Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (9): 1890-1896.doi: 10.12307/2025.147
Previous Articles Next Articles
Application of bilateral hip magnetic resonance imaging to predict risk of osteonecrosis of femoral head
Jin Jiming1, 2, Hao Yangquan2, Zhao Rushun1, 2, Zhang Yuting2, Jiang Yonghong2, Xu Peng2, Lu Chao2
- 1Shaanxi University of Chinese Medicine, Xianyang 712000, Shaanxi Province, China; 2Honghui Hospital Affiliated to Xi’an Jiaotong University, Xi’an 710054, Shaanxi Province, China
-
Received:2024-01-05Accepted:2024-03-09Online:2025-03-28Published:2024-10-10 -
Contact:Lu Chao, MD, Associate chief physician, Master’s supervisor, Honghui Hospital Affiliated to Xi’an Jiaotong University, Xi’an 710054, Shaanxi Province, China -
About author:Jin Jiming, Master candidate, Shaanxi University of Chinese Medicine, Xianyang 712000, Shaanxi Province, China; Honghui Hospital Affiliated to Xi’an Jiaotong University, Xi’an 710054, Shaanxi Province, China -
Supported by:China Postdoctoral Science Foundation, No. 2017M613179 (to LC); Shaanxi Provincial Administration of Traditional Chinese Medicine Clinical Collaborative Innovation Project, No. 2020-ZXY-010 (to HYQ)
CLC Number:
Cite this article
Jin Jiming, Hao Yangquan, Zhao Rushun, Zhang Yuting, Jiang Yonghong, Xu Peng, Lu Chao. Application of bilateral hip magnetic resonance imaging to predict risk of osteonecrosis of femoral head[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1890-1896.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
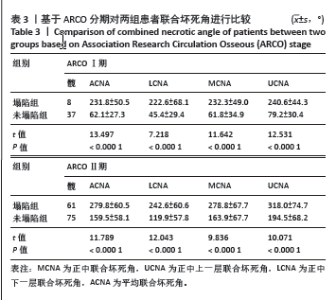
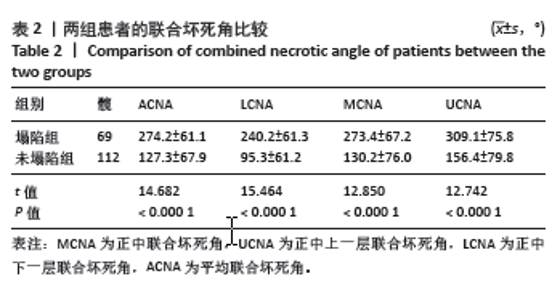
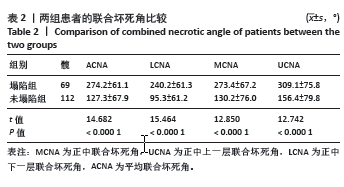
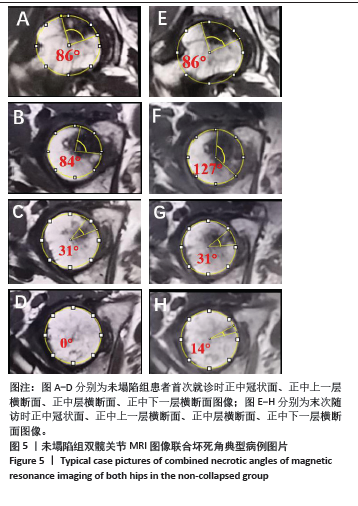
2.5 基于ARCO分期对两组患者坏死角进行比较 由上述结果可知,ARCO分期与联合坏死角均与股骨头塌陷具有相关性,故此次研究对ARCOⅠ期与Ⅱ期的患者与联合坏死角分别进行相关性分析,结果如表3所示。在ARCOⅠ期患者中,未塌陷组中ACNA、LCNA、MCNA、UCNA的平均值分别为62.1°,45.4°,61.76°,79.2°;塌陷组中ACNA、LCNA、MCNA、UCNA的平均值分别为231.8°,222.6°,232.3°,240.6°,且差异均有显著性意义(P < 0.000 1)。在ARCOⅡ期患者中,未塌陷组中ACNA、LCNA、MCNA、UCNA的平均值分别为159.5°,119.9°,163.9°,194.5°;塌陷组中ACNA、LCNA、MCNA、UCNA的平均值分别为279.8°,242.6°,278.8°,318.0°,且差异均有显著性意义(P < 0.000 1)。"
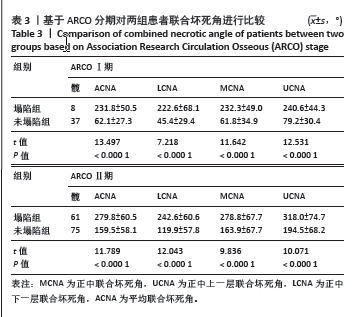
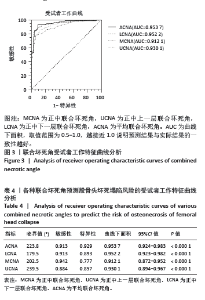
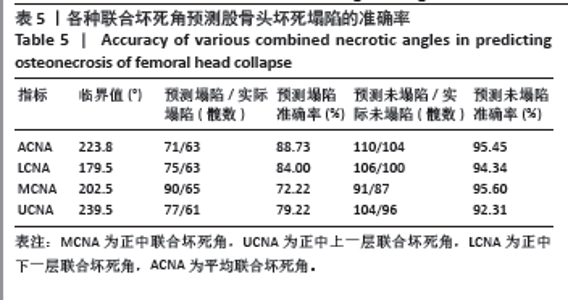
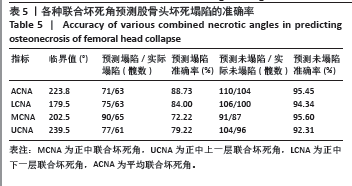
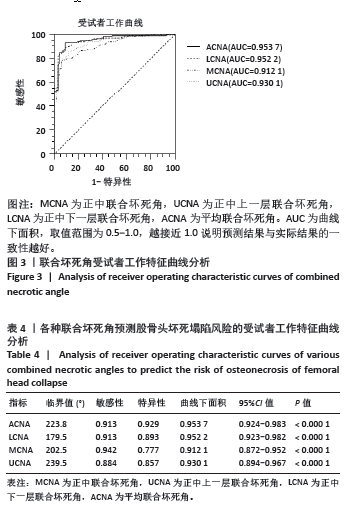
2.6 股骨头联合坏死角对股骨头坏死塌陷风险的预测价值 由于ARCOⅠ期样本量较少,且ARCOⅠ、Ⅱ期患者中塌陷组与未塌陷组在联合坏死角方面差异均有显著性意义,故将ARCOⅠ、Ⅱ期患者同时进行受试者工作特征分析。 图3及表4结果显示,受试者工作特征曲线中ACNA的临界值为223.8°(敏感性=91.3%,特异性=92.9%),即ACNA≥223.8°时与塌陷显著相关(对数秩检验:P < 0.000 1);LCNA的临界值为179.5°(敏感性=91.3%,特异性=89.3%),即LCNA≥179.5°时与塌陷显著相关(对数秩检验:P < 0.000 1);MCNA的临界值为202.5°(敏感性=94.2%,特异性=77.7%),即MCNA≥202.5°时与塌陷显著相关(对数秩检验:P < 0.000 1);UCNA的临界值为239.5°(敏感性=88.4%,特异性=85.7%),即UCNA≥239.5°时与塌陷显著相关(对数秩检验:P < 0.000 1)。"
