Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (9): 1897-1904.doi: 10.12307/2025.152
Previous Articles Next Articles
Effect of finite element method in treatment of developmental dysplasia of the hip in children
Sun Xiaojun1, 2, Wang Huaming2, Zhang Dehong2, Song Xuewen2, Huang Jin2, Zhang Chen2, Pei Shengtai2
- 1Gansu University of Chinese Medicine, Lanzhou 730000, Gansu Province, China; 2Gansu Provincial Hospital of TCM (First Affiliated Hospital of Gansu University of Chinese Medicine), Lanzhou 730050, Gansu Province, China
-
Received:2023-11-04Accepted:2024-02-22Online:2025-03-28Published:2024-10-11 -
Contact:Wang Huaming, Associate chief physician, Gansu Provincial Hospital of TCM (First Affiliated Hospital of Gansu University of Chinese Medicine), Lanzhou 730050, Gansu Province, China Zhang Dehong, Chief physician, Gansu Provincial Hospital of TCM (First Affiliated Hospital of Gansu University of Chinese Medicine), Lanzhou 730050, Gansu Province, China -
About author:Sun Xiaojun, Master candidate, Gansu University of Chinese Medicine, Lanzhou 730000, Gansu Province, China; Gansu Provincial Hospital of TCM (First Affiliated Hospital of Gansu University of Chinese Medicine), Lanzhou 730050, Gansu Province, China -
Supported by:Natural Science Foundation of Gansu Province, No. 22JR11RA203 (to WHM)
CLC Number:
Cite this article
Sun Xiaojun, Wang Huaming, Zhang Dehong, Song Xuewen, Huang Jin, Zhang Chen, Pei Shengtai. Effect of finite element method in treatment of developmental dysplasia of the hip in children[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1897-1904.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

2.2 有限元模型的建立 目前研究者利用电子计算机断层扫描(CT)、磁共振成像(MRI)所得的图像进行有限元模型的建立。首先将扫描图像数据导入Mimics等软件,选择适宜的灰度值,根据骨骼与软组织成像的差异性,提取出骨骼轮廓,并对图像进行阈值分割、蒙版编辑、区域增长、填充、光滑等等操作后,进行三维重建从而得到最初的髋关节骨骼三维模型。将所建立的模型导入3-matic、 Geomagic studio等软件自动生成面网格,通过优化、过滤网格、填补空洞、拟合曲线等操作,从而创建体网格。在Mimics中赋予材料属性后使用有限元分析软件如 ANSYS、ABAQUS等进行骨骼、关节、软组织、内固定植入物和假体等的力学分析。见图3。"

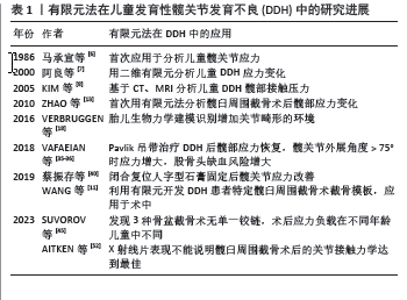
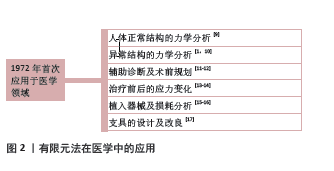
有限元法可基于影像学图像和解剖特征建立高精度人体仿真模型,利用有限的、相互关联的单元对人体复杂的关节进行简化,通过计算得到直观准确的分析结果,能降低分析成本;利用有限元法可以获得在体内无法测量的信息,由于其在虚拟环境中操作,不受时间和伦理的限制,因此在医学领域,尤其是骨科、生物力学等方面有重要应用价值。但有限元建模过程中将人体复杂结构简化再进行分析是固有的局限性;操作过程中影像学资料在不同的软件之间导入、切换,可能导致重要信息丢失,应将软件完善、统一,以便在相似研究之间横向比较;其中材料参数赋值、载荷施加等步骤直接影响结果,如何确保模拟实验前输入参数的准确是一大挑战。 2.3 正常与DDH患者的髋关节力学特点 髋关节是由股骨头和髋臼共同构成球窝关节,连接人体躯干和下肢,是最大的承重关节。与髋关节生物力学有关的力学因素主要是外展肌力和关节反应力,其中关节反应力是外展肌力与身体重力的合力,并作用于髋关节[18-19]。目前相关的有限元研究也证实,髋关节正常负重时,应力均匀分布于股骨头上,而DDH患者髋关节头臼不匹配,股骨头半脱位或全脱位,髋关节力学关系异常,导致外展肌无力、关节软骨磨损加重、髋部疼痛等,进而继发骨关节炎[20-21],CHU等[22]的研究证实DDH患者软骨下骨小梁骨微结构恶化,可能与软骨损伤有关。