Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (3): 731-739.doi: 10.12307/2025.869
Previous Articles Next Articles
A meta-analysis of risk factors for residual back pain after vertebral augmentation for osteoporotic vertebral compression fractures
Yang Peng1, 2, Xu Chenghan2, Zhou Yingjie2, Chai Xubin2, Zhuo Hanjie2, Li Lin1, 2, Shi Jinyu1, 2
- 1Henan University of Chinese Medicine, Zhengzhou 450046, Henan Province, China; 2Department of Spine Surgery II, Henan Luoyang Orthopedic Hospital (Henan Orthopedic Hospital), Luoyang 471002, Henan Province, China
-
Received:2024-11-15Accepted:2024-12-31Online:2026-01-28Published:2025-07-07 -
Contact:Zhou Yingjie, MS, Professor, Chief physician, Department of Spine Surgery II, Henan Luoyang Orthopedic Hospital (Henan Orthopedic Hospital), Luoyang 471002, Henan Province, China -
About author:Yang Peng, Master candidate, Henan University of Chinese Medicine, Zhengzhou 450046, Henan Province, China; Department of Spine Surgery II, Henan Luoyang Orthopedic Hospital (Henan Orthopedic Hospital), Luoyang 471002, Henan Province, China -
Supported by:Henan Province Traditional Chinese Medicine Inheritance and Innovation Talent Project (Zhongjing Project) (to ZYJ)
CLC Number:
Cite this article
Yang Peng, Xu Chenghan, Zhou Yingjie, Chai Xubin, Zhuo Hanjie, Li Lin, Shi Jinyu. A meta-analysis of risk factors for residual back pain after vertebral augmentation for osteoporotic vertebral compression fractures[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 731-739.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

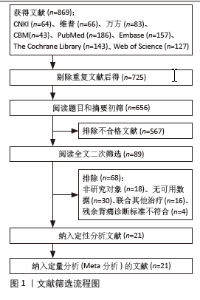
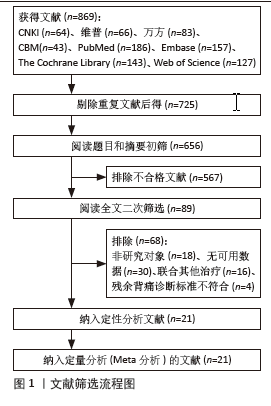
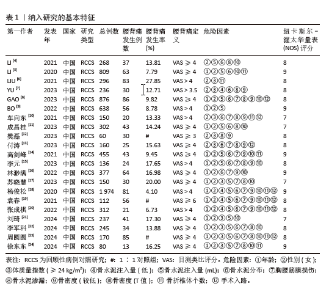
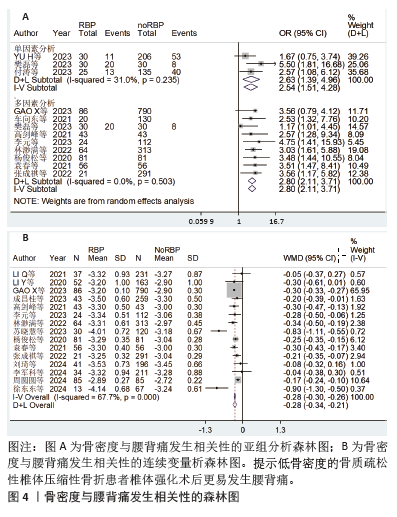
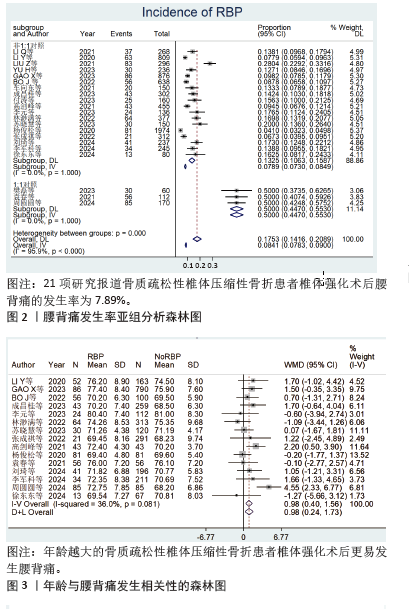
