Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (10): 2576-2583.doi: 10.12307/2026.616
Previous Articles Next Articles
Theta-stimulation for the treatment of motor function and daily activity ability in the lower extremities of stroke patients: a meta-analysis
Hu Xin1, Wan Haili1, Du Liang2, Li Yongjie3, Xia Yuan1
- 1Provincial Hospital of Hubei Province, Wuhan 430071, Hubei Province, China; 2Rehabilitation Medicine Department, General Hospital of the Central Theater Command, Wuhan 430000, Hubei Province, China; 3Guizhou Hospital of Beijing Jishuitan Hospital, Guiyang 550014, Guizhou Province, China
-
Received:2025-03-14Accepted:2025-06-27Online:2026-04-08Published:2025-08-30 -
Contact:Xia Yuan, MS, Primary rehabilitation therapist, Provincial Hospital of Hubei Province, Wuhan 430071, Hubei Province, China -
About author:Hu Xin, MS, Primary rehabilitation therapist, Provincial Hospital of Hubei Province, Wuhan 430071, Hubei Province, China -
Supported by:Guizhou Provincial Science and Technology Support Program in 2023, No. [2023] General 179 (to LYJ)
CLC Number:
Cite this article
Hu Xin, Wan Haili, Du Liang, Li Yongjie, Xia Yuan. Theta-stimulation for the treatment of motor function and daily activity ability in the lower extremities of stroke patients: a meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(10): 2576-2583.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
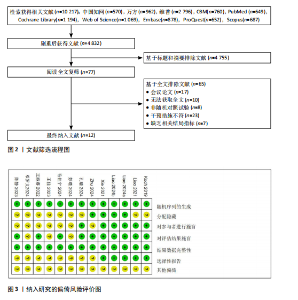
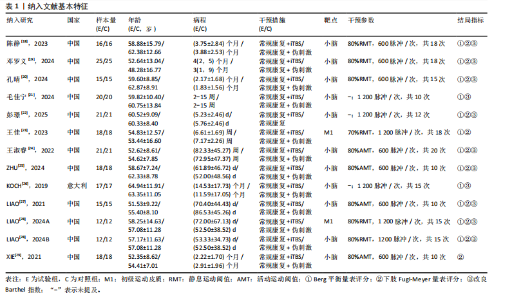
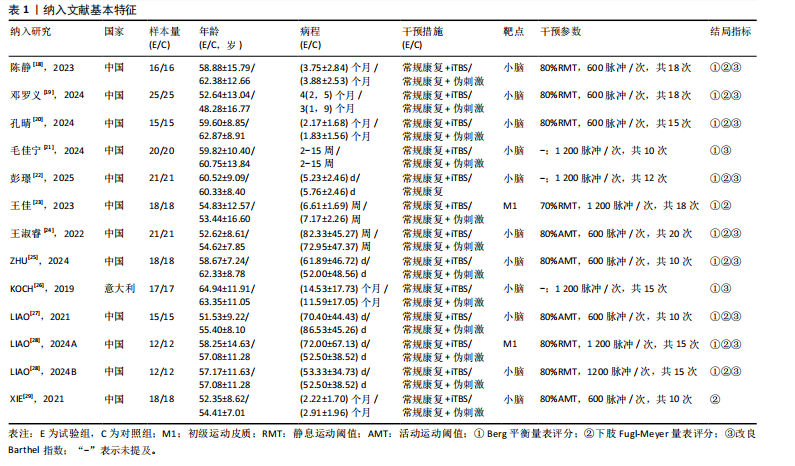
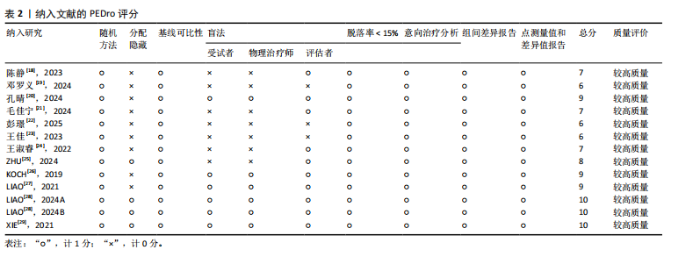
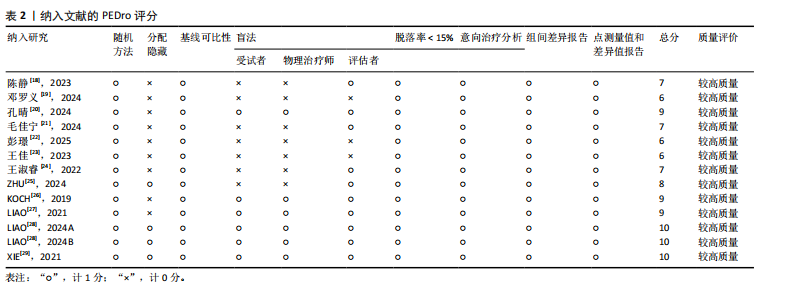
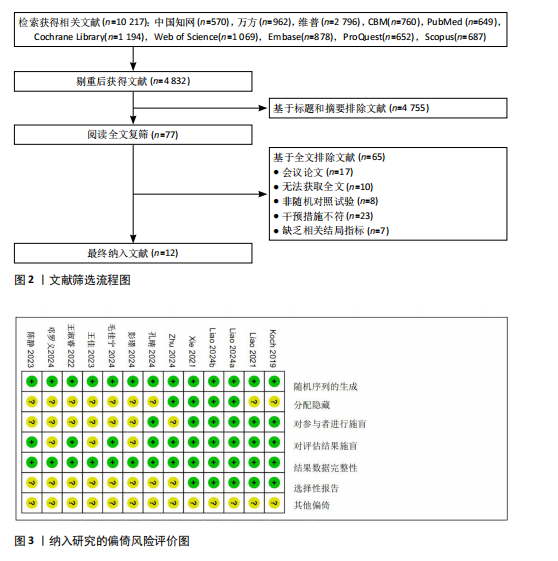
2.1 检索结果 检索到10 217篇文献,剔除重复文献后,剩余4 832篇文献。经标题和摘要筛选,77篇文献进入全文阅读环节,最终确定12篇文献符合系统综述标准,见图2。 2.2 纳入文献基本特征 此研究共纳入12篇文献[18-29],包括444例受试者。试验组均接受iTBS刺激,其中11项随机对照试验的刺激靶点为小脑[18-22,24-29],2项随机对照试验的刺激靶点为M1区[23,28]。对照组均采用常规治疗,见表1。 2.3 文献质量评价结果 由2名研究人员对纳入的12篇文献进行评估。这12篇文献均采用随机化分配方法(如随机数字法、随机信封法)[18-29],其中3篇文献实施了分配隐藏[25,28-29],5篇文献对参与者进行了施盲[20,26-29],9篇文献对结局指标的评估人员实施了盲法[18,20-21,24-29]。所有研究的结局数据均完整[18-29],4篇文献不存在选择性报告问题[26-29]。所有文献均未提及其他偏倚情况[18-29],因此认为其风险较低,见图3。参照PEDro量表评"

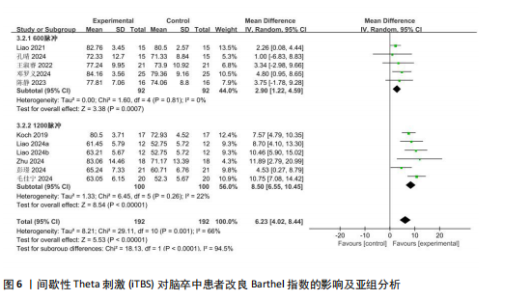
