Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (21): 4469-4476.doi: 10.12307/2025.806
Previous Articles Next Articles
Effect of foot position and chair height on lower limb kinematic and kinetic parameters during sit-to-stand tasks in children with cerebral palsy
Li Wenjing1, Gao Xiao2, Li Aihua3, Ni Yan3, Sun Wei1, Wang Jiangna1
- 1Shandong Sport University, Jinan 250102, Shandong Province, China; 2Linyi Rehabilitation Hospital, Linyi 276023, Shandong Province, China; 3Hospital of Jinan, Jinan 250013, Shandong Province, China
-
Received:2024-03-27Accepted:2024-06-17Online:2025-07-28Published:2024-12-05 -
Contact:Wang Jiangna, MS, Associate professor, Shandong Sport University, Jinan 250102, Shandong Province, China -
About author:Li Wenjing, Master candidate, Shandong Sport University, Jinan 250102, Shandong Province, China Gao Xiao, Linyi Rehabilitation Hospital, Linyi 276023, Shandong Province, China Li Wenjing and Gao Xiao contributed equally to this article. -
Supported by:Natural Science Foundation of Shandong Province, No. ZR2020QC091 (to WJN)
CLC Number:
Cite this article
Li Wenjing, Gao Xiao, Li Aihua, Ni Yan, Sun Wei, Wang Jiangna. Effect of foot position and chair height on lower limb kinematic and kinetic parameters during sit-to-stand tasks in children with cerebral palsy[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(21): 4469-4476.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

2.3 时间特征 双因素重复方差分析结果显示,座椅高度和足位两个因素在“坐-站转移”动作总时间、各阶段时间及各阶段时间百分比指标中不存在显著的交互效应(P > 0.05)和足位主效应(P > 0.05),存在显著的座椅高度主效应(P < 0.05)。 相对于高凳条件,痉挛型脑瘫儿童在低凳条件下执行“坐-站转移”任务时所花费的总时间显著更长(低凳vs.高凳,P=0.046)。相对于高凳和中凳条件,痉挛型脑瘫儿童在低凳条件下执行“坐-站转移”任务Ⅱ阶段所需时间显著更长(低凳vs.高凳,P=0.003;低凳vs.中凳,P=0.034)和其时间占比显著更高(低凳 vs.高凳,P=0.016)。见图7。"


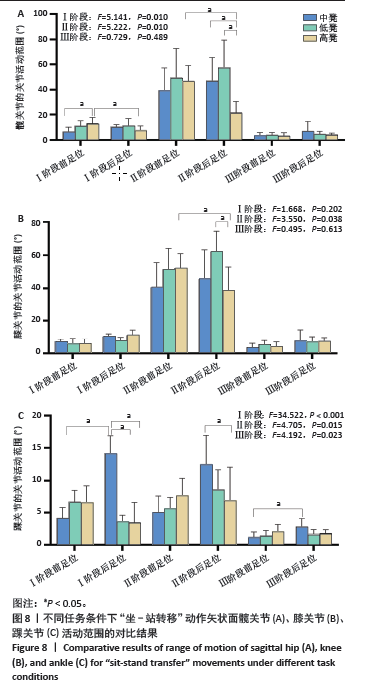
2.4 运动学指标 2.4.1 髋关节、膝关节、踝关节的活动范围 双因素重复方差分析结果显示,座椅高度和足位两个因素在不同任务条件下“坐-站转移”动作中矢状面髋关节、膝关节、踝关节的活动范围存在显著的交互效应(P < 0.05)。 事后分析结果显示,在高凳条件下,与双足前位相比,痉挛型脑瘫儿童在双足后位条件,在执行“坐-站转移”任务Ⅰ阶段过程中,髋关节的活动范围显著小一些(双足前位vs.双足后位,P=0.009);在中凳条件下,与双足前位相比,痉挛型脑瘫儿童在双足后位条件,在执行“坐-站转移”任务Ⅰ阶段过程中,踝关节的活动范围显著大一些(双足前位vs.双足后位,P < 0.001)。在双足前位条件下,与高凳条件相比,痉挛型脑瘫儿童在中凳条件,在执行“坐-站转移”任务Ⅰ阶段过程中,髋关节的活动范围显著小一些(中凳vs.高凳,P=0.008);在双足后位条件下,与低凳条件和高凳条件相比,痉挛型脑瘫儿童在中凳条件,在执行“坐-站转移”任务Ⅰ阶段过程中,踝关节的活动范围显著大一些(中凳vs.高凳,P=0.006;中凳vs.