2.3 Meta分析结果 2.3.1 腰背痛新发病率 共有21项研究报道了OVCF患者在椎体强化术后新发腰背痛的发病率[4-24]。整体异质性评估显示高度异质性(I2=95.9%,P=0.000),表明各研究之间存在显著差异。为了探究这种高度异质性的来源,根据是否按照1∶1比例纳入对照组患者进行了亚组分析。结果显示,2个亚组内部的异质性较低,进一步确认了研究设计类型是导致整体异质性的主要原因。1∶1对照研究亚组示OR=0.500 0,95%CI:0.447 0-0.553 0,P=0.00;非1∶1对照研究亚组示OR=0.078 9,95%CI:0.073 0-0.084 9,P=0.00,由于1∶1对照研究组在纳入对照组患者时严格遵循了与研究组等比例的原则,其结果可能并未真实反映实际发生率,因此在最终分析中将其排除。通过亚组分析,确定了研究设计的不同是导致整体高度异质性的关键因素。非1∶1对照研究亚组提供了更接近实际情况的数据,据此估计,OVCF患者椎体强化术后新发腰背痛的发生率为7.89%(95%CI:0.073 0-0.084 9),见图2。 2.3.2 基于患者基本特征分析结果 (1)年龄:15项研究报道了患者年龄[5,8-9,11,14-24],经过异质性检验,I2=36.0%,且Q检验P=0.081 < 0.1,各研究存在中度异质性,经过敏感性分析无法消除异质性,敏感性分析显示结果稳定,采用随机效应模型进行分析结果示,WMD=0.98,95%CI:0.40-1.56,P=0.010,提示年龄越大的OVCF患者椎体强化术后更易发生腰背痛(表2,图3)。"
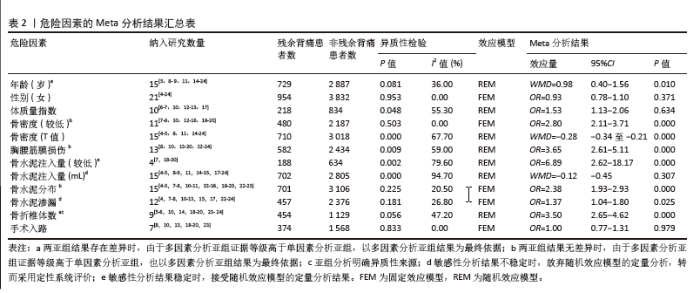
(2)性别:21项研究报道了患者性别[4-24],经过异质性检验,I2=0.00%,且Q检验P=0.953 > 0.1,各研究间无异质性,采用固定效应模型进行Meta分析结果示,OR=0.93,95%CI:0.78-1.10,P=0.371,提示性别与OVCF患者椎体强化术后发生腰背痛无关(表2)。 (3)体质量指数:6项研究报道了患者体质量指数[6-7,10,12-13,17],经过异质性检验,I2=55.3%,P=0.048 < 0.1,各研究间异质性高,采用随机效应模型进行分析结果示,OR=1.53,95%CI:1.13-2.06,P=0.634,提示体质量指数与OVCF患者椎体强化术后发生腰背痛无关(表2)。 (4)骨密度:19项研究报道了骨密度[4-5,7-8,10-24],其中11项研究报道了患者骨密度(较低)[7-8,10,12-16,18-20],其中3项研究报道了单因素分析的结果[7,12-13],Meta分析显示研究间有低异质性:I2=31.0%,P=0.235 > 0.1,采用固定效应模型进行分析结果示,OR=2.54,95%CI:1.51-4.28,P=0.00;9项研究报道了多因素分析的结果[8,10,12,14-16,18-20],Meta分析显示研究间无异质性:I2=0.0%,P=0.503 > 0.1,采用固定效应模型进行分析结果示,OR=2.80,95%CI:2.11-3.71,P=0.00。15项研究报道了患者骨密度(T值)[4-5,8,11,14-24],Meta分析显示研究间有高度异质性:I2=67.7%,P=0 < 0.1,经敏感性分析无法消除异质性,敏感性分析结果稳定,采用随机效应模型进行分析结果示,WMD=-0.28,95%CI:-0.34至-0.21,P=0.00,结果提示低骨密度是OVCF患者椎体强化术后发生腰背痛的独立危险因素(表2,图4)。"
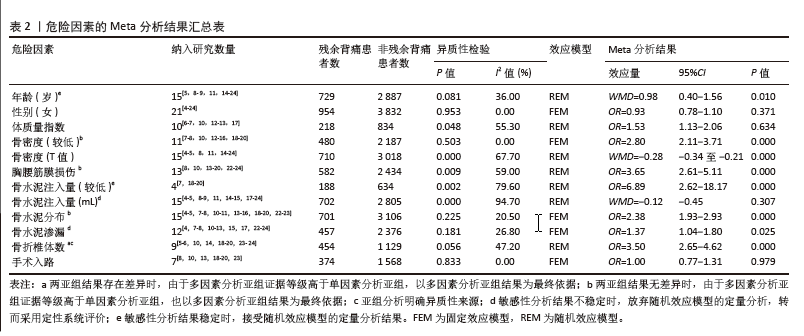
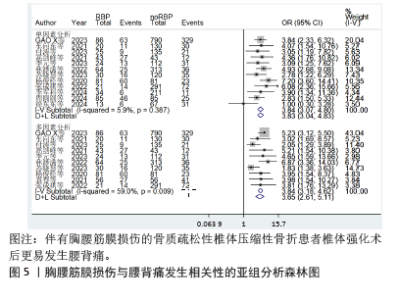
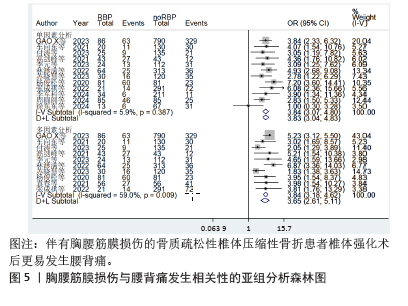
(5)胸腰筋膜损伤:13项研究报道了患者胸腰筋膜损伤[8,10,13-20,22-24],其中12项研究报道了单因素分析的结果[8,10,13-18,20,22-24],Meta分析显示各研究之间无异质性:I2=5.9%,P=0.387 > 0.1,采用固定效应模型进行分析结果示,OR=3.83,95%CI:3.04-4.83,P=0.00;10项研究报道了多因素分析的结果[8,10,13-20], Meta分析显示研究间有高度异质性:I2= 59.0%,P=0.009 < 0.1,经敏感性分析和亚组分析无法消除异质性,敏感性分析结果稳定,采用随机效应模型进行分析结果示,OR=3.65,95%CI:2.61-5.11,P=0.00。结果提示胸腰筋膜损伤是OVCF患者椎体强化术后发生腰背痛的独立危险因素(表2,图5)。"

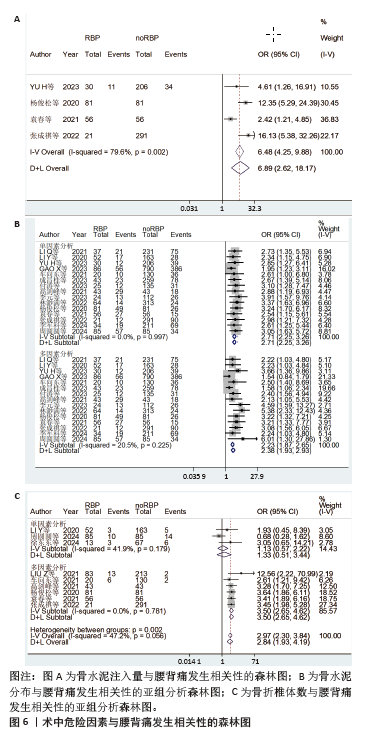