髋臼盂唇承担了部分髋关节的接触压力,当盂唇撕裂或切除接触压力增加,而修复或重建唇唇后,接触压力降低[23-24]。DDH的发生是由髋关节的先天性发育缺陷和后天的生物力学异常共同作用的[25],这是一个动态变化的过程,髋关节结构在生长发育过程中持续不断进行的不良改变[26-28];在儿童DDH有限元模型中,髋臼与股骨头接触面积减小,应力增大并集中,且股骨颈局部也存在应力集中的情况[29];生长中的骨骼对负荷条件敏感,负荷的变化能影响骨骼的形状和功能,MRI显示儿童DDH股骨头生长发育障碍,通常呈非球形且较健侧小,在复位成功后,可以发生显著的重塑改变,同时治疗的时机与时间长短也非常重要[30-32]。 2.4 DDH各种治疗方法的有限元法研究 0-6个月的DDH患儿使用Pavlik吊带治疗有> 90%的成功率[33-34]。由于婴儿髋关节未完全骨化,MRI相对于X射线片及CT可提供软骨性髋臼指数。VAFAEIAN等[35-36]的研究以MRI图像为基础,为正常婴儿的髋关节建立有限元模型并模拟其在佩戴Pavlik吊带时软骨性髋关节的软骨接触压力,显示髋臼的前部、后部和髋臼上内侧存在马蹄形的应力区域,而上外侧处于无负荷状态,在这种接触压力的分布下髋臼倾斜度增加、髋臼加深,髋臼顶仅承受轻微负荷(正常髋关节)或卸载(发育不良髋关节);研究模拟髋关节在屈曲90°、外展40°、60°和80°时的接触压力,发现随着髋关节外展角度增加(特别是> 75°)则接触压力增大。MáRQUEZ-FLóREZ等[37]的研究也表明,与站立位相比,婴儿处于仰卧髋关节屈曲外展时髋臼面接触力的分布更加均匀;而在极端外展(80°)时髋臼后壁和邻近的外侧股骨头的接触压力有增大和集中的趋势,外侧股骨头上的接触压力可能会减少股骨头血供,从而导致股骨头坏死[38]。HUAYAMAVE等[39]研究Pavlik吊带治疗严重脱位时前倾角在30°-70°之间的生物力学特性,模型分析结果表明减少股骨前倾角可能会增加治疗高度髋关节发育不良的成功率。这些研究从生物力学角度证明了Pavlik吊带治疗成功和DDH并发症发生的潜在生物力学因素。 闭合复位和髋人字石膏固定是6-18月龄DDH患儿的推荐治疗方法。蔡振存等[40]对1例DDH患者“人”字型石膏固定后的髋关节进行有限元分析,结果表明患侧髋关节头与臼间的平均接触压力、最大接触压力、股骨头所受Von Mises应力峰值均高于健侧,患侧头臼接触面积小于健侧。LIU等[41]的研究采用有限元法比较闭合复位治疗前后髋臼和股骨头上Von Mises应力的大小和分布特征,结果显示治疗后髋臼顶部外侧缘和股骨头外侧柱的高应力点消失,应力呈放射状均匀分布并向外周逐渐减弱,髋关节的应力大小和分布与健康侧相似,从而以力学的角度佐证了闭合复位治疗的有效性。ZHANG等[42]对1例右侧DDH的16月龄女性患儿的髋关节进行了三维有限元分析,发现随着髋关节外展角度的增加,髋臼后部的应力明显增加,股骨头外侧的应力也随之增加,闭合复位时髋臼上区软骨接触压力变化不明显,股骨头受压无明显差异,从力学角度说明过度外展时股骨头外侧应力的增加可能与缺血坏死有关,而屈曲角度的增加与之无关。 对于年龄在12-18个月或更大、以及闭合复位失败的患儿,建议采用骨盆截骨术的方式以实现髋关节同心圆复位[43]。NAKAMURA等[44]比较了26例接受Salter骨盆截骨术的女性单侧DDH患者术前术后的CT、MRI三维形态,发现患侧髋臼软骨经手术治疗后改善至正常形态。以往认为Salter截骨以耻骨联合软骨为铰链,Pemberton截骨以Y型软骨为铰链,Dega截骨则以坐骨大切迹后内侧皮质层为铰链;而SUVOROV等[45]使用2岁和6岁患者的健康骨盆CT数据建立模型并模拟这3种骨盆截骨术进行相关生物力学分析,发现在骨盆这个整体单元中,Salter、Dega和Pemberton截骨术没有单一的铰链;Salter截骨术中患侧Y型软骨后支的负载在2岁模型上较大,对侧半骨盆的负载在2岁和6岁的模型中均较大;Pemberton截骨术中,前、后Y型软骨为主要受力部分,对侧耻骨的负载在2岁模型上出现;Dega截骨术以坐骨大切迹区髂后皮质层为主,对侧半骨盆未见负荷。研究同时发现骨盆韧带在骨盆截骨术中发挥着重要的限制作用;年龄的不同对生物力学有影响,2岁患者的骨盆软骨铰链较多,其模型比6岁患者的更“软”,这表明髋臼畸形更易于矫正。TOYOHARA等[46]对髋关节发育不良手术前后骶髂关节应力分布进行分析,结果表明髋臼形态对骶髂关节有影响,髋臼后覆盖的改善可能有助于恢复骨盆的负荷传递,从而改善髋臼发育不良患者骶髂关节的应力环境。 对于早期未得到正规治疗或者漏诊的DDH患者,其髋臼软骨生长中心闭合,X射线片表明髋臼较浅导致股骨头未覆盖,髋关节一致、X射线片上没有关节炎变性的迹象,采用髋臼周围截骨术治疗以改善髋关节疼痛等症状,早期的有限元研究从关节接触面、关节接触压力、股骨的应力等的角度证明髋臼周围截骨术的有效性[47]。PARK等[48]的研究表明髋臼周围截骨术中冠状面旋转是获得最佳临床结果的主要手术参数之一;而近期的一项有限元研究发现仅冠状面矫正可能无法使髋关节生物力学正常化[49];KITAMURA等[50]通过虚拟髋臼周围截骨术操作,将髋臼骨块在冠状面上外旋,使得外侧中心边缘角达到30°,在矢状面上对髋臼骨块分别前旋转0°,5°,10°和15°,对这4个角度的髋臼进行有限元分析,结果表明在不同的前旋角度下,外旋髋臼可使关节接触压力正常化,且进一步的前旋髋臼可以进一步降低关节接触压力。KITAMURA等[51]的另一项研究以51例髋关节发育不良患者的三维髋关节模型分析髋臼周围截骨术前和术后单腿站立期间髋臼软骨的关节接触压力,研究结论是髋臼周围截骨术可以使64.7%的患者关节接触压力恢复正常,但对于具有非球形股骨头的患者,关节接触压力的恢复较困难。