| [1] ZHAO D, ZHANG F, WANG B, et al. Guidelines for clinical diagnosis and treatment of osteonecrosis of the femoral head in adults (2019 version). J Orthop Translat. 2020;21:100-110. [2] HINES JT, JO WL, CUI Q, et al. Osteonecrosis of the Femoral Head: an Updated Review of ARCO on Pathogenesis, Staging and Treatment. J Korean Med Sci. 2021;36(24):e177. [3] CHEN Y, MIAO Y, LIU K, et al. Evolutionary course of the femoral head osteonecrosis: Histopathological - radiologic characteristics and clinical staging systems. J Orthop Translat. 2022;32:28-40. [4] 何伟. 如何把握股骨头坏死患者的保髋治疗时机[J]. 中国骨与关节杂志,2016,5(2):82-86. [5] MONT MA, SALEM HS, PIUZZI NS, et al. Nontraumatic Osteonecrosis of the Femoral Head: Where Do We Stand Today: A 5-Year Update. J Bone Joint Surg Am. 2020;102(12):1084-1099. [6] KERBOUL M, THOMINE J, POSTEL M, et al. The conservative surgical treatment of idiopathic aseptic necrosis of the femoral head. J Bone Joint Surg Br. 1974;56(2):291-296. [7] SHEN X, LUO J, TANG X, et al. Deep Learning Approach for Diagnosing Early Osteonecrosis of the Femoral Head Based on Magnetic Resonance Imaging. J Arthroplasty. 2023;38(10):2044-2050. [8] 孙伟, 高福强, 李子荣. 股骨头坏死临床诊疗技术专家共识(2022年)[J]. 中国修复重建外科杂志,2022,36(11):1319-1326. [9] KARANTANAS AH, DRAKONAKI EE. The role of MR imaging in avascular necrosis of the femoral head. Semin Musculoskelet Radiol. 2011;15(3): 281-300. [10] KOO KH, KIM R. Quantifying the extent of osteonecrosis of the femoral head. A new method using MRI. J Bone Joint Surg Br. 1995;77(6):875-880. [11] HA YC, JUNG WH, KIM JR, et al. Prediction of collapse in femoral head osteonecrosis: a modified Kerboul method with use of magnetic resonance images. J Bone Joint Surg Am. 2006;88 Suppl 3:35-40. [12] KUBO Y, MOTOMURA G, IKEMURA S, et al. The effect of the anterior boundary of necrotic lesion on the occurrence of collapse in osteonecrosis of the femoral head. Int Orthop. 2018;42(7):1449-1455. [13] 王秋霞, 史传道, 张高魁, 等. 基于股骨头坏死数据库分析成人股骨头坏死误诊相关因素[J]. 临床误诊误治,2020,33(2):4-9. [14] FAN Y, ZHANG J, CHEN M, et al. Diagnostic value of necrotic lesion boundary in bone collapse of femoral head osteonecrosis. Int Orthop. 2022;46(3):423-431. [15] IKEMURA S, MOTOMURA G, KAWANO K, et al. The Discrepancy in the Posterior Boundary of Necrotic Lesion Between Axial and Oblique Axial Slices of MRI in Patients with Osteonecrosis of the Femoral Head. J Bone Joint Surg Am. 2022;104(Suppl 2):33-39. [16] KOLB AR, PATSCH JM, VOGL WD, et al. The role of the subchondral layer in osteonecrosis of the femoral head: analysis based on HR-QCT in comparison to MRI findings. Acta Radiol. 