低凳, P < 0.05)。 在双足后位条件下,与中凳和低凳条件相比,痉挛型脑瘫儿童在高凳条件,在执行“坐-站转移”任务Ⅱ阶段过程中,髋关节的活动范围显著小一些(中凳vs.高凳,P=0.015;低凳vs. 高凳,P < 0.001);在双足后位条件下,与低凳条件相比,痉挛型脑瘫儿童在高凳条件,在执行“坐-站转移”任务Ⅱ阶段过程中,膝关节的活动范围显著小一些(低凳vs.高凳,P=0.004);在双足后位条件下,与中凳条件相比,痉挛型脑瘫儿童在高凳条件,在执行“坐-站转移”任务Ⅱ阶段过程中,踝关节的活动范围显著小一些(中凳vs.高凳,P=0.021)。在高凳条件下,与双足前位条件相比,痉挛型脑瘫儿童在双足后位条件,在执行“坐-站转移”任务Ⅱ阶段过程中,髋关节和膝关节的活动范围都显著小一些(髋关节:双足前位vs.双足后位,P=0.003;膝关节:双足前位vs.双足后位,P=0.04);在中凳条件下,与双足前位条件相比,痉挛型脑瘫儿童在双足后位条件,在执行“坐-站转移”任务Ⅱ阶段过程中,踝关节的活动范围显著大一些(双足前位vs.双足后位,P=0.001)。见图8。 "

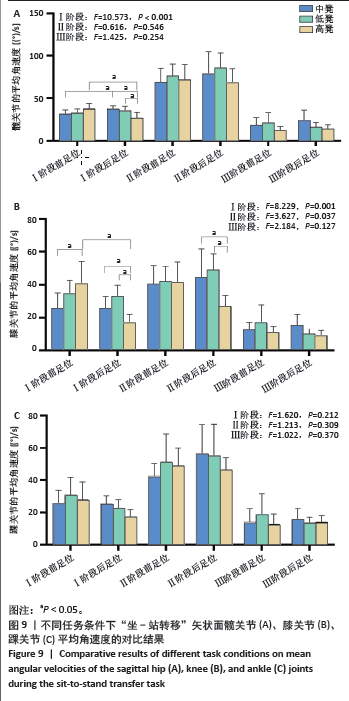
2.4.2 髋关节、膝关节、踝关节的平均角速度 双因素重复方差分析结果显示,座椅高度和足位两个因素在“坐-站转移”动作中矢状面髋关节、膝关节、踝关节的平均角速度存在显著的交互效应(P < 0.05)。 事后分析结果显示,在双足后位条件下,与中凳和低凳条件相比,痉挛型脑瘫儿童在高凳条件,在执行“坐-站转移”任务Ⅰ阶段过程中,髋关节和膝关节的平均角速度显著小一些。(髋关节:高凳 vs.中凳,P < 0.05;高凳vs.低凳,P < 0.05;膝关节:高凳vs.中凳,P=0.008,高凳vs. 低凳,P < 0.05);在高凳条件下,与双足后位相比,痉挛型脑瘫儿童在双足前位条件,在执行“坐-站转移”任务Ⅰ阶段过程中,髋关节和膝关节的平均角速度显著大一些(髋关节:双足前位vs.双足后位,P < 0.001;膝关节:双足前位vs.双足后位,P < 0.05);在中凳条件下,与双足后位相比,痉挛型脑瘫儿童在双足前位条件,在执行“坐-站转移”任务Ⅰ阶段过程中,髋关节的平均角速度显著小一些(双足前位vs.双足后位,P=0.038)。 在双足后位条件下,与中凳和低凳条件相比,痉挛型脑瘫儿童在高凳条件,在执行“坐-站转移”任务Ⅱ阶段过程中,膝关节的平均角速度显著小一些(高凳vs.中凳,P < 0.05;高凳vs.低凳,P < 0.05)。在高凳条件下,与双足后位相比,痉挛型脑瘫儿童在双足前位条件,在执行“坐-站转移”任务Ⅱ阶段过程中,膝关节的平均角速度显著大一些(双足前位vs.双足后位,P=0.022)。见图9。"

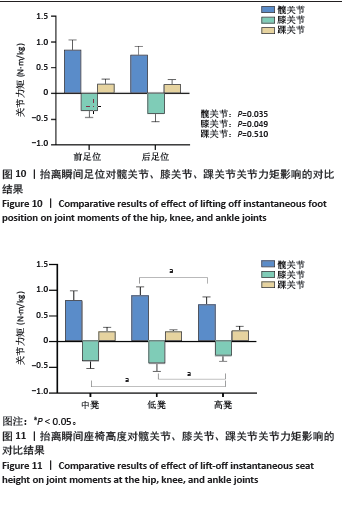
2.5 动力学指标 髋关节、膝关节、踝关节的关节力矩:双因素重复方差分析结果显示,座椅高度和足位两个因素在“坐-站转移”动作抬离瞬间髋关节力矩(P=0.923)、膝关节力矩(P=0.752)、踝关节力矩(P=0.321)不存在交互效应、分别存在足位主效应和座椅高度主效应(P < 0.05)。 与双足前位相比,痉挛型脑瘫儿童在双足后位条件下抬离瞬间髋关节的屈曲力矩显著小一些(双足前位vs.双足后位,P=0.035);与双足前位相比,痉挛型脑瘫儿童在双足后位条件下抬离瞬间膝关节的屈曲力矩显著大一些(双足前位vs.双足后位,P=0.049)。见图10。 与低凳条件相比,痉挛型脑瘫儿童在高凳条件下抬离瞬间髋关节和膝关节的屈曲力矩显著小一些(髋关节:低凳vs.高凳,P=0.008;膝关节:低凳vs.中凳,P=0.024);与中凳条件相比,痉挛型脑瘫儿童在高凳条件下抬离瞬间膝关节的屈曲力矩也显著小一些(中凳vs.高凳,P < 0.001)。见图11。 2.6 不良事件 所有参与测试的痉挛型脑瘫儿童均未发生跌倒、损伤等不良事件。 3 讨论 Discussion 3.1 足部位置及座椅高度对时间特征及运动学指标的影响 此次研究通过对脑瘫儿童在3种不同座椅高度下执行“坐-站转移”任务的时间及各阶段时间占比进行比较,结果显示在高凳条件下,脑瘫儿童完成“坐-站转移”动作所需时间更短。其原因可能是,在高凳条件下,患儿执行“坐-站转移”任务时,其身体重心位置增高[32],更加接近站立位置,身体抬高距离更短[11],完成动作所需时间缩短[33]。 此次研究的结果还表明,在低凳条件下运动总时间的增加,可能与第Ⅱ阶段的运动时间显著增加有关,第Ⅱ阶段主要进行下肢的蹬伸以及身体重心的转移,而低凳条件使得人体需要更长时间克服重力做功以及低凳条件可能会导致脑瘫儿童无法产生下肢伸展肌群的强力收缩[21,32],进而延长“坐-站转移”运动的完成时间。因此,低凳条件对脑瘫儿童下肢伸展肌群克服重力做功的能力有更高的要求,低凳座椅可能会增加其“坐-站转移”动作的完成难度,影响“坐-站转移”动作的完成质量[34]。 此次研究结果显示,足位与座椅高度对坐-站转移动作第Ⅰ、Ⅱ阶段中髋关节、膝关节、踝关节的活动范围均存在显著的交互效应。在第Ⅰ阶段,高凳条件下,与双足前位相比,双足后位条件下髋关节的活动范围显著小一些,可能与足部的放置位置改变了身体重心水平移动的距离有关。