随着对该病的认识加深以及相关研究的进一步进展,AITKEN等[52]建立了20例髋臼周围截骨患者术前、术后的髋关节模型,在机械最佳、临床最佳和手术达到的定位之间,比较了X射线影像覆盖范围、接触面积、峰值/平均接触应力等的指标,得出X射线片表现不能说明髋臼周围截骨术后的关节接触力学达到了最佳的结论,对此则需要充分的术前规划、计算机模拟最佳截骨位置、3D打印截骨模板等措施以达到临床最佳[11]。 上述DDH髋关节以及各阶段治疗相关的有限元分析(表1),验证了髋关节发育不良时的应力关系,从力学角度阐释了DDH髋臼及股骨产生异常的原因;对于保守治疗的病例,用有限元的方法验证其治疗的有效性,以及髋关节所处位置的角度,证明了“安全角”的重要意义,“安全角”过小则髋关节复位不稳定,过大则导致髋臼后壁及邻近外侧股骨头的软骨接触压力增大,最终影响股骨头血供。利用有限元方法从力学的角度验证手术治疗有效的原因,同时分析经过手术后骨盆力学关系的变化,以推测预后以及指导康复,并基于模拟实验结果指出存在的不足和需要改进的方向;除此之外,对于需要手术治疗的病例,可以借助有限元法进行术前规划,确定截骨的最佳位置以指导手术操作更加精确,同时可以适当降低手术创伤以及减少术中X射线照射的次数,这对患者是非常有利的。然而这些有限元分析中,较少提及髋臼横韧带、关节囊、肌肉等结构在髋关节中的力学作用,这与有限元建模、参数设置等的难易程度有关,如果在有限元模型中添加韧带、软骨、肌肉等元素,那么必须获得这些组织的3D信息,以及各自准确的材料参数,这是目前需要克服的一大困难。"
| [1] ZHANG H, ZHOU J, GUAN J, et al. How to restore rotation center in total hip arthroplasty for developmental dysplasia of the hip by recognizing the pathomorphology of acetabulum and Harris fossa? J Orthop Surg Res. 2019;14(1):339. [2] WANG Z, LI H, ZHOU Y, et al. Three-dimensional femoral morphology in Hartofilakidis type C developmental dysplastic hips and the implications for total hip arthroplasty. Int Orthop. 2020;44(10):1935-1942. [3] DU Y, LI T, SUN J, et al. The Effect of the False Acetabulum on Femoral Proximal Medullary Canal in Unilateral Crowe Type IV Developmental Dislocation of the Hip. Ther Clin Risk Manag. 2020; 16:631-637. [4] NICHOLSON A, DUNNE K, TAAFFE S, et al. Developmental dysplasia of the hip in infants and children. BMJ. 2023;383:e074507. [5] BREKELMANS WA, POORT HW, SLOOFF TJ. A new method to analyse the mechanical behaviour of skeletal parts. Acta Orthop Scand. 1972; 43(5):301-317. [6] 马承宣,刘贵林,房论光,等.儿童髋关节表面应力分布状态及与髋臼指数的关系[J]. 中华小儿外科杂志,1986,7(1):31-32. [7] 阿良,吉士俊,范慈方.有限元分析先天性髋关节半脱位及髋臼发育不良的应力变化[J].中华小儿外科杂志,2000(6):7-10. [8] KIM YH, PARK WM, CHOI IH. Planning of Shelf Operation in Dysplastic Hip by CT and MRI Based Finite Element Contact Analysis. JSME International Journal Series C. 2005; 48(4):586-591. [9] 陈诺,邱丽华,常晓丹. 基于CT图像马拉松运动员步态周期中髋关节应力分布的有限元分析[J]. 中华放射学杂志,2023,57(12): 1305-1311. [10] 田丰德, 赵德伟, 李东怡, 等. 髋臼缺损程度对成人髋关节应力影响的三维有限元分析[J]. 中国组织工程研究,2018,22(3):380-384. [11] WANG X, LIU S, PENG J, et al. Development of a novel customized cutting and rotating template for Bernese periacetabular osteotomy. J Orthop Surg Res. 2019;14(1):217. [12] CHEN S, ZHANG L, MEI Y, et al. Role of the Anterior Center-Edge Angle on Acetabular Stress Distribution in Borderline Development Dysplastic of Hip Determined by Finite Element Analysis. Front Bioeng Biotechnol. 