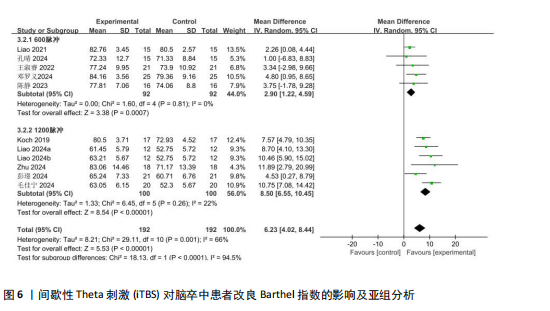
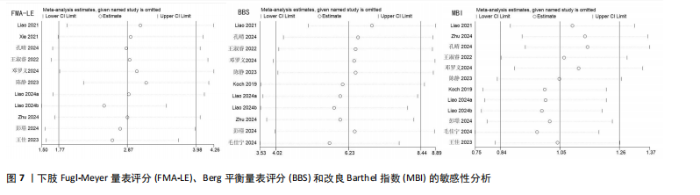
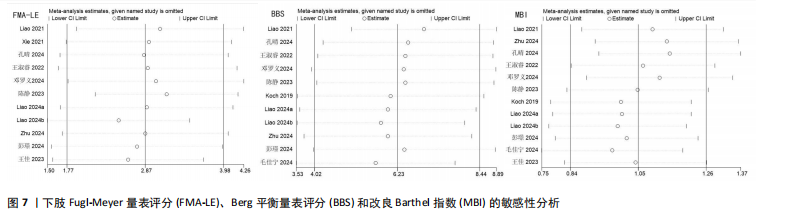
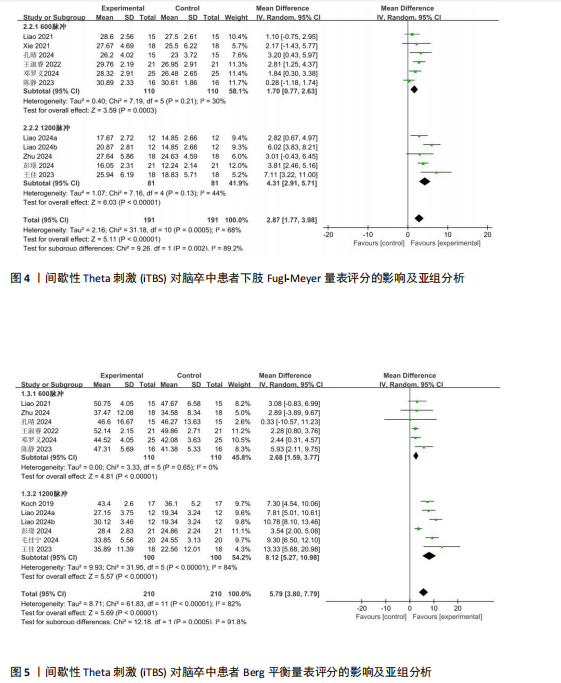
质性(I2=68%,P=0.000 5),故采用随机效应模型整合分析。结果显示,与对照组相比,iTBS组脑卒中受试者的FMA-LE评分有显著提高[WMD=2.87,95%CI(1.77,3.98),P < 0.000 01],见图4。 根据刺激总脉冲数的差异,将数据分为600脉冲和1 200脉冲2个亚组。其中,600脉冲亚组包括6项研究[18-20,24,27,29],共220例,各研究间异质性较小(P=0.21,I2=30%),采用固定效应模型。数据表明600脉冲数的iTBS能够有效改善脑卒中患者下肢运动功能[WMD=1.70,95%CI(0.77,2.63),P=0.000 3]。 1 200脉冲亚组包括4项研究[22,23,25,28],共150例,各研究间异质性较小(P=0.13,I2=44%),采用固定效应模型。数据表明1 200脉冲数的iTBS也能够提高脑卒中患者下肢运动功能[WMD=4.31,95%CI(2.91,5.71),P < 0.000 01]。两个亚组间存在显著异质性(P=0.002),其中1 200脉冲数亚组具有最高的效应量。 2.4.2 BBS评分 共11篇文献报告了BBS评分[9-28],共计408例受试者。因数据存在显著异质性(I2=82%,P < 0.000 01),故采用随机效应模型整合分析。结果显示,与对照组相比,iTBS组脑卒中患者BBS评分有显著改善[WMD=5.79,95%CI(3.80,7.79),P < 0.000 01],见图5。 根据刺激总脉冲数的差异,将数据分为600脉冲和1 200脉冲2个亚组。其中,600脉冲亚组包括6项研究[18-20,24-25,27],共220例,各研究间异质性较小(P=0.65,I2=0%),采用固定效应模型。数据表明600脉冲数的iTBS能够有效改善脑卒中患者的平衡功能[WMD=2.68,95%CI(1.59,3.77),P < 0.000 01]。1 200脉冲亚组包括5项研究[21-23,26,28],共188例,各研究间异质性较大(P < 0.000 01,I2=84%),采用随机效应模型。数据表明1 200脉冲数的iTBS也能够提高脑卒中患者的平衡功能[WMD=8.12,95%CI(5.27,10.98),P < 0.000 01]。两个亚组间效应量存在显著差异(P=0.000 5),其中1 200脉冲数亚组具有最高的效应量。 2.4.3 MBI 共10篇文献报告了MBI[18-22,24-28],总计372例受试者。因数据存在显著异质性(I2=66%,P=0.001),故采用随机效应模型整合分析。结果显示,与对照组相比,iTBS组脑卒中患者的MBI评分有明显改善[WMD=6.23,95%CI(4.02,8.44),P < 0.000 01],见图6。 根据刺激总脉冲数的差异,将数据分为600脉冲和1 200脉冲2个亚组。其中,600脉冲亚组包括5项研究[18-20,24,27],共184例,各研究间异质性较小(P=0.81,I2=0%),采用固定效应模型。数据表明600脉冲数的iTBS能够有效改善脑卒中患者的日常活动能力[WMD=2.90,95%CI (1.22,4.59),P=0.000 7]。1 200脉冲亚组包括5项研究[21,22,25-26,28],共188例,各研究间异质性较小(P=0.26,I2=22%),采用固定效应模型。数据表明1 200脉冲数的iTBS也能够提高脑卒中患者的日常活动能力[WMD=8.50,95%CI(6.55,10.45),P < 0.000 01]。两个亚组间效应量存在显著差异(P < 0.000 01),其中1 200脉冲数亚组具有最高的效应量。 2.4.4 发表偏倚检验 采用egger检验,结果显示,FMA-LE评分(t=1.14,P=0.282),BBS评分(t=1.40,P=0.192),MBI(t=0.87,P=0.409)均不存在明显的偏倚。 2.4.5 敏感性分析 采用依次排除法进行敏感性分析,结果显示FMA-LE评分、BBS评分及MBI指标较为稳定,见图7。"
