Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (12): 2994-3004.doi: 10.12307/2026.661
Previous Articles Next Articles
GJK Tablets intervene in cartilage homeostasis to protect articular cartilage of mice with knee osteoarthritis
Li Yijin1, Li Jiahao2, Zhang Haitao3, Huang Yiwei4, Chen Jinlun5, Zeng Yirong5, Feng Wenjun5
- Li Yijin1, Li Jiahao2, Zhang Haitao3, Huang Yiwei4, Chen Jinlun5, Zeng Yirong5, Feng Wenjun5
1Shenzhen Clinical College of Integrated Chinese and Western Medicine, Guangzhou University of Chinese Medicine, Shenzhen 518100, Guangdong Province, China; 2Department of Joint Orthopedics, Panyu District Hospital of Traditional Chinese Medicine, Guangzhou 511400, Guangdong Province, China; 3Longhua Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai 200032, China; 4Zhongshan Hospital of Traditional Chinese Medicine Affiliated to Guangzhou University of Chinese Medicine, Zhongshan 528400, Guangdong Province, China; 5The First Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China
-
Received:2025-03-13Accepted:2025-08-04Online:2026-04-28Published:2025-09-28 -
Contact:Zeng Yirong, MD, Professor, The First Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China -
About author:Li Yijin, MD candidate, Shenzhen Clinical College of Integrated Chinese and Western Medicine, Guangzhou University of Chinese Medicine, Shenzhen 518100, Guangdong Province, China Corresponding author: Feng Wenjun, MD, Associate professor, The First Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China -
Supported by:The National Natural Science Foundation of China (Youth Fund), No. 82104882 (to FWJ); The National Natural Science Foundation of China (General Program), No. 82374484 (to ZYR)
CLC Number:
Cite this article
Li Yijin, Li Jiahao, Zhang Haitao, Huang Yiwei, Chen Jinlun, Zeng Yirong, Feng Wenjun. GJK Tablets intervene in cartilage homeostasis to protect articular cartilage of mice with knee osteoarthritis[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(12): 2994-3004.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

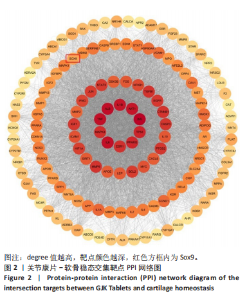
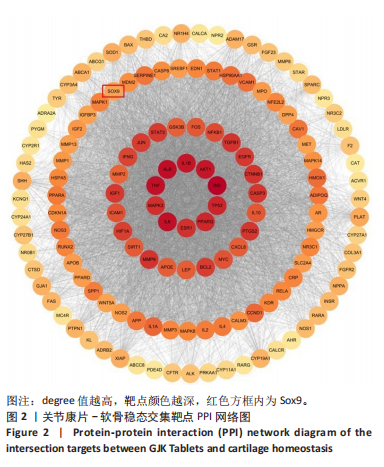
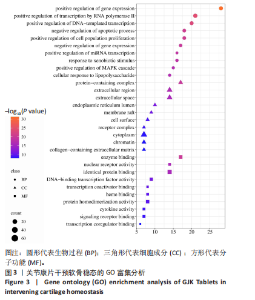