2022;10:823557. [13] ZHAO X, CHOSA E, TOTORIBE K, et al. Effect of periacetabular osteotomy for acetabular dysplasia clarified by three-dimensional finite element analysis. J Orthop Sci. 2010;15(5):632-640. [14] 张景贺, 窦永峰, 许世东, 等. 有限元模拟单通道分体内镜下双侧腰椎管减压对腰椎生物力学的影响[J]. 中国组织工程研究,2024, 28(12):1849-1854. [15] FEYZI M, FALLAHNEZHAD K, TAYLOR M, et al. A review on the finite element simulation of fretting wear and corrosion in the taper junction of hip replacement implants. Comput Biol Med. 2021;130:104196. [16] CHETHAN KN, SHYAMASUNDER BN, ZUBER M, et al. Finite element analysis of hip implant with varying in taper neck lengths under static loading conditions. Comput Methods Programs Biomed. 2021; 208:106273. [17] 张静, 萨日娜, 嘎拉台. 基于瞬态分析的桡骨远端骨折外固定支具结构优化设计[J]. 医用生物力学,2022,37(5):952-959. [18] VERBRUGGEN SW, LOO JH, HAYAT TT, et al. Modeling the biomechanics of fetal movements. Biomech Model Mechanobiol. 2016;15(4):995-1004. [19] POLKOWSKI GG, CLOHISY JC. Hip biomechanics. Sports Med Arthrosc Rev. 2010;18(2):56-62. [20] DE PIERI E, FRIESENBICHLER B, LIST R, et al. Subject-Specific Modeling of Femoral Torsion Influences the Prediction of Hip Loading During Gait in Asymptomatic Adults. Front Bioeng Biotechnol. 2021;9: 679360. [21] HARRIS MD, SHEPHERD MC, SONG K, et al. The biomechanical disadvantage of dysplastic hips. J Orthop Res. 2022;40(6):1387-1396. [22] CHU L, HE Z, QU X, et al. Different subchondral trabecular bone microstructure and biomechanical properties between developmental dysplasia of the hip and primary osteoarthritis. J Orthop Translat. 2019;22: 50-57. [23] HENAK CR, ABRAHAM CL, ANDERSON AE, et al. Patient-specific analysis of cartilage and labrum mechanics in human hips with acetabular dysplasia. Osteoarthritis Cartilage. 2014;22(2):210-217. [24] DANTAS P, GONCALVES S R, GRENHO A, et al. Hip joint contact pressure and force: a scoping review of in vivo and cadaver studies. Bone Joint Res. 2023;12(12):712-721. [25] SONG K, ANDERSON AE, WEISS JA, et al. Musculoskeletal models with generic and subject-specific geometry estimate different joint biomechanics in dysplastic hips. Comput Methods Biomech Biomed Engin. 2019;22(3):259-270. [26] KLISIC PJ. Congenital dislocation of the hip--a misleading term: brief report. J Bone Joint Surg Br. 1989;71(1):136. [27] LODER RT, SKOPELJA EN. The epidemiology and demographics of hip dysplasia. ISRN Orthop. 2011;2011:238607. [28] KOTLARSKY P, HABER R, BIALIK V, et al. Developmental dysplasia of the hip: What has changed in the last 20 years? World J Orthop. 