此阶段患儿完成动作需要向前移动身体重心,相较于双足前位,双足后位条件下减小了坐-站转移动作身体重心的前向水平移动距离,从而减小了髋关节的活动范围,进而降低了“坐-站转移”动作的难度。在第Ⅱ阶段,双足后位条件下,髋关节、膝关节、踝关节在高凳条件下的活动范围显著小于中凳和低凳条件。第Ⅱ阶段主要进行身体重心的垂直移动[35],而高凳条件可以直接减少“坐-站转移”动作第Ⅱ阶段的垂直位移,从而减小下肢关节的活动范围,这也与BURDETT等[16]的研究结果相一致,高凳有助于降低髋关节和膝关节活动范围,从而有利于减少髋关节和膝关节的关节压力负荷,降低“坐-站转移”动作的难度[34],更有利于脑瘫儿童“坐-站转移”动作的完成。在第Ⅱ阶段,相较于高凳和中凳,在低凳条件下,膝关节的活动范围显著大一些,可能被用来补偿脑瘫儿童“坐-站转移”运动中髋关节和膝关节伸肌无力造成的关节活动范围受限[7]。 此次研究结果显示,在第Ⅰ阶段,双足后位条件下,髋关节在高凳条件下的平均角速度显著低于中凳条件和低凳条件。从人体功效学进行分析,对于中凳和低凳来说髋关节需要更多的速度补偿以产生向前的角动量,而在高凳条件下不需要髋关节提供额外的速度补偿,因此高凳条件更有利于“坐-站转移”动作的完成[16]。已有研究表明,足部的位置越靠前,坐-站转移越困难[21],这与此次研究结果一致,与双足前位相比,脑瘫儿童在双足后位条件下执行“坐-站转移”任务时,在第Ⅰ阶段髋关节和膝关节提供较大的速度补偿,可能有助于产生向前的角动量,因此脑瘫儿童采用后足位更有助于完成“坐-站转移”动作。 3.2 足部位置及座椅高度对动力学指标的影响 关节力矩为跨过关节的所有主动肌与拮抗肌产生的净力矩,代表了中枢神经系统对肌骨系统的协同控制[36]。此次研究结果表明,相比于双足前位,脑瘫儿童在抬离瞬间采用双足后位完成“坐-站转移”动作时,髋关节的力矩显著较小,这与KAWAGOE等[33]的研究结果相一致,提示后足位条件下患儿髋关节输出较小的力矩即可完成“坐-站转移”动作,可能有利于提高神经系统对肌骨系统的控制能力,有助于动作完成。 研究结果显示,高凳条件下脑瘫儿童抬离瞬间髋关节屈曲力矩显著小于低凳条件,高凳条件下膝关节屈曲力矩显著小于中凳和低凳条件,表明抬高座椅高度可以减小髋关节和膝关节的关节力矩,降低关节受力载荷,有利于脑瘫儿童完成“坐-站转移”动作[12]。尽管如此,此次研究发现,座椅高度对脑瘫儿童抬离瞬间踝关节的力矩并没有显著性影响,其原因可能是踝关节调节策略更多的是控制身体在前后方向的运动,而髋关节和膝关节调节策略更多的是控制身体在垂直方向的运动[37]。 研究结果还发现,抬离瞬间身体重心投影在支撑面外,不充分的膝关节屈曲力矩会导致患者向后跌倒[33],与双足前位相比,双足后位条件下,脑瘫儿童抬离瞬间膝关节的屈曲力矩显著大一些,这可能是一种安全保护策略。痉挛型脑瘫儿童采取增大膝关节屈曲力矩的策略来提高抬离瞬间身体的稳定性。反之,膝关节屈曲力矩不足可能会导致脑瘫儿童跌倒风险增大以及“坐-站转移”动作的失败[38],因此,后足位有助于增大膝关节的屈曲力矩,提高身体稳定性,顺利完成“坐-站转移”动作。 3.3 应用价值及研究局限性 “坐-站转移”功能是提高脑瘫儿童移动能力的基础,脑瘫患者如果完全依赖康复师、照顾者或其他辅助人员进行“坐-站转移”,易造成肌肉萎缩,进一步造成运动功能缺失[39],因此适当的“坐-站转移”训练有利于增强肌肉力量,提高下肢运动控制和协调性,提高平衡能力,改善运动功能,提升生活质 量[40]。座椅高度及足位选择是影响患者独立、快速、稳定地完成“坐-站转移”动作的重要因素。对于脑瘫儿童的“坐-站转移”康复训练方式,可以根据患者残疾程度,通过改变患者“坐-站转移”时足位位置、座椅高度等方式进行个性化设计,有助于患者顺利完成“坐-站转移”动作。此次研究发现,高凳双足后位更有助于痉挛型脑瘫儿童完成“坐-站转移”动作,建议残疾程度严重者或在训练初期,可以建议患者采用该姿位进行康复训练。 此次研究仅纳入粗大运动功能分类系统水平为Ⅰ级的脑瘫儿童,后续研究可以纳入更多的研究对象,探讨不同障碍级别、不同障碍类型的脑瘫儿童“坐-站转移”动作特征。此外,此次研究探讨了脑瘫儿童“坐-站转移”动作的运动学、动力学特征,后续研究可以应用表面肌电测试方法,探讨该群体“坐-站转移”的神经肌肉控制特征,为精准康复提供数据支撑。 3.4 结论 此次研究发现,高凳双足后位能够减小脑瘫儿童“坐-站转移”动作中下肢活动范围及髋、膝关节运动的角速度及力矩峰值,有助于脑瘫患儿更好地完成“坐-站转移”动作。研究发现双足前位条件下执行“坐-站转移”任务,对脑瘫儿童膝关节的神经肌肉功能要求较低,对髋关节的神经肌肉功能要求较高。因此,可以根据痉挛型脑瘫儿童功能障碍重点所累及的关节不同,在执行“坐-站转移”时选择不同的足位,避免引起脑瘫儿童下肢痉挛。高座椅可作为痉挛型脑瘫儿童增强“坐-站转移”表现的辅助工具,高凳双足后位条件更有利于痉挛型脑瘫儿童“坐-站转移”的完成,建议高凳双足后位可以考虑作为脑瘫儿童“坐-站转移”训练初期的个性化姿位选择 之一。"