2.3.3 基于术中危险因素分析结果 (1)骨水泥注入量:16项研究报道了患者骨水泥注入量,其中4项多因素研究报道了患者骨水泥注入量(较 低)[7,18-20],Meta分析显示研究间有高度异质性:I2= 79.6%,P=0.002 < 0.1,经敏感性分析无法消除异质性,敏感性分析结果稳定,采用随机效应模型进行分析结果示,OR=6.89,95%CI:2.62-18.17,P=0.00(图6A);15研究报道了患者骨水泥注入量(mL)[4-5,8-9,11,14-15,17-24],Meta分析结果显示,研究间存在高度异质性:I2= 94.7%,P=0 < 0.1,进一步敏感性分析表明结果不稳定,因此放弃随机效应模型的定量分析,采用定性系统评价,10项研究均报道骨水泥注入量与椎体强化术后腰背痛的发生无关[4,8-9,11,15,17,21-24],4项研究表明骨水泥注入量少时椎体强化术后易发生腰背痛[5,14,18,20],仅有1项研究表明骨水泥注入量多时椎体强化术后易发生腰背痛[19]。 (3)骨水泥分布:15项研究报道了患者骨水泥分布[4-5,7-8,10-11,13-16,18-20,22-23], 其中15项研究报道了单因素分析的结 果[4-5,7-8,10-11,13-16,18-20,22-23],Meta分析显示研究之间无异质性:I2= 0.0%,P=0.997 > 0.1,采用固定效应模型进行分析结果示,OR=2.71,95%CI:2.25-3.26,P=0.00);15项研究报道了多因素分析的结 果[4-5,7-8,10-11,13-16,18-20,22-23],Meta分析显示各研究之间存在低度异质性:I2= 20.5%,P=0.225 > 0.1,采用固定效应模型进行分析结果示 (OR=2.38,95%CI:1.93-2.93,P=0.00)。结果提示骨水泥分布不满意是OVCF患者椎体强化术后发生腰背痛的独立危险因素(表2,图6B)。 (4)骨水泥泄漏:12项研究报道了患者骨水泥泄漏[4,7-8,10-13,15,17,22-24],经过异质性检验,I2=26.8%,且Q检验P=0.181 > 0.1,各研究间异质性较低,进一步敏感性分析表明结果不稳定,放弃随机效应模型的定量分析,使用定性系统评价,10项研究均报道骨水泥渗漏与椎体强化术后腰背痛的发生无 关[4,7-8,11-13,15,17,22,24],仅有2项研究表明骨水泥渗漏发生椎体强化术后易产生腰背痛[10,23]。 (5)椎体骨折数:9项研究报道了患者骨折椎体数[5-6,10,14,18-20,23-24],经过异质性检验,I2=47.2%,P=0.056 < 0.1,各研究间有中度异质性,按照分析类型进行亚组分析,各组内异质性较低,整体存在中度异质性,说明分析类型为异质性来源,多因素分析亚组(OR=3.50,95%CI:2.65-4.62,P=0.00);单因素分析亚组(OR=1.33,95%CI:0.51-3.44,P=0.561);综合结果(OR=2.84,95%CI:1.93-4.19,P=0.00),两亚组分析结果出现差异,由于多因素分析证据等级高于单因素分析,且各研究间无异质性,以多因素分析亚组结果为准,提示骨折椎体数较多是OVCF患者椎体强化术后发生腰背痛的独立危险因素(表2,图6C)。 (6)手术入路:7研究报道了患者手术入路[8,10,13,18-20,23],经过异质性检验,I2=0.00%,且Q检验P=0.833 > 0.1,各研究间无异质性,采用固定效应模型进行Meta分析结果示,OR=1.00,95%CI:0.77-1.31,P=0.979,提示手术入路与OVCF患者椎体强化术后发生腰背痛无关(表2)。"
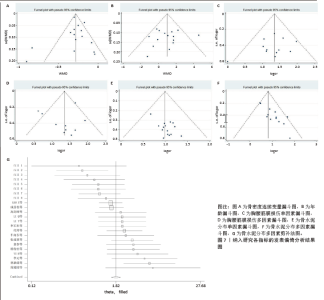
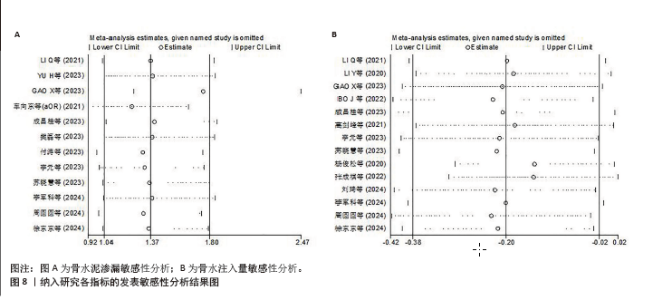
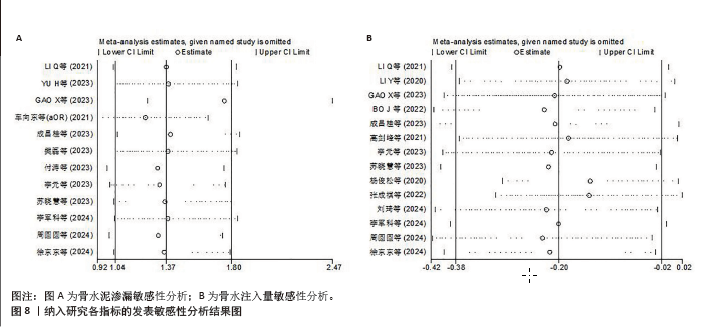
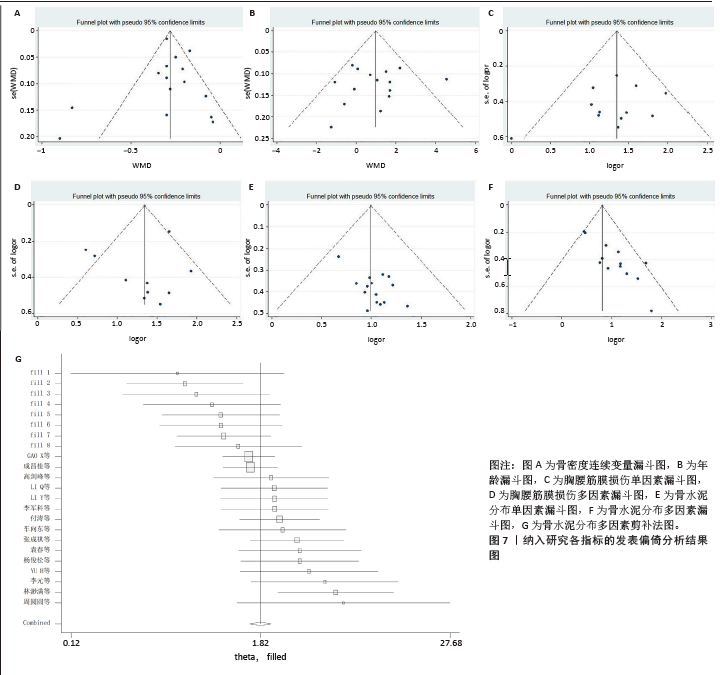
2.3.4 发表偏倚性评价及敏感性分析 对年龄、骨水泥分布、胸腰筋膜损伤、骨密度的发表偏倚进行评估,结果显示,胸腰筋膜损伤、骨密度、年龄Begg’s检验与Egger’s检验结果均为P > 0.05,提示漏斗图对称,不存在显著发表偏倚。骨水泥分布Begg’s检验结果显示P=0.010 < 0.05;Egger’s检验结果显示P=0 < 0.05,表明漏斗图不对称,存在较多异常值,通过剪补法估计缺失了8项研究,纳入8篇虚拟研究的数据后,分析结果未发生反转,提示分析结果稳定。然而,由于所纳入的文献均来自中国,可能存在一定的地区偏倚。对多个变量年龄、性别(女)、体质量指数(≥24 kg/m2)、手术入路、骨水泥分布、胸腰筋膜损伤、骨密度、骨折椎体数逐一剔除各项研究后进行敏感性分析,结果均未改变,提示整体结果稳定。对于骨水泥渗漏和骨水泥注入量,敏感性分析结果显示不稳定,因此决定放弃随机效应定量分析,转而采用定性系统评价(图7,8)。"