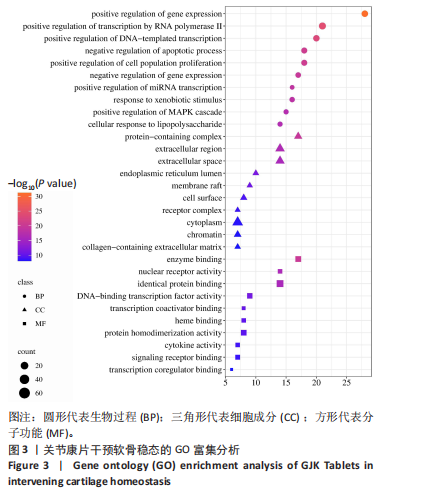
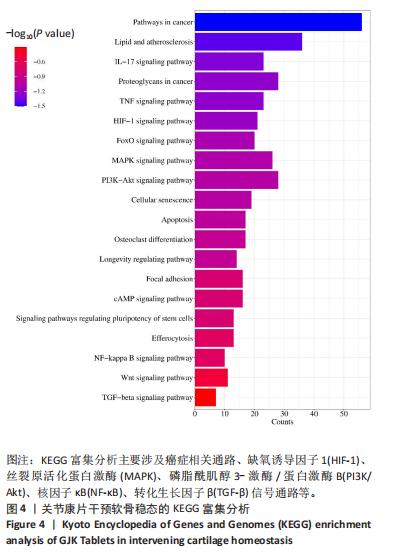
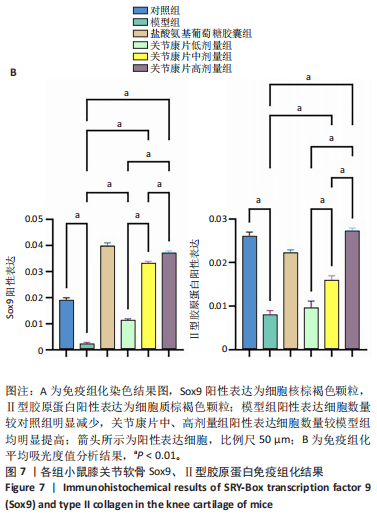
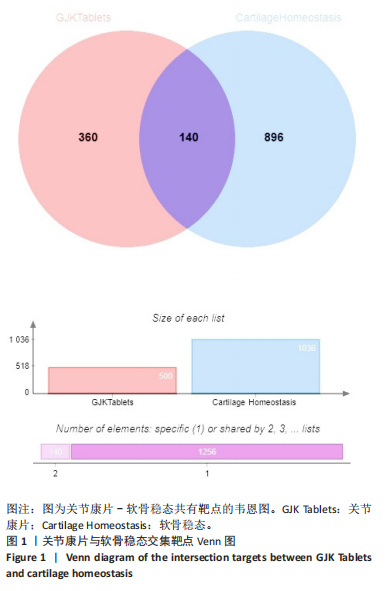
2.1 关节康片成分靶点与软骨稳态靶点交集分析 通过TCMSP、BATMAN-TCM数据库,设置生物利用度≥30%,类药性≥0.18,去除重复项,共检索到关节康片活性成分321个。使用SwissTargetPrediction数据库对以上有效成分进行靶点预测,剔除可信度为0的靶点,共获得500个潜在靶点。 检索GeneCards数据库得到软骨稳态靶点7 407个,靶点relevance score最高为74.27,最低为0.21,取relevance score排名前1 000的靶点作为潜在靶点。OMIM数据库检索到45个靶点,DisGeNET数据库检索到0个靶点。合并以上数据库靶点,去除重复项,最终得到软骨稳态相关靶点1 036个。将关节康片潜在靶点与软骨稳态靶点取交集,共得到“关节康片-软骨稳态”交集靶点140个,见图1。 2.2 交集靶点PPI网络构建 将交集靶点导入String平台,设置可信度为≥0.4,同时删除游离节点,构建关节康片-软骨稳态PPI网络,共有139个节点,3 514条边。将该PPI网络数据导入Cytoscape 3.10.3 软件,使用degree值进行排序,发现最高degree值为232,最低为2,其中Sox9的degree值为88,最后将PPI网络进行可视化展示,见图2。 2.3 GO和KEGG富集分析 通过DAVID数据库对关节康片-软骨稳态交集靶点进行GO和KEGG富集分析,并筛选P值≤0.01的结果,最终得到GO分析条目673条,KEGG分析条目142条。使用微生信平台,取GO富集前10位条目进行气泡图可视化,见图3。GO分析显示,生物过程主要涉及基因表达的正向调控、RNA聚合酶Ⅱ介导的转录正向调控、凋亡过程的负向调控、细胞群体增殖的正向调控等,细胞组分主要涉及含蛋白质的复合物、细胞外区域、内质网腔、膜筏等,分子功能主要涉及酶结合、核受体活性、转录共激活因子结合、转录共调节因子结合等。 取KEGG富集前20位条目进行柱状图可视化,见图4。KEGG分析显示,关节康片干预软骨稳态主要涉及癌症相关通路、缺氧诱导因子1(Hypoxia Inducible Factor-1,HIF-1)、丝裂原活化蛋白激酶(Mitogen- Activated Protein Kinase,MAPK)、磷脂酰肌醇3-激酶/蛋白激酶B(Phosphatidylinositol 3-Kinase/Akt,PI3K/Akt)、核因子κB(Nuclear Factor-κB,NF-κB)、转化生长因子β(Transforming Growth Factor-β,TGF-β)等信号通路。"

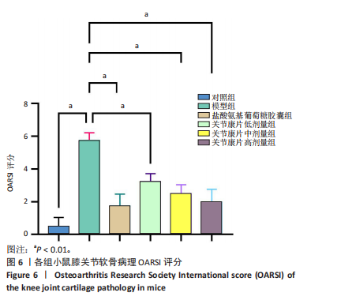
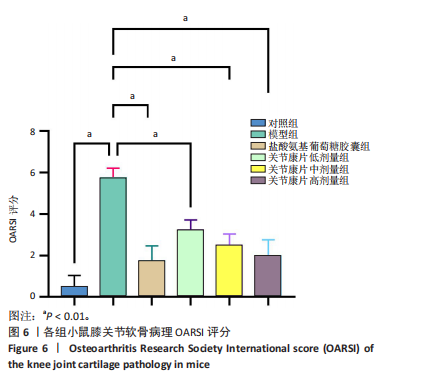
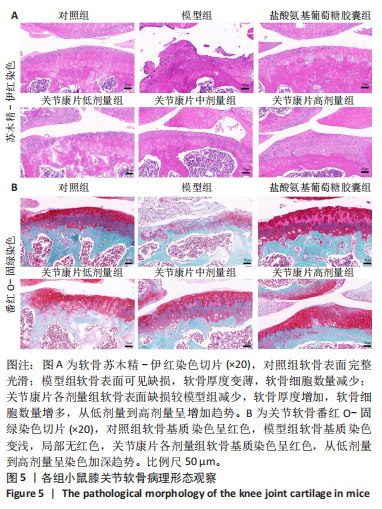
2.4 实验动物数量分析 实验共选取48只小鼠,造模、饲养及灌胃过程中无死亡,全部纳入结果分析。 2.5 各组小鼠软骨病理染色情况 2.5.1 苏木精-伊红染色结果 见图5A。对照组软骨表面完整光滑,未见明显缺损,软骨细胞排列正常;模型组软骨轮廓形变,软骨局部见缺损、分层,软骨厚度及软骨细胞数量明显减少;关节康片各剂量组软骨表面完整,低剂量组软骨缺损较小,中、高剂量组未见明显软骨缺损,软骨厚度及软骨细胞数量增加,从关节康片低剂量组到高剂量组呈增加趋势,软骨细胞排列均匀;盐酸氨基葡萄糖胶囊组软骨表面相对完整,软骨缺损较小,软骨厚度增加,软骨细胞数量增多。 2.5.2 番红O-固绿染色结果 见图5B。对照组软骨基质染色明显,软骨细胞排列均匀,未见明显软骨细胞增生变化,潮线清晰;模型组软骨基质番红染色变浅,软骨细胞数量明显减少,排列紊乱,潮线模糊;关节康片各剂量组软骨番红染色较模型组加深,软骨细胞数量较模型组增多,从关节康片低剂量组到高剂量组呈增加趋势,潮线清晰;盐酸氨基葡萄糖组软骨基质番红染色较模型组变深,软骨细胞数量较模型组增多,潮线完整。"
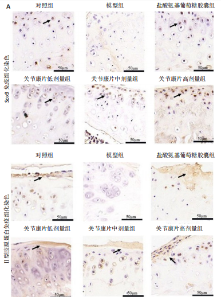
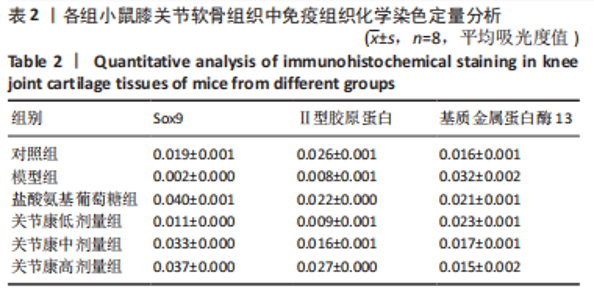
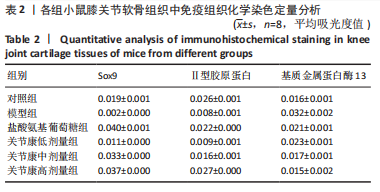
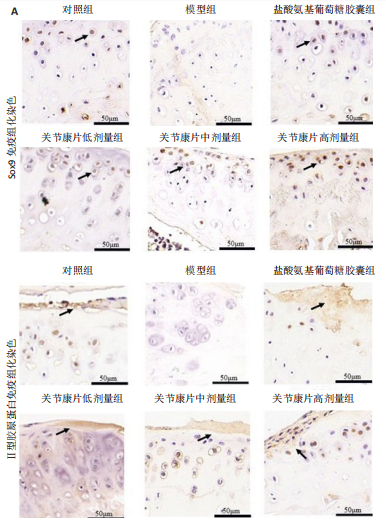