2019;60(4):501-508. [17] LIU LH, LI ZR, SUN W, et al. Reliability and Repeatability of the China-Japan Friendship Hospital Typing Classification for Nontraumatic Osteonecrosis of the Femoral Head. J Bone Joint Surg Am. 2022; 104(Suppl 2):40-46. [18] WEI QS, LI ZQ, HONG ZN, et al. Predicting Collapse in Osteonecrosis of the Femoral Head Using a New Method: Preserved Angles of Anterior and Lateral Femoral Head. J Bone Joint Surg Am. 2022;104(Suppl 2): 47-53. [19] YUE Y, YANG H, LI Y, et al. Combining ultrasonic and computed tomography scanning to characterize mechanical properties of cancellous bone in necrotic human femoral heads. Med Eng Phys. 2019;66:12-17. [20] CHI Z, WANG S, ZHAO D, et al. Evaluating the Blood Supply of the Femoral Head During Different Stages of Necrosis Using Digital Subtraction Angiography. Orthopedics. 2019;42(2):e210-e215. [21] ZHANG Z, YU T, XIE L, et al. Biomechanical bearing-based typing method for osteonecrosis of the femoral head: ABC typing. Exp Ther Med. 2018;16(3):2682-2688. [22] MA J, GE J, CHENG L, et al. Subchondral Bone Plate Classification: A New and More Sensitive Approach for Predicting the Prognosis of Osteonecrosis of the Femoral Head. Cartilage. 2023;14(3):269-277. [23] FENG W, YE P, NI S, et al. One-stage simultaneous hip-preserving surgeries for the management of bilateral femoral head osteonecrosis: a mean 7.0-year follow-up. J Orthop Surg Res. 2019; 14(1):455. [24] TAN B, LI W, ZENG P, et al. Epidemiological Study Based on China Osteonecrosis of the Femoral Head Database. Orthop Surg. 2021; 13(1):153-160. [25] STEINBERG ME, OH SC, KHOURY V, et al. Lesion size measurement in femoral head necrosis. Int Orthop. 2018;42(7):1585-1591. [26] HATANAKA H, MOTOMURA G, IKEMURA S, et al. Differences in magnetic resonance findings between symptomatic and asymptomatic pre-collapse osteonecrosis of the femoral head. Eur J Radiol. 2019; 112:1-6. [27] HINDOYAN KN, LIEBERMAN JR, MATCUK GR, JR, et al. A Precise and Reliable Method of Determining Lesion Size in Osteonecrosis of the Femoral Head Using Volumes. J Arthroplasty. 2020;35(1):285-290. [28] BOONTANAPIBUL K, HUDDLESTON JI, 3RD, AMANATULLAH DF, et al. Modified Kerboul Angle Predicts Outcome of Core Decompression With or Without Additional Cell Therapy. J Arthroplasty. 2021;36(6): 1879-1886. [29] 赵汝顺, 郝阳泉, 许鹏, 等. 不同坏死病灶位置对非创伤性股骨头坏死自然病程的影响[J]. 中国组织工程研究,2024,28(6) 917-921. [30] 鲁超, 刘洪智, 刘道兵, 等. 