| [1] 丁悦, 张嘉, 岳华,等. 骨质疏松性椎体压缩性骨折诊疗与管理专家共识[J]. 中华骨质疏松和骨矿盐疾病杂志,2018,11(5):425-437. [2] 杜宇康, 廖瑛扬, 肖淼盛,等. 经皮椎体成形术与经皮椎体后突成形术治疗骨质疏松性椎体压缩骨折的疗效对比分析[J]. 中国矫形外科杂志, 2014,22(10):946-948. [3] STANG A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603-605. [4] LI Q, SHI L, WANG Y, et al. A Nomogram for Predicting the Residual Back Pain after Percutaneous Vertebroplasty for Osteoporotic Vertebral Compression Fractures. Pain Res Manag. 2021;2021:3624614. [5] LI Y, YUE J, HUANG M, et al. Risk factors for postoperative residual back pain after percutaneous kyphoplasty for osteoporotic vertebral compression fractures. Eur Spine J. 2020;29(10):2568-2575. [6] LIU Z, ZHANG X, LIU H, et al. A nomogram for short-term recurrent pain after percutaneous vertebroplasty for osteoporotic vertebral compression fractures. Osteoporos Int. 2022; 33(4):851-860. [7] YU H, LUO G, WANG Z, et al. Predictors of residual low back pain in patients with osteoporotic vertebral fractures following percutaneous kyphoplasty. Front Surg. 2023;10:1119393. [8] GAO X, DU J, HAO D, et al. Risk factors for residual back pain following percutaneous vertebral augmentation: the importance of paraspinal muscle fatty degeneration. Int Orthop. 2023;47(7):1797-1804. [9] BO J, ZHAO X, HUA Z, et al. Impact of sarcopenia and sagittal parameters on the residual back pain after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fracture. J Orthop Surg Res. 2022;17(1):111. [10] 车向东, 李茂山, 张战峰. PKP术治疗骨质疏松性胸腰椎压缩性骨折残余腰背疼痛的危险因素分析[J]. 颈腰痛杂志,2021,42(1):63-65+69. [11] 成昌桂, 高增鑫, 陈优民,等. 骨质疏松性椎体压缩性骨折经皮椎体成形术后残余腰背痛风险列线图模型的构建与验证[J]. 实用临床医药杂志,2023,27(12):38-43. [12] 樊磊. 骨质疏松性椎体骨折PKP术后残留疼痛程度的影响因素分析[J]. 系统医学,2023,8(14): 85-88. [13] 付涛, 钟炎伟, 于金华. 骨质疏松性腰椎骨折PVP术后慢性腰痛危险因素调查[J]. 颈腰痛杂志,2023,44(4):672-673+676. [14] 高剑峰, 袁景, 沈文东,等. 经皮椎体后凸成形术后残余腰背痛的危险因素分析[J]. 现代医学,2021,49(11):1297-1302. [15] 李元, 李立平, 李强. PKP治疗骨质疏松性椎体压缩骨折早期疼痛缓解不佳相关因素分析[J]. 实用骨科杂志,2023,29(5):390-394. [16] 林渺满, 文雪梅, 黄宗伟,等. 骨质疏松性椎体压缩骨折椎体强化术后残余腰背痛风险预测模型的构建与验证[J]. 中国脊柱脊髓杂志, 2022,32(8):720-728. [17] 苏晓慧, 芮晶晶, 陈文月,等. 骨质疏松性椎体压缩骨折经皮椎体强化术后并发残余腰背痛的危险因素[J]. 临床与病理杂志,2023,43(7): 1384-1391. [18] 杨俊松, 陈浩, 刘鹏,等. 经皮椎体成形术治疗胸腰椎骨质疏松性椎体压缩骨折疗效不佳的多因素分析[J]. 中国脊柱脊髓杂志,2020,30(1): 45-52. [19] 袁春, 缪伟, 唐文凯,等. PVP治疗骨质疏松性椎体压缩骨折术后持续腰背疼痛的影响因素分析[J]. 中国骨与关节损伤杂志,2021,36(9): 956-958. [20] 张成祺, 裴济民, 赵永辉,等. PVP术后早期残留腰背痛的风险因素分析[J]. 