2.7 各组小鼠软骨Sox9、Ⅱ型胶原蛋白免疫组化分析 各组小鼠软骨组织中均有Sox9及Ⅱ型胶原蛋白表达,见图7A。Sox9、Ⅱ型胶原蛋白的表达在免疫组化软骨组织中分别表现为细胞核棕褐色颗粒及质棕褐色。与对照组相比,模型组Sox9、Ⅱ型胶原蛋白染色较浅,阳性表达细胞数量明显减少;与模型组相比,关节康片中、高剂量组的Sox9、Ⅱ型胶原蛋白染色均加深,阳性表达细胞数量均明显提高。免疫组化平均吸光度值见表2,图7B。与对照组相比,模型组Sox9、Ⅱ型胶原蛋白阳性表达明显降低(P < 0.01);与模型组相比,关节康片中、高剂量组的Sox9、Ⅱ型胶原蛋白阳性表达均明显提高(P < 0.01),且从关节康片低剂量到高剂量组阳性表达呈增加趋势(P < 0.01);关节康片低剂量组Sox9阳性表达明显提高(P < 0.01),Ⅱ型胶原蛋白阳性表达差异无显著意义(P > 0.05)。"

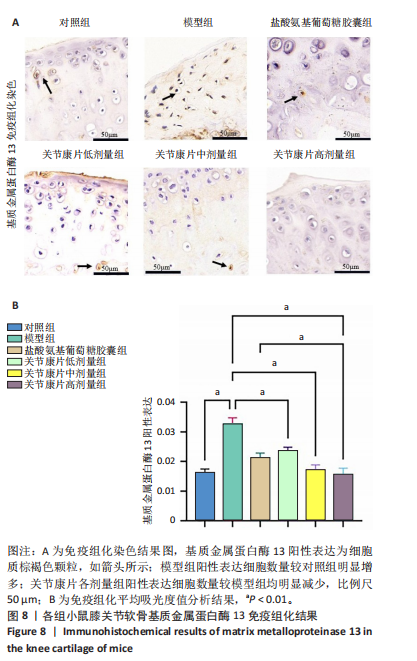
2.8 各组小鼠软骨基质金属蛋白酶13免疫组化分析 各组小鼠软骨组织中均可观察到基质金属蛋白酶13表达,见图8A。在免疫组化软骨组织中,基质金属蛋白酶13阳性表达为细胞质棕褐色颗粒。与对照组相比,模型组基质金属蛋白酶13染色加深,阳性表达细胞数量明显增多;与模型组相比,关节康片低、中、高剂量组的基质金属蛋白酶13染色均较浅,阳性表达细胞数量均明显减少。免疫组化平均光密度值见表2,分析结果见图8B。与对照组相比,模型组基质金属蛋白酶13阳性表达明显增加(P < 0.01);与模型组相比,关节康片各剂量组的基质金属蛋白酶13阳性表达均明显减少(P < 0.01);与盐酸氨基葡萄糖胶囊组相比,关节康片高剂量组的基质金属蛋白酶13阳性表达明显降低(P < 0.01)。"
| [1] GELBER AC. Knee Osteoarthritis. Ann Intern Med. 2024;177(9):ITC129-ITC144. [2] YAO Q, WU X, TAO C, et al. Osteoarthritis: pathogenic signaling pathways and therapeutic targets. Signal Transduct Target Ther. 2023; 8(1):56. [3] PENG Z, SUN H, BUNPETCH V, et al. The regulation of cartilage extracellular matrix homeostasis in joint cartilage degeneration and regeneration. Biomaterials. 2021;268:120555. [4] SHAO R, SUO J, ZHANG Z, et al. H3K36 methyltransferase NSD1 protects against osteoarthritis through regulating chondrocyte differentiation and cartilage homeostasis. Cell Death Differ. 2024;31(1):106-118. [5] SHARMA L. Osteoarthritis of the Knee. N Engl J Med. 2021;384(1):51-59. [6] GIORGINO R, ALBANO D, FUSCO S, et al. Knee Osteoarthritis: Epidemiology, Pathogenesis, and Mesenchymal Stem Cells: What Else Is New? An Update. Int J Mol Sci. 2023;24(7):6405. [7] 傅永升, 谭茗月, 王卫国, 等. 中药调控膝骨关节炎相关信号通路的研究进展[J].中国实验方剂学杂志,2023,29(22):231-243. [8] 陈丹丹, 武晏屹, 姬叔梅, 等. 基于文献分析的治疗膝骨关节炎中药应用规律分析[J].中药药理与临床,2022,38(4):186-191. [9] 李晓峰, 刘元禄, 关雪峰, 等. 补肾活血方剂治疗膝骨关节炎研究进展[J]. 辽宁中医药大学学报,2023,25(10):142-146. [10] 杨浩宇, 王世坤, 杨东元, 等.补肾活血中药治疗膝骨性关节炎与骨质疏松症“共病”机制研究进展[J].中草药,2024,55(11):3898-3905. [11] 唐立明, 李鹏飞, 庞智晖, 等. 樊粤光治疗膝骨性关节炎经验介绍[J].新中医,2017,49(5):146-147. [12] 梁笃, 樊粤光, 王海彬. 关节康治疗膝骨性关节炎22例临床观察[J]. 新中医,2009,41(6):59-60. [13] 梁笃, 樊粤光, 王海彬. 关节康结合关节镜技术治疗膝骨性关节炎23例[J]. 江西中医药,2009,40(7):28-30. [14] 曹厚然, 冯文俊, 陈昭, 等. 关节康片调控白细胞介素6表达促进膝关节损伤修复的机制及相关生物标志物的测定[J]. 广州中医药大学学报,2020,37(11):2210-2218. [15] 周斌, 樊粤光, 曾意荣. 中药关节康对骨性关节炎软骨TGF-β1、IL-1β表达的影响[J]. 