股骨头坏死病灶分布规律探讨 [J]. 中国矫形外科杂志,2014,22(5):396-400. [31] IKEMURA S, MAWATARI T, MATSUI G, et al. The depth of the low-intensity band on the T1-weighted MR image is useful for distinguishing subchondral insufficiency fracture from osteonecrosis of the collapsed femoral head. Arch Orthop Trauma Surg. 2018; 138(8):1053-1058. [32] LAVERNIA CJ, SIERRA RJ. Core decompression in atraumatic osteonecrosis of the hip. J Arthroplasty. 2000;15(2):171-178. [33] 魏秋实, 何伟, 张庆文, 等. 岭南袁氏中医药防治股骨头坏死传承文化研究[J]. 新中医,2022,54(23):216-220. [34] SAI KRISHNA MLV, KAR S, KUMAR R, et al. The Role of Conservative Management in the Avascular Necrosis of the Femoral Head: A Review of Systematic Reviews. Indian J Orthop. 2023;57(3):410-420. [35] 张磊, 金红婷, 童培建. 骨健口服液早期干预非创伤性股骨头坏死的临床研究[J]. 中医正骨,2016,28(3):14-19. [36] AGARWALA S, BANAVALI SD, VIJAYVARGIYA M. Bisphosphonate Combination Therapy in the Management of Postchemotherapy Avascular Necrosis of the Femoral Head in Adolescents and Young Adults: A Retrospective Study From India. J Glob Oncol. 2018;4:1-11. |
| [1] | Zhou Jiajun, Ma Fei, Leng Yebo, Xu Shicai, He Baoqiang, Li Yang, Liao Yehui, Tang Qiang, Tang Chao, Wang Qing, Zhong Dejun. Assessing distribution characteristics and clinical significance of vertebral fractures in patients with osteoporosis based on whole spine MRI [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1883-1889. |
| [2] | Chen Hao, Wu Pigen, Teng Jiaqi, Zhang Liang, Feng Xinmin. Analysis of risk factors for lumbar fascial edema in patients with osteoporotic vertebral compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6174-6179. |
| [3] | Yin Hao, Ji Meiqi, Hu Zhixiang, Wu Han, Lyu Heng, Li Shengyun, Li Lei, Zhai Chuntao, Lyu Yue. Comparison and evaluation of three different methods for preparing rat models of lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(14): 2930-2936. |
| [4] | Hu Zhixing, Li Qun, Yang Chao, Wang Xiaoxiao, Fang Luochangting, Hou Wuqiong, Lin Na, Chen Weiheng, Liu Chunfang, Lin Ya. Network meta-analysis of the modeling effects of different factors on rabbit models of steroid-induced osteonecrosis of femoral head [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 976-984. |
| [5] | Lu Guangqi, Cui Ying, Li Jing, Yu Zhangjingze, Zhu Liguo, Yu Jie, Zhuang Minghui. Feasibility of constructing a diagnostic classification model for cervical instability by magnetic resonance imaging radiomics [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(33): 5370-5374. |