颈腰痛杂志, 2022,43(2):204-207. [21] 刘琦, 钱军, 张岚,等. OVCF患者PVP术后肌肉减少和矢状面参数对残余背痛的影响[J]. 颈腰痛杂志,2024,45(2):311-314. [22] 李军科, 马续彬, 李亮,等. 预测骨质疏松性椎体压缩骨折经皮椎体成形术后残余背痛的列线图[J]. 中国骨伤,2024,37(6):553-559. [23] 周圆圆, 张玲敏, 袁之木. 老年骨质疏松性胸腰椎压缩骨折患者术后残余腰背痛影响因素及预测模型的构建分析[J]. 颈腰痛杂志,2024, 45(1): 101-106. [24] 徐东东, 张坚若, 何戟锋. 经皮椎体强化治疗胸腰椎OVCF患者术后残余痛发生危险因素分析[J]. 浙江创伤外科,2024,29(5):857-859. [25] 陈莹, 盛珺, 刘达,等. 唑来膦酸改善骨质疏松患者后路腰椎椎间融合术后腰痛[J]. 脊柱外科杂志,2019,17(5):319-323. [26] 李智斐, 付拴虎, 张家立,等. 椎体成形术后再骨折相关因素分析[J]. 中国脊柱脊髓杂志, 2014,24(9):790-794. [27] 金军伟, 赵刚, 胡付立. 唑来膦酸静脉滴注联合仙灵骨葆胶囊和醋酸钙胶囊口服对骨质疏松性椎体压缩骨折经皮椎体成形术后疗效和安全性的影响[J]. 中医正骨,2019,31(7):15-20. [28] 杨鑫, 皮文杰, 李素铠. 经皮穿刺椎体成形术后余椎新发骨折的风险因素分析[J]. 重庆医学, 2024,53(18):2793-2798,2803. [29] PRESTWOOD KM, KENNY AM. Osteoporosis: pathogenesis, diagnosis, and treatment in older adults. Clin Geriatr Med. 1998;14(3):577-599. [30] 钟远鸣, 张翼升, 李智斐,等. 胸腰椎骨质疏松骨折时间与PVP术后临床疗效相关性的研究[J]. 重庆医学,2018,47(32):4134-4138. [31] YAN Y, XU R, ZOU T. Is thoracolumbar fascia injury the cause of residual back pain after percutaneous vertebroplasty? A prospective cohort study. Osteoporos Int. 2015;26(3): 1119-1124. [32] YANG JS, LIU JJ, CHU L, et al. Causes of Residual Back Pain at Early Stage After Percutaneous Vertebroplasty: A Retrospective Analysis of 1,316 Cases. Pain Physician. 2019;22(5):E495-E503. [33] 万广, 杨慧, 吴大鹏,等. 脊柱-骨盆参数对椎体成形术效果的影响[J]. 中国矫形外科杂志, 2020,28(16):1472-1476. [34] 董洲, 陶晖, 刘艺明,等. 脊柱-骨盆矢状面平衡状态与骨质疏松性椎体压缩性骨折经皮球囊扩张椎体后凸成形效果的关系[J]. 中国组织工程研究,2023,27(29):4635-4640. [35] 刘长枫, 宋文慧, 刘昌文,等. 经皮椎体成形术骨水泥分布评价及影响因素分析[J]. 中国脊柱脊髓杂志,2019,29(11):1001-1008. [36] WIGGINS MC, SEHIZADEH M, PILGRAM TK, et al. Importance of intravertebral fracture clefts in vertebroplasty outcome. AJR Am J Roentgenol. 2007;188(3):634-640. [37] 付兆宗, 陈忠羡, 秦英,等. 骨水泥分布指数对椎体成形术后症状性邻近节段骨折的影响[J]. 南方医科大学学报,2017,37(7):947-951. [38] 蔡明, 戚颖, 刘肃,等. 骨水泥不同分布对骨质疏松性椎体压缩性骨折的生物力学影响:三维有限元分析[J]. 中国医学物理学杂志, 2022,39(6):771-777. [39] LIU H, ZHANG J, LIANG X, et al. Distribution Pattern Making Sense: Patients Achieve Rapider Pain Relief with Confluent Rather Than Separated Bilateral Cement in Percutaneous Kyphoplasty for Osteoporotic Vertebral Compression Fractures. World Neurosurg. 