2015;6(11):886-901. [29] INCZE-BARTHA Z, INCZE-BARTHA S, SIMON SZ, et al. Finite Element Analysis of Normal and Dysplastic Hip Joints in Children. J Pers Med. 2023;13(11):1593. [30] SHIN CH, YOO WJ, PARK MS, et al. Acetabular Remodeling and Role of Osteotomy After Closed Reduction of Developmental Dysplasia of the Hip. J Bone Joint Surg Am. 2016;98(11):952-957. [31] TSUKAGOSHI Y, KAMADA H, TAKEUCHI R, et al. Three-dimensional MRI analyses of prereduced femoral head sphericity in patients with developmental dysplasia of the hip after Pavlik harness failure. J Pediatr Orthop B. 2018;27(5):394-398. [32] SADEGHIAN SM, ARTHURS OJ, LI X, et al. Neonatal Hip Loading in Developmental Dysplasia: Finite Element Simulation of Proximal Femur Growth and Treatment. HSS J. 2023;19(4):418-427. [33] MORALEDA L, ALBIÑANA J, SALCEDO M, et al. Displasia in the development of the hip. Rev Esp Cir Ortop Traumatol. 2013;57(1):67-77. [34] VAQUERO-PICADO A, GONZALEZ-MORAN G, GARAY EG, et al. Developmental dysplasia of the hip: update of management. EFORT Open Rev. 2019;4(9):548-556. [35] VAFAEIAN B, ADEEB S, EL-RICH M, et al. Hip Joint Contact Pressure Distribution During Pavlik Harness Treatment of an Infant Hip: A Patient-Specific Finite Element Model. J Biomech Eng. 2018;140(7). doi: 10.1115/1.4039827. [36] VAFAEIAN B, ADEEB S, EL-RICH M, et al. Prediction of mechanical behavior of cartilaginous infant hips in pavlik harness: A subject-specific simulation study on normal and dysplastic hips. J Orthop Res. 2019;37(3):655-664. [37] MÁRQUEZ-FLÓREZ KM, SILVA O, NARVAEZ-TOVAR CA, et al. A Comparison of the Contact Force Distributions on the Acetabular Surface Due to Orthopedic Treatments for Developmental Hip Dysplasia. J Biomech Eng. 2016;138(7). doi: 10.1115/1.4033547. [38] BOROWSKI A, THAWRANI D, GRISSOM L, et al. Bilaterally dislocated hips treated with the Pavlik harness are not at a higher risk for failure. J Pediatr Orthop. 2009;29(7):661-665. [39] HUAYAMAVE V, LOZINSKI B, ROSE C, et al. Biomechanical evaluation of femoral anteversion in developmental dysplasia of the hip and potential implications for closed reduction. Clin Biomech (Bristol, Avon). 2020;72:179-185. [40] 蔡振存,朴成哲,周宏宇,等.有限元法分析儿童发育不良髋关节“人”字型固定后的应力特征[J]. 中国组织工程研究,2019,23(36): 5841-5845. [41] LIU J, GAO T, LI J, et al. Evaluation of the short-term curative effect of closed reduction in the treatment of developmental dysplasia of the hip based on three-dimensional magnetic resonance imaging finite element analysis. BMC Musculoskelet Disord. 2022;23(1):455. [42] ZHANG Z, SUI D, QIN H, et al. Contact pressure distribution of the hip joint during closed reduction of developmental dysplasia of the hip: a patient-specific finite element analysis. BMC Musculoskelet Disord. 