. Comparison of a zero-profile anchored spacer (ROI-C) and the polyetheretherketone (PEEK) cages with an anterior plate in anterior cervical discectomy and fusion for multilevel cervical spondylotic myelopathy. Eur Spine J. 2016;25(6):1881-1890. [29] SONG KJ, CHOI BW, JEON TS, et al. Adjacent segment degenerative disease: is it due to disease progression or a fusion-associated phenomenon? Comparison between segments adjacent to the fused and non-fused segments. Eur Spine J. 2011;20(11):1940-1945. [30] HARINATHAN B, JEBASEELAN D, YOGANANDAN N, et al. Comparing adjacent segment biomechanics between anterior and posterior cervical fusion using patient-specific finite element modeling. Asian Spine J. 2024;18(6):777-793. [31] LIANG W, YANG Y, HAN B, et al. Biomechanical Analysis of Hybrid Artificial Discs or Zero-Profile Devices for Treating 1-Level Adjacent Segment Degeneration in ACDF Revision Surgery. Neurospine. 2024; 21(2):606-619. [32] SAAVEDRA-POZO FM, DEUSDARA RAM, BENZEL EC. Adjacent segment disease perspective and review of the literature. Ochsner J. 2014; 14(1):78-83. [33] WEI Z, YANG S, ZHANG Y, et al. Prevalence and Risk Factors for Cervical Adjacent Segment Disease and Analysis of the Clinical Effect of Revision Surgery: A Minimum of 5 Years’ Follow-Up. Global Spine J. 2023;15(2):314-320. [34] TEO SJ, GOH GS, YEO W, et al. The Relationship between Cervical Sagittal Balance and Adjacent Segment Disease after Three-level Anterior Cervical Discectomy and Fusion. Clin Spine Surg. 2021;34(5): e264-e270. [35] LIU C, LI Y, LI X, et al. Factors related to T1 slope: spinopelvic balance and thoracic compensation. BMC Surg. 2023;23(1):145. [36] WEI Z, YANG S, ZHANG Y, et al. Prevalence and Risk Factors for Cervical Adjacent Segment Disease and Analysis of the Clinical Effect of Revision Surgery: A Minimum of 5 Years’ Follow-Up. Global Spine J. 2025;15(2):314-320. [37] LIANG X, RAN L, ZHANG Z, et al. Development and validation of a predictive model for the risk of symptomatic adjacent segmental degeneration after anterior cervical discectomy and fusion. Front Neurol. 2025;16:1530257. [38] CHUNG TT, HUENG DY, LIN SC. Biomechanical comparison of static and dynamic cervical plates in terms of the bone fusion, tissue degeneration, and implant behavior. J Orthop Surg Res. 2024; 19(1):142. [39] CHIEN A, LAI DM, WANG SF, et al. Differential segmental motion contribution of single- and two-level anterior cervical discectomy and fusion. Eur Spine J. 2015;24(12):2857-2865. [40] 张在恒, 厉玉杰, 王永峰, 等. 颈椎前路钢板与零切迹系统治疗多节段伴后凸畸形颈椎病[J]. 实用骨科杂志,2017,23(7):600-608. [41] PARK JB, CHO YS, RIEW KD. Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Joint Surg Am. 2005; 87(3):558-563. |
| [1] | Li Zhifei, Han Bin, Liu Qiuli, Zhang Zhanming, Wei Haokai, Zuo Kuangshi, Zhang Yisheng. Cervical motion characteristics in patients with cervical spondylotic radiculopathy based on motion capture technology [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2286-2293. |
| [2] | Wang Nan, Chen Shuang, Xi Zhipeng, Qian Yuzhang, Zhang Xiaoyu, Gu Jun, Kang Ran, Xie Lin. MRI evaluation of nerve root subsidence sign affecting efficacy of percutaneous endoscopic decompression in lumbar spinal stenosis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2262-2268. |
| [3] | Zhang Xianxu, Ma Zhong, Liu Xin, Huang Lei, Shen Wenxiang, Luo Zhiqiang . Lumbar fusion combined with unilateral fixation for lumbar degenerative diseases: biomechanics, technical evolution, and clinical applications [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2334-2342. |
| [4] | Zhu Xiaolong, Zhang Wei, Yang Yang. Visualization analysis of research hotspots and cutting-edge information in the field of intervertebral disc regeneration and repair [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2391-2402. |
| [5] | Xinjiang Branch of China Trauma Rescue & Treatment Association. Expert consensus on diagnosis and treatment of brucellar osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2403-2412. |
| [6] | Wen Fayan, Li Yan, Qiang Tianming, Yang Chen, Shen Linming, Li Yadong, Liu Yongming. Unilateral biportal endoscopic technology for treatment of lumbar degenerative diseases: global research status and changing trends [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2380-2390. |
| [7] | Wang Qisa, Lu Yuzheng, Han Xiufeng, Zhao Wenling, Shi Haitao, Xu Zhe. Cytocompatibility of 3D printed methyl acrylated hyaluronic acid/decellularized skin hydrogel scaffolds [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1912-1920. |
| [8] | Wang Songpeng, Liu Yusan, Yu Huanying, Gao Xiaoli, Xu Yingjiang, Zhang Xiaoming, Liu Min. Bidirectional regulation of reactive oxygen species based on zeolitic imidazolate framework-8 nanomaterials: from tumor therapy and antibacterial activity to cytoprotection [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2033-2013. |
| [9] | Sun Lei, Zhang Qi, Zhang Yu. Pro-osteoblastic effect of chlorogenic acid protein microsphere/polycaprolactone electrospinning membrane [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1877-1884. |
| [10] | Wu Yanting, Li Yu, Liao Jinfeng. Magnesium oxide nanoparticles regulate osteogenesis- and angiogenesis-related gene expressions to promote bone defect healing [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1885-1895. |
| [11] | Li Qingbin, Lin Jianhui, Huang Wenjie, Wang Mingshuang, Du Jiankai, Lao Yongqiang. Bone cement filling after enlarged curettage of giant cell tumor around the knee joint: a comparison of subchondral bone grafting and non-grafting [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1896-1902. |
| [12] | Jiang Xinghai, Song Yulin, Li Dejin, Shao Jianmin, Xu Junzhi, Liu Huakai, Wu Yingguo, Shen Yuehui, Feng Sicheng. Vascular endothelial growth factor 165 genes transfected into bone marrow mesenchymal stem cells to construct a vascularized amphiphilic peptide gel module [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1903-1911. |
| [13] | Gao Yanguo, Guo Xu, Li Xiaohan, Chen Shiqi, Zhu Haitao, Huang Liangyong, Ye Fang, Lu Wei Wang Qibin, Zheng Tao, Chen Li. Optimization of prescription ratio of “Honghuangbai” gel by orthogonal test in diabetic skin wound mouse models [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1921-1928. |
| [14] | Liu Hongjie, Mu Qiuju, Shen Yuxue, Liang Fei, Zhu Lili. Metal organic framework/carboxymethyl chitosan-oxidized sodium alginate/platelet-rich plasma hydrogel promotes healing of diabetic infected wounds [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1929-1939. |
| [15] | Min Changqin, Huang Ying. Construction of pH/near-infrared laser stimuli-responsive drug delivery system and its application in treatment of oral squamous cell carcinoma [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1940-1951. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||