2019;126:e1190-e1196. [40] BRIGGS AM, WRIGLEY TV, VAN DIEËN JH, et al. The effect of osteoporotic vertebral fracture on predicted spinal loads in vivo. Eur Spine J. 2006; 15(12):1785-1795. [41] HE X, LI H, MENG Y, et al. Percutaneous Kyphoplasty Evaluated by Cement Volume and Distribution: An Analysis of Clinical Data. Pain Physician. 2016;19(7):495-506. [42] HUANG S, ZHU X, XIAO D, et al. Therapeutic effect of percutaneous kyphoplasty combined with anti-osteoporosis drug on postmenopausal women with osteoporotic vertebral compression fracture and analysis of postoperative bone cement leakage risk factors: a retrospective cohort study. J Orthop Surg Res. 2019;14(1):452. [43] FU Z, HU X, WU Y, et al. Is There a Dose-Response Relationship of Cement Volume With Cement Leakage and Pain Relief After Vertebroplasty? Dose Response. 2016;14(4):1559325816682867. [44] REN HL, JIANG JM, CHEN JT, et al. Risk factors of new symptomatic vertebral compression fractures in osteoporotic patients undergone percutaneous vertebroplasty. Eur Spine J. 2015; 24(4):750-758. [45] LI K, YAN J, YANG Q, et al. The effect of void creation prior to vertebroplasty on intravertebral pressure and cement distribution in cadaveric spines with simulated metastases. J Orthop Surg Res. 2015;10:20. [46] LIEBSCHNER MA, ROSENBERG WS, KEAVENY TM. Effects of bone cement volume and distribution on vertebral stiffness after vertebroplasty. Spine (Phila Pa 1976). 2001; 26(14):1547-1554. [47] LUO J, DAINES L, CHARALAMBOUS A, et al. Vertebroplasty: only small cement volumes are required to normalize stress distributions on the vertebral bodies. Spine (Phila Pa 1976). 2009;34(26):2865-2873. [48] ZHU SY, ZHONG ZM, WU Q, et al. Risk factors for bone cement leakage in percutaneous vertebroplasty: a retrospective study of four hundred and eighty five patients. Int Orthop. 