| [1] SAINI V, GUADA L, YAVAGAL DR. Global Epidemiology of Stroke and Access to Acute Ischemic Stroke Interventions. Neurology. 2021;97(20 Suppl 2):S6-S16. [2] CHEN Y, SU W, GUI CF, et al. Effectiveness of cerebellar vermis intermittent theta-burst stimulation in improving trunk control and balance function for patients with subacute stroke: a randomised controlled trial protocol. BMJ Open. 2023;13(1):e066356. [3] GITTLER M, DAVIS AM. Guidelines for Adult Stroke Rehabilitation and Recovery. JAMA. 2018;319(8):820-821. [4] MEAD GE, HSIEH CF, LEE R, et al. Selective serotonin reuptake inhibitors for stroke recovery: a systematic review and meta-analysis. Stroke. 2013;44(3):844-850. [5] LANGHAMMER B, STANGHELLE JK. Can physiotherapy after stroke based on the Bobath concept result in improved quality of movement compared to the motor relearning programme. Physiother Res Int. 2011;16(2):69-80. [6] WOODFORD H, PRICE C. EMG biofeedback for the recovery of motor function after stroke. Cochrane Database Syst Rev. 2007; 2007(2):CD004585. [7] NATHOU C, DUPREY E, SIMON G, et al. Effects of low- and high-frequency repetitive transcranial magnetic stimulation on long-latency auditory evoked potentials. Neurosci Lett. 2018;686:198-204. [8] DUAN X, HUANG D, ZHONG H, et al. Efficacy of rTMS in treating functional impairment in post-stroke patients: a systematic review and meta-analysis. Neurol Sci. 2024;45(8): 3887-3899. [9] 夏渊,卢悦,李爱玲,等.θ节律刺激对脑卒中后患者上肢运动功能和日常生活能力影响的Meta分析[J].中国医学物理学杂志,2022,39(3):341-348. [10] CHUNG SW, HOY KE, FITZGERALD PB. Theta-burst stimulation: a new form of TMS treatment for depression? Depress Anxiety. 2015;32(3):182-192. [11] CARDENAS-MORALES L, NOWAK DA, KAMMER T, et al. Mechanisms and applications of theta-burst rTMS on the human motor cortex. Brain Topogr. 2010; 22(4):294-306. [12] GUTIÉRREZ-MUTO AM, CASTILLA J, FREIRE M, et al. Theta burst stimulation: Technical aspects about TMS devices. Brain Stimul. 2020;13(3):562-564. [13] KOCH G, ESPOSITO R, MOTTA C, et al. Improving visuo-motor learning with cerebellar theta burst stimulation: Behavioral and neurophysiological evidence. Neuroimage. 2020;208:116424. [14] LIN LF, CHANG KH, HUANG YZ, et al. Simultaneous stimulation in bilateral leg motor areas with intermittent theta burst stimulation to improve functional performance after stroke: a feasibility pilot study. Eur J Phys Rehabil Med. 2019; 55(2):162-168. [15] 陈伟群,王新德.全国第五届脑血管病学术会议纪要[J].