| [1] LIMA CRG, PAVãO SL, DA SILVA BR, et al. Cognitive-Motor Dual-Task Costs on Postural Sway During Sit-to-Stand Movement in Children With Cerebral Palsy. Phys Ther. 2023;103(4):pzad016. [2] LIM HK, KO J, LEE D, et al. Modified desk height helps children with cerebral palsy perform sit-to-stand. Disabil Rehabil Assist Technol. 2022;17(2): 221-227. [3] SOANGRA R, LOCKHART TE. A comparative study for performance evaluation of sit-to-stand task with body worn sensor and existing laboratory methods. Biomed Sci Instrum. 2012:48:407-414. [4] CHAOVALIT S, TAYLOR NF, DODD KJ. Sit-to-stand exercise programs improve sit-to-stand performance in people with physical impairments due to health conditions: a systematic review and meta-analysis. Disabil Rehabil. 2020;42(9):1202-1211. [5] LIMA CRG, PAVÃO SL, DE CAMPOS AC, et al. Impact of dual task on postural sway during sit-to-stand movement in children with unilateral cerebral palsy. Clin Biomech (Bristol, Avon). 2020;78:105072. [6] DOS SANTOS AN, PAVÃO SL, ROCHA NA. Sit-to-stand movement in children with cerebral palsy: a critical review. Res Dev Disabil. 2011;32(6):2243-2252. [7] HENNINGTON G, JOHNSON J, PENROSE J, et al. Effect of bench height on sit-to-stand in children without disabilities and children with cerebral palsy. Arch Phys Med Rehabil. 2004;85(1):70-76. [8] BEKTESHI S, MONBALIU E, MCINTYRE S, et al. Towards functional improvement of motor disorders associated with cerebral palsy. Lancet Neurol. 2023;22(3):229-243. [9] ALLEN J, ZAREEN Z, DOYLE S, et al. Multi-Organ Dysfunction in Cerebral Palsy. Front Pediatr. 2021;9:668544. [10] TEGEGNE KT. Determinants of cerebral palsy in children: systematic review. Sudan J Paediatr. 2023;23(2):126-144. [11] SURIYAAMARIT D, BOONYONG S. Comparison of the effects of chair height and anterior seat inclination on sit-to-stand ability in children with spastic diplegic cerebral palsy. J Biomech. 2020;113:110098. [12] SURIYAAMARIT D, BOONYONG S. Mechanical work, kinematics, and kinetics during sit-to-stand in children with and without spastic diplegic cerebral palsy. Gait Posture. 2019;67:85-90. [13] PAVãO SL, SILVA FP, SAVELSBERGH GJ, et al. Use of sensory information during postural control in children with cerebral palsy: systematic review. J Motor Behav. 