中国中医骨伤科杂志,2009,17(2):11-13. [16] 梁笃, 樊粤光, 王海彬, 等. 关节康中药血清促进去分化软骨细胞再分化的实验研究[J]. 新中医,2009,41(4):101-103. [17] FUJII Y, LIU L, YAGASAKI L, et al. Cartilage Homeostasis and Osteoarthritis. Int J Mol Sci. 2022;23(11):6316. [18] ZHANG X, WU S, ZHU Y, et al. Exploiting Joint-Resident Stem Cells by Exogenous SOX9 for Cartilage Regeneration for Therapy of Osteoarthritis. Front Med (Lausanne). 2021;8:622609. [19] MUTHU S, KORPERSHOEK JV, NOVAIS EJ, et al. Failure of cartilage regeneration: emerging hypotheses and related therapeutic strategies. Nat Rev Rheumatol. 2023;19(7):403-416. [20] YEE JL, HUANG CY, YU YC, et al. Potential Mechanisms of Guizhi Fuling Wan in Treating Endometriosis: An Analysis Based on TCMSP and DisGeNET Databases. J Ethnopharmacol. 2024;329:118190. [21] KONG X, LIU C, ZHANG Z, et al. BATMAN-TCM 2.0: an enhanced integrative database for known and predicted interactions between traditional Chinese medicine ingredients and target proteins. Nucleic Acids Res. 2024;52(D1):D1110-D1120. [22] PESARE E, VICENTI G, KON E, et al. Italian Orthopaedic and Traumatology Society (SIOT) position statement on the non-surgical management of knee osteoarthritis. J Orthop Traumatol. 2023;24(1):47. [23] HERRERO-BEAUMONT G,LARGO R.Glucosamine and O-GlcNAcylation:a novel immunometabolic therapeutic target for OA and chronic, low-grade systemic inflammation? Ann Rheum Dis. 2020;79(10):1261-1263. [24] 程丽丽, 黄传兵, 陈君洁, 等. 重骨颗粒干预膝骨关节炎大鼠细胞焦亡的机制[J].中国骨质疏松杂志,2024,30(9):1317-1322. [25] Ji X, Du W, Che W, et al. Apigenin Inhibits the Progression of Osteoarthritis by Mediating Macrophage Polarization. Molecules. 2023;28(7):2915. [26] ZHU S, QU W, HE C. Evaluation and management of knee osteoarthritis.J Evid Based Med. 2024;17(3):675-687. [27] COURTIES A, KOUKI I, SOLIMAN N, et al. Osteoarthritis year in review 2024: Epidemiology and therapy. Osteoarthritis Cartilage. 2024; 32(11):1397-1404. [28] YOU B, ZHOU C, YANG Y. MSC-EVs alleviate osteoarthritis by regulating microenvironmental cells in the articular cavity and maintaining cartilage matrix homeostasis. Ageing Res Rev. 2023;85:101864. [29] LIU X, JIANG S, JIANG T, et al. Bioenergetic-active exosomes for cartilage regeneration and homeostasis maintenance. Sci Adv. 2024; 10(42):eadp7872. [30] WANG Z, EFFERTH T, HUA X, et al. Medicinal plants and their secondary metabolites in alleviating knee osteoarthritis: A systematic review. Phytomedicine. 