中华神经科杂志,2000, 33(4):252. [16] HIGGINS JP, ALTMAN DG, GOTZSCHE PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [17] MAHER CG, SHERRINGTON C, HERBERT RD, et al. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713-721. [18] 陈静,石明芳,陈君,等.小脑间歇性θ短阵脉冲刺激联合物理治疗对脑卒中患者平衡功能和步态的影响[J].中华物理医学与康复杂志,2023,45(5):402-407. [19] 邓罗义,陈彦,曾妮,等.健侧小脑间歇性θ短阵脉冲刺激康复治疗对脑卒中患者下肢步行功能的影响[J].实用医学杂志,2024,40(13):1797-1802. [20] 孔晴,郭壮丽,高呈飞,等.小脑间歇性θ脉冲刺激对脑卒中后下肢功能障碍患者步行功能的影响[J].中华物理医学与康复杂志,2024,46(3):226-231. [21] 毛佳宁,张皓,崔利华.小脑经颅磁刺激对脑卒中偏瘫患者平衡及运动功能的影响[J].神经损伤与功能重建,2024, 19(10):574-578+604. [22] 彭瑾,谢珊,查益,等.间歇性θ短阵脉冲刺激小脑蚓部对脑卒中患者下肢运动功能障碍的影响[J].神经损伤与功能重建,2025,20(1):21-25. [23] 王佳,王先斌,宋宁,等.不同经颅磁刺激模式对脑卒中后下肢运动障碍患者肢体运动功能的影响[J].贵州医科大学学报,2023,48(6):702-709. [24] 王淑睿,李丽.小脑间歇性θ短阵快速脉冲刺激对脑卒中患者下肢运动功能的影响[J].中国康复理论与实践,2022, 28(10):1205-1210. [25] ZHU PA, LI ZL, LU QQ, et al. Can cerebellar theta-burst stimulation improve balance function and gait in stroke patients? A randomized controlled trial. Eur J Phys Rehabil Med. 2024;60(3):391-399. [26] KOCH G, BONNÌ S, CASULA EP, et al. Effect of Cerebellar Stimulation on Gait and Balance Recovery in Patients With Hemiparetic Stroke: A Randomized Clinical Trial. JAMA Neurol. 2019;76(2):170-178. [27] LIAO LY, XIE YJ, CHEN Y, et al. Cerebellar Theta-Burst Stimulation Combined With Physiotherapy in Subacute and Chronic Stroke Patients: A Pilot Randomized Controlled Trial. Neurorehabil Neural Repair. 2021;35(1):23-32. [28] LIAO LY, ZHU Y, PENG QY, et al. Intermittent Theta-Burst Stimulation for Stroke: Primary Motor Cortex Versus Cerebellar Stimulation: A Randomized Sham-Controlled Trial. Stroke. 2024;55(1):156-165. [29] XIE YJ, WEI QC, CHEN Y, et al. Cerebellar Theta Burst Stimulation on Walking Function in Stroke Patients: A Randomized Clinical Trial. Front Neurosci. 2021;15:688569. [30] MCKENNEY K, ELDER AS, ELDER C, et al. Myofascial release as a treatment for orthopaedic conditions: a systematic review. J Athl Train. 2013;48(4):522-527. [31] SMITH MC, BYBLOW WD, BARBER PA, et al. Proportional Recovery From Lower Limb Motor Impairment After Stroke. Stroke. 