2016;40(6):1205-1210. [49] MANSOORINASAB M, ABDOLHOSEINPOUR H. A review and update of vertebral fractures due to metastatic tumors of various sites to the spine: Percutaneous vertebroplasty. Interv Med Appl Sci. 2018;10(1):1-6. [50] KIM WJ, MA SB, SHIN HM, et al. Correlation of Sagittal Imbalance and Recollapse after Percutaneous Vertebroplasty for Thoracolumbar Osteoporotic Vertebral Compression Fracture: A Multivariate Study of Risk Factors. Asian Spine J. 2022;16(2):231-240. [51] AHMADI SA, TAKAHASHI S, HOSHINO M, et al. Association between MRI findings and back pain after osteoporotic vertebral fractures: a multicenter prospective cohort study. Spine J. 2019;19(7):1186-1193. [52] 王华锋, 叶小伟, 周福山,等. PVP术后有症状椎管内骨水泥渗漏的诊治并文献回顾[J]. 中国骨与关节损伤杂志,2019,34(5):499-501. |
| [1] | Sun Yajie, Zhao Xinchen, Bo Shuangling. Spatiotemporal expression of bone morphologic protein 7 in mouse kidney development [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1156-1161. |
| [2] | Li Haojing, Wang Xin, Song Chenglin, Zhang Shengnan, Chen Yunxin. Therapeutic efficacy of extracorporeal shock wave therapy in the upper trapezius muscle area combined with exercise control training in patients with chronic non-specific neck pain [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1162-1170. |
| [3] | Liu Yu, Lei Senlin, Zhou Jintao, Liu Hui, Li Xianhui. Mechanisms by which aerobic and resistance exercises improve obesity-related cognitive impairment [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1171-1183. |
| [4] | Yu Huifen, Mo Licun, Cheng Leping. The position and role of 5-hydroxytryptamine in the repair of tissue injury [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1196-1206. |
| [5] | Wang Zhengye, Liu Wanlin, Zhao Zhenqun. Advance in the mechanisms underlying miRNAs in steroid-induced osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1207-1214. |
| [6] | Bu Yangyang, Ning Xinli, Zhao Chen. Intra-articular injections for the treatment of osteoarthritis of the temporomandibular joint: different drugs with multiple combined treatment options [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1215-1224. |
| [7] | Wen Fan, Xiang Yang, Zhu Huan, Tuo Yanfang, Li Feng. Exercise improves microvascular function in patients with type 2 diabetes [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1225-1235. |