2015;47(4):291-301. [14] PARK ES, PARK CI, LEE HJ, et al. The characteristics of sit-to-stand transfer in young children with spastic cerebral palsy based on kinematic and kinetic data. Gait Posture. 2003;17(1):43-49. [15] DOS SANTOS AN, PAVãO SL, SANTIAGO PR, et al. Sit-to-stand movement in children with hemiplegic cerebral palsy: relationship with knee extensor torque and social participation. Res Dev Disabil. 2013;34(6):2023-2032. [16] BURDETT RG, HABASEVICH R, PISCIOTTA J, et al. Biomechanical comparison of rising from two types of chairs. Phys Ther. 1985;65(8):1177-1183. [17] LEE HY, LEE IH. Comparison of center-of-pressure displacement during sit-to-stand according to chair height in children with cerebral palsy. J Phys Ther Sci. 2015;27(7):2299-2301. [18] SHEPHERD RB, KOH HP. Some biomechanical consequences of varying foot placement in sit-to-stand in young women. Scand J Rehabil Med. 1996;28(2):79-88. [19] ROCHA ADE S, KNABBEN RJ, MICHAELSEN SM. Non-paretic lower limb constraint with a step decreases the asymmetry of vertical forces during sit-to-stand at two seat heights in subjects with hemiparesis. Gait Posture. 2010;32(4):457-463. [20] KHEMLANI MM, CARR JH, CROSBIE WJ. Muscle synergies and joint linkages in sit-to-stand under two initial foot positions. Clin Biomech (Bristol, Avon). 1999;14(4):236-246. [21] MEDEIROS DL, CONCEIÇÃO JS, GRACIOSA MD, et al. The influence of seat heights and foot placement positions on postural control in children with cerebral palsy during a sit-to-stand task. Res Dev Disabil. 2015;43-44:1-10. [22] BOONYONG S, SURIYAAMARIT D. The effects of anterior seat inclination on movement time, mechanical work and kinematics during sit-to-stand in children with spastic diplegic cerebral palsy. Disabil Rehabil Assist Technol. 2021;16(5):479-482. [23] PAVÃO SL, DOS SANTOS AN, DE OLIVEIRA AB, et al. Functionality level and its relation to postural control during sitting-to-stand movement in children with cerebral palsy. Res Dev Disabil. 2014;35(2):506-511. [24] GAO B, LI L, SHEN P, et al. Effects of proprioceptive neuromuscular facilitation stretching in relieving pain and balancing knee loading during stepping over obstacles among older adults with knee osteoarthritis: A randomized controlled trial. PloS One. 2023;18(2):e0280941. [25] LI Y, YU N, ZHANG C, et al. Test-retest reliability of kinematic and kinetic parameters during dual-task stair walking in the elderly. Front Physiol. 