2017;48(5):1400-1403. [32] CHEN K, SUN M, ZHUANG H. Effect of theta burst stimulation on lower extremity motor function improvement and balance recovery in patients with stroke: A systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2024;103(44):e40098. [33] JEMNA N, ZDRENGHEA AC, FRUNZA G, et al. Theta-burst stimulation as a therapeutic tool in neurological pathology: a systematic review. Neurol Sci. 2024;45(3):911-940. [34] WANG CP, TSAI PY, YANG TF, et al. Differential effect of conditioning sequences in coupling inhibitory/facilitatory repetitive transcranial magnetic stimulation for poststroke motor recovery. CNS Neurosci Ther. 2014;20(4):355-363. [35] BALASUBRAMANIAN CK, LI CY, BOWDEN MG, et al. Dimensionality and Item-Difficulty Hierarchy of the Lower Extremity Fugl-Meyer Assessment in Individuals With Subacute and Chronic Stroke. Arch Phys Med Rehabil. 2016;97(4):582-589. [36] DI LAZZARO V, DILEONE M, PROFICE P, et al. Direct demonstration that repetitive transcranial magnetic stimulation can enhance corticospinal excitability in stroke. Stroke. 2006;37(11):2850-2853. [37] HUANG YZ, EDWARDS MJ, ROUNIS E, et al. Theta burst stimulation of the human motor cortex. Neuron. 2005;45(2):201-206. [38] FUNKE K, BENALI A. Modulation of cortical inhibition by rTMS - findings obtained from animal models. J Physiol. 2011;589(Pt 18): 4423-4435. [39] REHME AK, EICKHOFF SB, ROTTSCHY C, et al. Activation likelihood estimation meta-analysis of motor-related neural activity after stroke. Neuroimage. 2012;59(3):2771-2782. [40] LUFT AR, FORRESTER L, MACKO RF, et al. Brain activation of lower extremity movement in chronically impaired stroke survivors. Neuroimage. 2005;26(1):184-194. [41] BODDINGTON LJ, REYNOLDS JNJ. Targeting interhemispheric inhibition with neuromodulation to enhance stroke rehabilitation. Brain Stimul. 2017;10(2): 214-222. [42] ACOBS JV, HORAK FB. Cortical control of postural responses. J Neural Transm (Vienna). 2007;114(10):1339-1348. [43] NEULS PD, CLARK TL, VAN HEUKLON NC, et al. Usefulness of the Berg Balance Scale to predict falls in the elderly. J Geriatr Phys Ther. 2011;34(1):3-10. [44] SPAMPINATO DA, CELNIK PA, ROTHWELL JC. Cerebellar-Motor Cortex Connectivity: One or Two Different Networks? J Neurosci. 