| [8] | Liu Xinyue, Li Chunnian, Li Yizhuo, Xu Shifang. Regeneration and repair of oral alveolar bone defects [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1247-1259. |
| [9] | Zheng Yin, Wu Zhenhua, Zhang Cheng, Ruan Kexin, Gang Xiaolin, Ji Hong. Safety and efficacy of immunoadsorption therapy for rheumatoid arthritis: a network meta-analysis and systematic review [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1260-1268. |
| [10] | Chen Qiang, Wu Wenjuan, Jiang Shuhua, Huang Da. Physical exercise improves physical function in burn patients: a systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1269-1281. |
| [11] | Leng Xiaoxuan, Zhao Yuxin, Liu Xihua. Effects of different neuromodulatory stimulation modalities on non-motor symptoms in Parkinson’s patients: a network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1282-1293. |
| [12] | Wen Xiaolong, Weng Xiquan, Feng Yao, Cao Wenyan, Liu Yuqian, Wang Haitao. Effects of inflammation on serum hepcidin and iron metabolism related parameters in patients with type 2 diabetes mellitus: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1294-1301. |
| [13] | Yang Zeyu, Zhi Liang, Wang Jia, Zhang Jingyi, Zhang Qingfang, Wang Yulong, Long Jianjun. A visualized analysis of research hotspots in high-frequency repetitive transcranial magnetic stimulation from the macroscopic perspective [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1320-1330. |
| [14] | Yang Zhijie, Zhao Rui, Yang Haolin, Li Xiaoyun, Li Yangbo, Huang Jiachun, Lin Yanping, Wan Lei, HuangHongxing. Postmenopausal osteoporosis: predictive values of muscle mass, grip strength, and appendicular skeletal muscle index [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1073-1080. |
| [15] | Yin Yongcheng, Zhao Xiangrui, Yang Zhijie, Li Zheng, Li Fang, Ning Bin. Effect and mechanism of peroxiredoxin 1 in microglial inflammation after spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1106-1113. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||