2020;21(1):600. [43] YANG S, ZUSMAN N, LIEBERMAN E, et al. Developmental Dysplasia of the Hip. Pediatrics. 2019;143(1): e20181147. [44] NAKAMURA T, WADA A, NATORI T, et al. A Novel Method for Assessing the 3-dimensional Morphology of Cartilaginous Acetabulum Via Childhood Magnetic Resonance Imaging. J Pediatr Orthop. 2023;43(10): 640-648. [45] SUVOROV V, FILIPCHUK V, MELNYK M. The biomechanical analysis of pelvic osteotomies applied for DDH treatment in pediatric patients. Wiad Lek. 2023;76(8):1804-1812. [46] TOYOHARA R, KANEUJI A, TAKANO N, et al. A patient-cohort study of numerical analysis on sacroiliac joint stress distribution in pre- and post-operative hip dysplasia. Sci Rep. 2022;12(1):14500. [47] LEE KJ, PARK SJ, KWO SY, et al. Biomechanical study on the efficacy of the periacetabular osteotomy using Patient-specific finite element analysis. Int J Precis Eng Man. 2015;16(4):823-829. [48] PARK SJ, LEE SJ, CHEN WM, et al. Computer-Assisted Optimization of the Acetabular Rotation in Periacetabular Osteotomy Using Patient’s Anatomy-Specific Finite Element Analysis. Appl Bionics Biomech. 2018;2018:9730525. [49] KITAMURA K, FUJII M, IWAMOTO M, et al. Effect of coronal plane acetabular correction on joint contact pressure in Periacetabular osteotomy: a finite-element analysis. BMC Musculoskelet Disord. 2022;23(1):48. [50] KITAMURA K, FUJII M, IWAMOTO M, et al. Is Anterior Rotation of the Acetabulum Necessary to Normalize Joint Contact Pressure in Periacetabular Osteotomy? A Finite-element Analysis Study. Clin Orthop Relat Res. 2022; 480(1):67-78. [51] KITAMURA K, FUJII M, IKEMURA S, et al. Factors Associated With Abnormal Joint Contact Pressure After Periacetabular Osteotomy: A Finite-Element Analysis. J Arthroplasty. 2022;37(10):2097-2105. [52] AITKEN HD, MILLER A, RIVAS DJL, et al. Radiographically successful periacetabular osteotomy does not achieve optimal contact mechanics in dysplastic hips. Clin Biomech (Bristol, Avon). 2023;104: 105928. [53] MENG Y, LU Z, ZHANG XL, et al. A short-term magnetic resonance imaging analysis of acetabular adaptation in developmental dysplasia of the hip by open reduction or open reduction combined with Dega osteotomy. Chin Med J (Engl). 2021;134(13):1619-1621. [54] FU Z, ZHANG Z, DENG S, et al. MRI assessment of femoral head docking following closed reduction of developmental dysplasia of the hip. Bone Joint J. 2023;105-B(2):140-147. [55] HASEGAWA K, KABATA T, KAJINO Y, et al. The influence of pelvic tilt on stress distribution in the acetabulum: finite element analysis. BMC Musculoskelet Disord. 