2020;40(21):4230-4239. [45] HANAKAWA T, HOTTA F, NAKAMURA T, et al. Macrostructural Cerebellar Neuroplasticity Correlates With Motor Recovery After Stroke. Neurorehabil Neural Repair. 2023; 37(11-12):775-785. [46] XIA Y, TANG X, HU R, et al. Cerebellum-Cerebrum paired target magnetic stimulation on balance function and brain network of patients with stroke: A functional near-infrared spectroscopy pilot study. Front Neurol. 2022;13:1071328. [47] TAN HX, WEI QC, CHEN Y, et al. The Immediate Effects of Intermittent Theta Burst Stimulation of the Cerebellar Vermis on Cerebral Cortical Excitability During a Balance Task in Healthy Individuals: A Pilot Study. Front Hum Neurosci. 2021;15: 748241. [48] CASULA EP, PELLICCIARI MC, PONZO V, et al. Cerebellar theta burst stimulation modulates the neural activity of interconnected parietal and motor areas. Sci Rep. 2016;6:36191. [49] DIAO X, LU Q, QIAO L, et al. Cortical Inhibition State-Dependent iTBS Induced Neural Plasticity. Front Neurosci. 2022;16:788538. [50] WANG YC, CHANG PF, CHEN YM, et al. Comparison of responsiveness of the Barthel Index and modified Barthel Index in patients with stroke. Disabil Rehabil. 2023;45(6):1097-1102. [51] CHUNG SW, HILL AT, ROGASCH NC, et al. Use of theta-burst stimulation in changing excitability of motor cortex: A systematic review and meta-analysis. Neurosci Biobehav Rev. 2016;63:43-64. [52] NETTEKOVEN C, VOLZ LJ, KUTSCHA M, et al. Dose-dependent effects of theta burst rTMS on cortical excitability and resting-state connectivity of the human motor system. J Neurosci. 2014;34(20):6849-6859. [53] YU F, TANG X, HU R, et al. The After-Effect of Accelerated Intermittent Theta Burst Stimulation at Different Session Intervals. Front Neurosci. 2020;14:576. [54] WILLIAMS NR, SUDHEIMER KD, BENTZLEY BS, et al. High-dose spaced theta-burst TMS as a rapid-acting antidepressant in highly refractory depression. Brain. 2018; 141(3):e18. [55] ANIL S, LU H, ROTTER S, et al. Repetitive transcranial magnetic stimulation (rTMS) triggers dose-dependent homeostatic rewiring in recurrent neuronal networks. PLoS Comput Biol. 2023;19(11):e1011027. [56] 黄如训,郭玉璞. 2000年广州全国脑血管病专题研讨会脑卒中的分型分期治疗(建议草案)[J]. 