2023;14:1177159. [26] LI Y, SONG Q, LI L, et al. Tai Chi practitioners have lower fall risks under dual-task conditions during stair descending. PloS One. 2021;16(2):e0246292. [27] WANG J, MAO M, SONG Q, et al. Effects of dual tasks on kinematic and kinetic performances during stair descent: respective effects of manual and cognitive tasks. J Sports Med Phys Fitness. 2022;62(4):492-499. [28] DOS SANTOS AN, VISICATTO LP, DE OLIVEIRA AB, et al. Effects of Kinesio taping in rectus femoris activity and sit-to-stand movement in children with unilateral cerebral palsy: placebo-controlled, repeated-measure design. Disabil Rehabil. 2019;41(17):2049-2059. [29] RODOSKY MW, ANDRIACCHI TP, ANDERSSON GB. The influence of chair height on lower limb mechanics during rising. J Orthop Res. 1989;7(2):266-271. [30] PAVãO SL, DE CAMPOS AC, ROCHA N. Age-related Changes in Postural Sway During Sit-to-stand in Typical Children and Children with Cerebral Palsy. J Mot Behav. 2019;51(2):185-192. [31] ZHENG H, SONG Q, ZHANG C, et al. The effect of text-based math task on dynamic stability control during stair descent. J Biomech. 2020;113:110088. [32] SCHENKMAN M, RILEY PO, PIEPER C. Sit to stand from progressively lower seat heights -- alterations in angular velocity. Clin Biomech (Bristol, Avon). 1996;11(3):153-158. [33] KAWAGOE S, TAJIMA N, CHOSA E. Biomechanical analysis of effects of foot placement with varying chair height on the motion of standing up. J Orthop Sci. 2000;5(2):124-133. [34] DOS SANTOS AN, PENA GM, GUILHERME EM, et al. Asymmetry in children with unilateral cerebral palsy during sit-to-stand movement: Cross-sectional, repeated-measures and comparative study. Clin Biomech (Bristol, Avon). 2020;71:152-159. [35] SCHENKMAN M, BERGER RA, RILEY PO, et al. Whole-body movements during rising to standing from sitting. Phys Ther. 1990;70(10):638-648; discussion 48-51. [36] 刘宇. 生物力学在运动控制与协调研究中的应用[J]. 体育科学,2010, 30(11):62-73. [37] YOSHIOKA S, NAGANO A, HAY DC, et al. Peak hip and knee joint moments during a sit-to-stand movement are invariant to the change of seat height within the range of low to normal seat height. Biomed Eng Online. 