2022;105:154347. [31] ZENG L, ZHOU G, YANG W, et al. Guidelines for the diagnosis and treatment of knee osteoarthritis with integrative medicine based on traditional Chinese medicine. Front Med (Lausanne). 2023;10:1260943. [32] 李慧, 周祥, 刘伟, 等. 补肾活血法治疗膝关节骨性关节炎机制研究进展[J]. 实用中医药杂志,2024,40(5):1027-1030. [33] 陈继鑫, 周沁心, 余伟杰, 等. 补肾活血法治疗膝骨关节炎随机对照试验结局指标的现状分析[J]. 中国中药杂志,2024,49(6):1661-1672. [34] KIM SM, JO SY, PARK HY, et al. Investigation of Drug-Interaction Potential for Arthritis Dietary Supplements:Chondroitin Sulfate, Glucosamine,and Methylsulfonylmethane. Molecules. 2023;28(24):8068. [35] MENG Z, LIU J, ZHOU N. Efficacy and safety of the combination of glucosamine and chondroitin for knee osteoarthritis: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2023;143(1):409-421. [36] RABADE A, VISWANATHA GL, NANDAKUMAR K, et al. Evaluation of efficacy and safety of glucosamine sulfate, chondroitin sulfate, and their combination regimen in the management of knee osteoarthritis: a systematic review and meta-analysis. Inflammopharmacology. 2024;32(3):1759-1775. [37] ROELOFS AJ, DE BARI C. Osteoarthritis year in review 2023: Biology.Osteoarthritis Cartilage. 2024;32(2):148-158. [38] ARAI Y, CHA R, NAKAGAWA S, et al. Cartilage Homeostasis under Physioxia. Int J Mol Sci. 2024;25(17):9398. [39] TAHEEM DK, JELL G, GENTLEMAN E.Hypoxia Inducible Factor-1alpha in Osteochondral Tissue Engineering. Tissue Eng Part B Rev. 2020; 26(2):105-115. [40] LU R, WANG YG, QU Y, et al. Dihydrocaffeic acid improves IL-1beta-induced inflammation and cartilage degradation via inhibiting NF-kappaB and MAPK signalling pathways. Bone Joint Res. 2023;12(4):259-273. [41] TIAN B, ZHANG L, ZHENG J, et al. The role of NF-kappaB-SOX9 signalling pathway in osteoarthritis. Heliyon. 2024;10(17):e37191. [42] KLAMPFLEUTHNER F, LOTZ B, RENKAWITZ T, et al.Stage-Dependent Activity and Pro-Chondrogenic Function of PI3K/AKT during Cartilage Neogenesis from Mesenchymal Stromal Cells. Cells. 