2021;22(1):764. [56] LI J. Development and validation of a finite-element musculoskeletal model incorporating a deformable contact model of the hip joint during gait. J Mech Behav Biomed Mater. 2021;113:104136. [57] GAO Y, CHAI W, AN Z, et al. Effect of Hip Joint Center on Multi-body Dynamics and Contact Mechanics of Hip Arthroplasty for Crowe IV Dysplasia. Orthop Surg. 2022;14(11):3061-3069. [58] MOSHFEGHIFAR F, GHOLAMALIZADEH T, FERGUSON Z, et al. LibHip: An open-access hip joint model repository suitable for finite element method simulation. Comput Methods Programs Biomed. 2022;226:107140. [59] DU Y, FU J, SUN J, et al. Acetabular Bone Defect in Total Hip Arthroplasty for Crowe II or III Developmental Dysplasia of the Hip: A Finite Element Study. Biomed Res Int. 2020 Aug 25;2020:4809013. [60] INCZE-BARTHA Z, INCZE-BARTHA S, SIMON-SZABÓ Z, et al. Finite Element Analysis of Various Osteotomies Used in the Treatment of Developmental Hip Dysplasia in Children. J Pers Med. 2024; 14(2):189. [61] VAFAEIAN B, ZONOOBI D, MABEE M, et al. Finite element analysis of mechanical behavior of human dysplastic hip joints: a systematic review. Osteoarthritis Cartilage. 2017;25(4):438-447. [62] IKE H, INABA Y, KOBAYASHI N, et al. Effects of rotational acetabular osteotomy on the mechanical stress within the hip joint in patients with developmental dysplasia of the hip: a subject-specific finite element analysis. Bone Joint J. 2015;97-B(4):492-497. |
| [1] | Xu Hao, Ding Lu, Li Xiao. Investigating the effect of the mechanical wear on abutment screw in Morse taper connection implant implant system by using finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [2] | Li Liangkui, Huang Yongcan, Wang Peng, Yu Binsheng. Effect of anterior controllable anteriodisplacement and fusion on vertebrae-ossification of posterior longitudinal ligament complex and implants: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1761-1767. |
| [3] | Xu Biao, Lu Tan, Jiang Yaqiong, Yin Yujiao. Xu Biao, Lu Tan, Jiang Yaqiong, Yin Yujiao [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1768-1774. |
| [4] | Zhou Jinhai, Li Jiangwei, Wang Xuquan, Zhuang Ying, Zhao Ying, Yang Yuyong, Wang Jiajia, Yang Yang, Zhou Shilian. Three-dimensional finite element analysis of anterior femoral notching during total knee arthroplasty at different bone strengths [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1775-1782. |