2014; 13(1):27. [38] RILEY PO, KREBS DE, POPAT RA. Biomechanical analysis of failed sit-to-stand. IEEE Trans Rehabil Eng. 1997;5(4):353-359. [39] 吴雪娇, 郑洁皎, 夏汶, 等. 脑卒中偏瘫患者坐-站转移生物力学分析研究进展[J]. 中国康复理论与实践,2018,24(3):290-295. [40] TUNG FL, YANG YR, LEE CC, et al. Balance outcomes after additional sit-to-stand training in subjects with stroke: a randomized controlled trial. Clin Rehabil. 2010;24(6):533-542. |
| [1] | Liu Xingzhao, Hu Tong, Ma Yan, Wang Qian, Wei Xiaohui, Chang Wanpeng, Yu Shaohong. Efficacy of rehabilitation robots on lower limb motor function in patients with cerebral palsy: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(18): 3925-3933. |
| [2] | Zuo Xinwei, Liu Gang, Bai Huizhong, Xu Lin, Zhao Yi, Ren Jingpei, Hu Chuanyu, Mu Xiaohong. Relationship between lumbar spine development and hip development in children with spastic cerebral palsy [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1247-1252. |
| [3] | Jiang Yu, Xu Lin, Zhao Yalin, Liu Gang, Zhang Yaqi, Bai Huizhong, Ren Jingpei, Zeng Jie, Mu Xiaohong. Effects of Shujin Jiannao Prescription on cell apoptosis in rats with hypoxic-ischemic brain injury [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(28): 4477-4483. |
| [4] | Liu Gang, Zeng Jie, Zhao Yalin, Deng Bowen, Jiang Shengyuan, Zhang Yaqi, Zhao Yi, Ren Jingpei, Hu Chuanyu, Xu Lin, Mu Xiaohong. Shujin Jiannao Prescription alleviates inflammation in the cerebral cortex of rats with hypoxic-ischemic cerebral palsy [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(23): 3674-3679. |
| [5] | Zhang Houjun, Deng Bowen, Jiang Shengyuan, Zhao Yi, Ren Jingpei, Xu Lin, Mu Xiaohong. Proteomic analysis of cerebrospinal fluid exosomes derived from cerebral palsy children [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(6): 903-908. |
| [6] | Liu Gang, Ma Chao, Wang Le, Zeng Jie, Jiao Yong, Zhao Yi, Ren Jingpei, Hu Chuanyu, Xu Lin, Mu Xiaohong. Ankle-foot orthoses improve motor function of children with cerebral palsy: a Meta-analysis based on 12 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1299-1304. |