2022;11(19):2965. [43] XU R, WU J, ZHENG L, et al. Undenatured type II collagen and its role in improving osteoarthritis. Ageing Res Rev. 2023;91:102080. [44] SONG H, PARK KH. Regulation and function of SOX9 during cartilage development and regeneration. Semin Cancer Biol. 2020;67(Pt 1):12-23. [45] DANALACHE M, UMRATH F, RIESTER R, et al. Proteolysis of the pericellular matrix: Pinpointing the role and involvement of matrix metalloproteinases in early osteoarthritic remodeling. Acta Biomater. 2024;181:297-307. [46] HU Q, ECKER M. Overview of MMP-13 as a Promising Target for the Treatment of Osteoarthritis. Int J Mol Sci. 2021;22(4):1742. [47] OUYANG Y, WANG W, TU B, et al. Overexpression of SOX9 alleviates the progression of human osteoarthritis in vitro and in vivo. Drug Des Devel Ther. 2019;13:2833-2842. [48] SHAO Y, ZHANG H, GUAN H, et al. PDZK1 protects against mechanical overload-induced chondrocyte senescence and osteoarthritis by targeting mitochondrial function. Bone Res. 2024;12(1):41. [49] FU B, SHEN J, ZOU X, et al. Matrix stiffening promotes chondrocyte senescence and the osteoarthritis development through downregulating HDAC3. Bone Res. 2024;12(1):32. [50] SUN Y, YOU Y, WU Q, et al. Senescence-targeted MicroRNA/Organoid composite hydrogel repair cartilage defect and prevention joint degeneration via improved chondrocyte homeostasis. Bioact Mater. 2024;39:427-442. [51] GUAN Z, JIN X, GUAN Z, et al. The gut microbiota metabolite capsiate regulate SLC2A1 expression by targeting HIF-1alpha to inhibit knee osteoarthritis-induced ferroptosis. Aging Cell. 2023;22(6):e13807. [52] LIU J, JIA S, YANG Y, et al. Exercise induced meteorin-like protects chondrocytes against inflammation and pyroptosis in osteoarthritis by inhibiting PI3K/Akt/NF-kappaB and NLRP3/caspase-1/GSDMD signaling. Biomed Pharmacother. 2023;158:114118. [53] ZHANG Z, MA J, YI Y, et al. Isoliensinine suppresses chondrocytes pyroptosis against osteoarthritis via the MAPK/NF-kappaB signaling pathway. Int Immunopharmacol. 