现代实用医学,2003,15(9): 592-594. [57] WANG L, HUANG G, ZHANG L, et al. Effects of the Intermittent Theta Burst Stimulation of the Cerebellar Vermis on Balance Recovery After Stroke: A Study Protocol for a Randomized Controlled Trial. Front Aging Neurosci. 2022;14:881311. [58] LI D, CHENG A, ZHANG Z, et al. Effects of low-frequency repetitive transcranial magnetic stimulation combined with cerebellar continuous theta burst stimulation on spasticity and limb dyskinesia in patients with stroke. BMC Neurol. 2021; 21(1):369. [59] CABRAL DF, FRIED P, KOCH S, et al. Efficacy of mechanisms of neuroplasticity after a stroke. Restor Neurol Neurosci. 2022; 40(2):73-84. |
| [1] | Wang Zheng, Cheng Ji, Yu Jinlong, Liu Wenhong, Wang Zhaohong, Zhou Luxing. Progress and future perspectives on the application of hydrogel materials in stroke therapy [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2081-2090. |
| [2] | Gao Feng, Zhang Jun, Yu Wenjun, Chanyu Yujing, Zhao Le, Hu Yuting, Wang Junhua, Liu Yongfu. Effects of wrist-hand orthosis on hand dysfunction in stroke patients: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2124-2131. |
| [3] | Tao Daiju, Su Haiyu, Wang Yuqi, Shen Zhiqiang, He Bo . Construction and identification of stable PC12 cell lines with high/low expression of miR-122-5p [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1790-1799. |
| [4] | Wang Zhenze, Liu Fende, Zhang Rui, Li Wujun. Mesenchymal stem cells in treatment of arteriosclerosis obliterans of lower extremities: systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1869-1876. |
| [5] | Zheng Yin, Wu Zhenhua, Zhang Cheng, Ruan Kexin, Gang Xiaolin, Ji Hong. Safety and efficacy of immunoadsorption therapy for rheumatoid arthritis: a network meta-analysis and systematic review [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1260-1268. |
| [6] | Chen Qiang, Wu Wenjuan, Jiang Shuhua, Huang Da. Physical exercise improves physical function in burn patients: a systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1269-1281. |