| [7] | Zhong Liqing, Zhong Shanshan, Han Weichao, Hu Runkai, He Shufen, Ding Shaobo. Systematic review of the efficacy and safety of umbilical cord-derived cell transplantation for patients with cerebral palsy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 4095-4100. |
| [8] | Liu Shuai, Sun Qiangsan. ICB orthotic insole can correct balance, walking ability and biological force line of lower limbs in children with spastic diplegia [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(33): 5272-5276. |
| [9] | Xu Ping, Liang Leichao, Liang Zhenwen, Cai Ming, Chen Bo, Huang Ping, Zhang Linlin. Surface electromyogram features of the lower limb muscles in cerebral palsy children standing and walking on tiptoes [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(23): 3673-3677. |
| [10] | Dai Guang-hui, Liu Xue-bin, Zhang Zan, Cheng Hong-bin, Wang Xiao-dong, An Yi-hua. Bone marrow mesenchymal stem cells versus bone marrow mononuclear cells for treating cerebral palsy [J]. Chinese Journal of Tissue Engineering Research, 2018, 22(1): 70-76. |
| [11] | Lou Yuan-jun, Liu Yang, Shan Hai-jun, Cao Cai-hong, Jie Xiao-su. Effect of acupuncture of “Xingnao Kaiqiao” on the behavior of an immature rat model of cerebral palsy and the underlying mechanism [J]. Chinese Journal of Tissue Engineering Research, 2016, 20(49): 7314-7319. |
| [12] | Shi Hua, Zhang Pu, Guo Xin, Jie Xiao-su. Effect of acupuncture on cerebral amino acids and neurotransmitters in the immature rat model of cerebral palsy [J]. Chinese Journal of Tissue Engineering Research, 2016, 20(40): 5959-5965. |
| [13] | Jie Xiao-su, Hou Yu-jin. Effect of acupuncture on neural cell apoptosis of cerebral palsy rats [J]. Chinese Journal of Tissue Engineering Research, 2016, 20(27): 4036-4042. |
| [14] | Shi Hua, Zhang Pu, Guo Xin, Jie Xiao-su. Combination of acupuncture with placenta derived mesenchymal stem cell transplantation for cerebral palsy in a rat model [J]. Chinese Journal of Tissue Engineering Research, 2016, 20(19): 2789-2795. |
| [15] | Yang Zi-jin, Guo Jia-li, Lu Si-guang, Gao Chang-long, Li Hong-mei, Feng Yue. Human umbilical blood cord mesenchymal stem cell transplantation combined with injection of ganglioside for cerebral palsy [J]. Chinese Journal of Tissue Engineering Research, 2016, 20(19): 2803-2809. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||