| [6] | Li Yang, Ma Fei, Leng Yebo, Xu Shicai, He Baoqiang, Zhou Jiajun, Liao Yehui, Tang Qiang, Tang Chao, Wang Qing, Zhong Dejun. Correlation between intervertebral disc degeneration and hyperuricemia [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(32): 5091-5096. |
| [7] | Huang Dong, Ge Jin, Liu Guangluan, Guo Zonglei, Wang Yehua. Anatomical risk factors for tibial insertion avulsion fracture of anterior cruciate ligament based on MRI [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(24): 3890-3896. |
| [8] | Yin Yuetong, Zhu Guangyu, Tian Xiangdong, Tan Yetong, Ma Sheng, Xue Zhipeng, Hu Yuanyi, Li Xiaomin. Effects of distal tibial tuberosity-high tibial osteotomy on ankle angle on coronal plane [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(21): 3349-3354. |
| [9] | Yuan Xinwei, Huang Yixuan, Xi Hongzhong, Guo Mingbin, Mai Jianbin, Sun Guangquan, Liu Xin, Du Bin. Effect of three-dimensional spatial distribution of necrotic and support areas on outcomes of fibular support for hip preservation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(18): 2789-2794. |
| [10] | Liu Yanan, Wang Xing, Li Kun, Sun Ruifen, Ma Xueying, Zhao Lei, Liu Yuhang, Yang Yang, Hao Yunteng, Li Ziyu, Zhang Shaojie, Li Zhijun. Digital characteristics of brainstem morphology and age-related development in young children [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(11): 1730-1736. |
| [11] | Xu Xiangjun, Wang Chao, Song Qunshan, Li Bingyan, Zhang Jichao, Wang Guodong, Dong Yuefu. Optimal angle for prosthesis implantation in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 612-618. |
| [12] | Chen Bohao, He Qi, Yang Junzheng, Pan Zhaofeng, Xiao Jiacong, Li Miao, Li Shaocong, Zeng Jiaxu, Wang Haibin, Zheng Jia, Zhang Meng. Significance of Piezo1 protein in the pathogenesis of osteonecrosis of femoral head [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(27): 4414-4420. |
| [13] | Gao Yue, Fu Ziwei, Wu Yanbo, Pan Shinong, Lu Zhao. Clinical and imaging features of slipped capital femoral epiphysis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(27): 4421-4428. |
| [14] | Niu Cehao, Zhang Chunlin, Yan Xu, Fu Su, Feng Yang, Zhu Andi. Posterior vertebral structure and its influence on measurement of disc herniation volume [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(18): 2897-2902. |
| [15] | Gao Yue, Lin Jianwen, Li Di, Lan Xiaoyan, Li Shen, Chu Chengyan. Oligodendrocyte progenitor cells prolong the survival of glioblastoma-bearing rats after high-dose radiotherapy [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(17): 2669-2674. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||