2024;143(Pt 3):113589. [54] WANG L, XU H, LI X, et al. Cucurbitacin E reduces IL-1beta-induced inflammation and cartilage degeneration by inhibiting the PI3K/Akt pathway in osteoarthritic chondrocytes. J Transl Med. 2023;21(1):880. [55] LIU L, ZHAO C, ZHANG H, et al. Asporin regulated by miR-26b-5p mediates chondrocyte senescence and exacerbates osteoarthritis progression via TGF-beta1/Smad2 pathway. Rheumatology (Oxford). 2022;61(6):2631-2643. [56] PRIMORAC D, MOLNAR V, MATISIC V, et al.Comprehensive Review of Knee Osteoarthritis Pharmacological Treatment and the Latest Professional Societies’ Guidelines. Pharmaceuticals (Basel). 2021; 14(3):205. |
| [1] | Chen Qiuhan, Yang Long, Yuan Daizhu, Wu Zhanyu, Zou Zihao, Ye Chuan. Peri-knee osteotomy for treatment of knee osteoarthritis: optimization of treatment strategies [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2303-2312. |
| [2] | Li Linzhen, Jiao Hongzhuo, Chen Weinan, Zhang Mingzhe, Wang Jianlong, Zhang Juntao. Effect of icariin-containing serum on lipopolysaccharide-induced inflammatory damage in human chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1368-1374. |
| [3] | Gu Fucheng, Yang Meixin, Wu Weixin, Cai Weijun, Qin Yangyi, Sun Mingyi, Sun Jian, Geng Qiudong, Li Nan. Effects of Guilu Erxian Glue on gut microbiota in rats with knee osteoarthritis: machine learning and 16S rDNA analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 1058-1072. |
| [4] | Chen Yixian, Chen Chen, Lu Liheng, Tang Jinpeng, Yu Xiaowei. Triptolide in the treatment of osteoarthritis: network pharmacology analysis and animal model validation [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 805-815. |
| [5] | Li Xiaomin, Tian Xiangdong, Wang Chaolu. High tibial osteotomy on a single plane: femorofibular angle as a reference marker for mechanical axis correction [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 570-576. |
| [6] | Guo Jingwen, Wang Qingwei, He Zijun, Hu Zihang, Chen Zhi, Zhu Rong, Wang Yuming, Liu Wenfei, Luo Qinglu. Intra-articular injection of different concentrations of silicon-based bioceramics in treatment of knee osteoarthritis in rats [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(2): 288-295. |
| [7] | Ye Wei, Jiang Dongfu, Zhuang Jielin, Lai Huaxin. Effect of warm acupuncture combined with platelet-rich plasma injection on gait parameters and joint function recovery of knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(12): 2975-2985. |