| [5] | Chen Xi, Tang Tao, Chen Tongbing, Li Qing, Zhang Wen. Mechanical stability of intertrochanteric fracture of femur with different internal fixation systems [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1783-1788. |
| [6] | Fu Enhong, Yang Hang, Liang Cheng, Zhang Xiaogang, Zhang Yali, Jin Zhongmin. OpenSim-based prediction of lower-limb biomechanical behavior in adolescents with plantarflexor weakness [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1789-1795. |
| [7] | Ao Xiaojing, Li Kun, Liu Yuhang, Yang Xiaoxuan, Wang Xing, Li Zhijun, Ren Xiaoyan, Zhang Shaojie. Development and application of a three-dimensional digital visualization system for children’s neck acupoints [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1834-1840. |
| [8] | Zhao Jiyu, Wang Shaowei. Forkhead box transcription factor O1 signaling pathway in bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1923-1930. |
| [9] | Liang Haobo, Wang Zeyu, Ma Wenlong, Liu Hao, Liu Youwen. Hot issues in the field of joint revision: infection, rehabilitation nursing, bone defect, and prosthesis loosening [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1963-1971. |
| [10] | Lu Jieming, Li Yajing, Du Peijie, Xu Dongqing. Effects of artificial turf versus natural grass on biomechanical performance of the lower limbs in young females during jump-landing [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1101-1107. |
| [11] | He Guanghui, Yuan Jie, Ke Yanqin, Qiu Xiaoting, Zhang Xiaoling. Hemin regulates mitochondrial pathway of oxidative stress in mouse chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1183-1191. |
| [12] | He Bo, Chen Wen, Ma Suilu, He Zhijun, Song Yuan, Li Jinpeng, Liu Tao, Wei Xiaotao, Wang Weiwei, Xie Jing . Pathogenesis and treatment progress of flap ischemia-reperfusion injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1230-1238. |
| [13] | Qian Kun, Li Ziqing, Sun Shui . Endoplasmic reticulum stress in the occurrence and development of common degenerative bone diseases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1285-1295. |
| [14] | Xiang Pan, Che Yanjun, Luo Zongping. Compressive stress induces degeneration of cartilaginous endplate cells through the SOST/Wnt/beta-catenin pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 951-957. |
| [15] | Lu Ranran, Zhou Xu, Zhang Lijie, Yang Xinling. Dimethyl fumarate alleviates nerve damage in a mouse model of Parkinson’s disease [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 989-994. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||