| [7] | Leng Xiaoxuan, Zhao Yuxin, Liu Xihua. Effects of different neuromodulatory stimulation modalities on non-motor symptoms in Parkinson’s patients: a network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1282-1293. |
| [8] | Wen Xiaolong, Weng Xiquan, Feng Yao, Cao Wenyan, Liu Yuqian, Wang Haitao. Effects of inflammation on serum hepcidin and iron metabolism related parameters in patients with type 2 diabetes mellitus: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1294-1301. |
| [9] | Wang Jie, Huang Rui, Zhang Ye, Shou Zhaoxi, Yao Jie, Liu Chenxi, Liao Jian. Role and mechanism of probiotics in peri-implantitis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 901-907. |
| [10] | Jin Zhiyong, Wang Yufeng, Zhao Binjie, Xiong Minquan, Yan Li. Effects of inter-limb asymmetry on athletic performance from the perspective of bilateral limb control strategy [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 949-963. |
| [11] | Jiang Yang, Peng Hao, Song Yanping, Yao Na, Song Yueyu, Yin Xingxiao, Li Yanqi, Chen Qigang. Isometric exercise reduces resting blood pressure: a meta-analysis of moderating factors and dose effects [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 975-986. |
| [12] | Li Hanyue, Li Yini, Xiang Linmei, Li Sen. Effects of resistance exercise therapy on pain and function in patients with cervical spondylotic radiculopathy: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 987-996. |
| [13] | Sun Jiahe, Shi Jipeng, Zhu Tianrui, Quan Helong, Xu Hongqi. Effect of exercise intervention in elderly individuals with sarcopenia and its comorbidities: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 997-1007. |
| [14] | Yang Yuanyuan, Zhou Shanshan, Cheng Xiaofei, Feng Luye, Tang Jiqin. Network meta-analysis of non-invasive brain stimulation in the treatment of lower limb motor dysfunction after stroke [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 1008-1018. |
| [15] | Yang Peng, Xu Chenghan, Zhou Yingjie, Chai Xubin, Zhuo Hanjie, Li Lin, Shi Jinyu. A meta-analysis of risk factors for residual back pain after vertebral augmentation for osteoporotic vertebral compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 731-739. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||