| [8] | Lu Yuchun, Zhu Zimo, Li Chaomeng, Liu Ju, Jiang Zixian, Li Xiufang, Wang Tao, Wang Wenjing. Effect and mechanism of dichloromethane extract of fresh Sambucus adnata Wall. in rat osteoarthritis models [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(12): 3014-3028. |
| [9] | Ma Chi, Wang Ning, Chen Yong, Wei Zhihan, Liu Fengji, Piao Chengzhe. Application of 3D-printing patient-specific instruments combined with customized locking plate in opening wedge high tibial osteotomy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1863-1869. |
| [10] | Sun Yundi, Cheng Lulu, Wan Haili, Chang Ying, Xiong Wenjuan, Xia Yuan. Effect of neuromuscular exercise for knee osteoarthritis pain and function: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1945-1952. |
| [11] | Wang Peiguang, Zhang Xiaowen, Mai Meisi, Li Luqian, Huang Hao. Generalized equation estimation of the therapeutic effect of floating needle therapy combined with acupoint embedding on different stages of human knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1565-1571. |
| [12] | He Guanghui, Yuan Jie, Ke Yanqin, Qiu Xiaoting, Zhang Xiaoling. Hemin regulates mitochondrial pathway of oxidative stress in mouse chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1183-1191. |
| [13] | Ma Haoyu, Qiao Hongchao, Hao Qianqian, Shi Dongbo. Causal effects of different exercise intensities on the risk of osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1305-1311. |
| [14] | Xu Tianjie, Fan Jiaxin, Guo Xiaoling, Jia Xiang, Zhao Xingwang, Liu kainan, Wang Qian. Metformin exerts a protective effect on articular cartilage in osteoarthritis rats by inhibiting the PI3K/AKT/mTOR pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1003-1012. |
| [15] | Wu Guangtao, Qin Gang, He Kaiyi, Fan Yidong, Li Weicai, Zhu Baogang, Cao Ying . Causal relationship between immune cells and knee osteoarthritis: a two-sample bi-directional Mendelian randomization analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1081-1090. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||