Chinese Journal of Tissue Engineering Research ›› 2023, Vol. 27 ›› Issue (5): 663-668.doi: 10.12307/2023.119
Previous Articles Next Articles
Anatomic risk factors for medial meniscus posterior root tears combined with anterior cruciate ligament injuries
Liu Guangluan1, Guo Zonglei1, Ge Jin1, Huang Dong1, Wang Yehua1, 2
- 1Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China; 2Department of Orthopedics, Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China
-
Received:2022-04-03Accepted:2022-05-17Online:2023-02-18Published:2022-07-22 -
Contact:Wang Yehua, MD, Chief physician, Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China; Department of Orthopedics, Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China -
About author:Liu Guangluan, Master candidate, Physician, Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China
CLC Number:
Cite this article
Liu Guangluan, Guo Zonglei, Ge Jin, Huang Dong, Wang Yehua. Anatomic risk factors for medial meniscus posterior root tears combined with anterior cruciate ligament injuries[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(5): 663-668.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
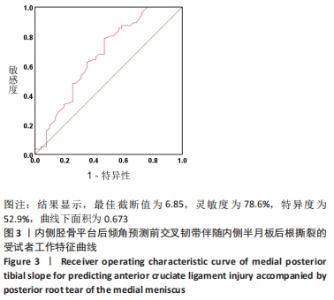
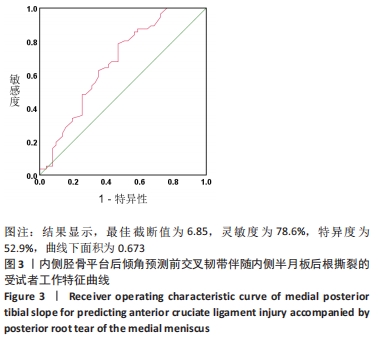
| [1] MUSAHL V, KARLSSON J. Anterior Cruciate Ligament Tear. N Engl J Med. 2019;24:2341-2348. [2] 袁浩翔,徐菁,曾锦树,等. 预防序列模型框架下前交叉韧带损伤的筛查、干预与评估[J]. 中国组织工程研究,2022,26(17):2775-2781. [3] CAIN EL JR, FLEISIG GS, PONCE BA, et al. Variables Associated with Chondral and Meniscal Injuries in Anterior Cruciate Ligament Surgery. J Knee Surg. 2017;7:659-667. [4] MANSORI AE, LORDING T, SCHNEIDER A, et al. Incidence and patterns of meniscal tears accompanying the anterior cruciate ligament injury: possible local and generalized risk factors. Int Orthop. 2018;9:2113-2121. [5] FEUCHT MJ, BIGDON S, BODE G, et al. Associated tears of the lateral meniscus in anterior cruciate ligament injuries: risk factors for different tear patterns. J Orthop Surg Res. 2015;10:34. [6] PALETTA GA JR, LEVINE DS, O’BRIEN SJ, et al. Patterns of meniscal injury associated with acute anterior cruciate ligament injury in skiers. Am J Sports Med. 1992;5:542-547. [7] LAPRADE CM, FOAD A, SMITH SD, et al. Biomechanical consequences of anonanatomic posterior medial meniscal root repair. Am J Sports Med. 2015;4:912-920. [8] MATAVA MJ. Editorial Commentary: Repair of Posterior-Medial Meniscal Root Tears: One More Potential Tool in Your Box. Arthroscopy. 2020;36(9):2498-2500. [9] CHOI YR, KIM JH, CHUNG JH, et al. The association between meniscal subluxation and cartilage degeneration. Eur J Orthop Surg Traumatol. 2014;1:79-84. [10] NAGHIBI H, JANSSEN D, VAN DEN BOOGAARD T, et al. The implications of non-anatomical positioning of a meniscus prosthesis on predicted human knee joint biomechanics. Med Biol Eng Comput. 2020;6:1341-1355. [11] MOON HS, CHOI CH, JUNG M, et al. Medial Meniscal Posterior Horn Tears Are Associated With Increased Posterior Tibial Slope: A Case-Control Study. Am J Sports Med. 2020;7:1702-1710. [12] ALAIA MICHAEL J, KAPLAN DANIEL J, MANNINO BRIAN J, et al. Tibial Sagittal Slope in Anterior Cruciate Ligament Injury and Treatment. J Am Acad Orthop Surg. 2021;29:e1045-e1056. [13] HUDEK R, FUCHS B, REGENFELDER F, et al. Is noncontact ACL injury associated with the posterior tibial and meniscal slope?. Clin Orthop Relat Res. 2011;8:2377-2384. [14] HASHEMI J, CHANDRASHEKAR N, GILL B, et al. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am. 2008;12:2724-2734. [15] HOHMANN E, TETSWORTH K, GLATT V, et al. Increased Posterior Slope of the Medial and Lateral Meniscus Posterior Horn Is Associated With Anterior Cruciate Ligament Injuries. Arthroscopy. 2022;1:109-118. [16] JIANG J, LIU Z, WANG X, et al. Increased Posterior Tibial Slope and Meniscal Slope Could Be Risk Factors for Meniscal Injuries: A Systematic Review. Arthroscopy. 2022 Jan 20:S0749-8063(22)00016-0. [17] IKAWA MH, YAMADA AF, DA ROCHA CORRÊA FERNANDES A, et al. Relationship between anterior cruciate ligament rupture and the posterior tibial and meniscal slopes in professional soccer athletes.Skeletal Radiol. 2021;10:2041-2047. [18] JENNY JY, RAPP E, KEHR P. Proximal tibial meniscal slope: a comparison with the bone slope.Rev Chir Orthop Reparatrice Appar Mot. 1997;83: 435-438. [19] OKAZAKI Y, FURUMATSU T, KODAMA Y, et al. Steep posterior slope and shallow concave shape of the medial tibial plateau are risk factors for medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. 2021;29:44-50. [20] HUDEK R, SCHMUTZ S, REGENFELDER F, et al. Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;8:2066-2072. [21] HOHMANN E, TETSWORTH K, GLATT V, et al. Increased Posterior Slope of the Medial and Lateral Meniscus Posterior Horn Is Associated With Anterior Cruciate Ligament Injuries. Arthroscopy. 2022;1:109-118. [22] GRASSI A, DI PAOLO S, LUCIDI GA, et al. The Contribution of Partial Meniscectomy to Preoperative Laxity and Laxity After Anatomic Single-Bundle Anterior Cruciate Ligament Reconstruction: In Vivo Kinematics With Navigation. Am J Sports Med. 2019;47:3203-3211. [23] POULSEN E, GONCALVES GH, BRICCA A, et al. Knee osteoarthritis risk is increased 4-6 fold after knee injury - a systematic review and meta-analysis. Br J Sports Med. 2019;53:1454-1463. [24] AGNESKIRCHNER JD, HURSCHLER C, STUKENBORG-COLSMAN C, et al. Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Winner of the AGA-DonJoy Award 2004. Arch Orthop Trauma Surg. 2004;9: 575-584. [25] MAROUANE H, SHIRAZI-ADL A, HASHEMI J. Quantification of the role of tibial posterior slope in knee joint mechanics and ACL force in simulated gait. J Biomech. 2015;10:1899-1905. [26] SHELBURNE KB, KIM HJ, STERETT WI, et al. Effect of posterior tibial slope on knee biomechanics during functional activity. J Orthop Res. 2011;29:223-231. [27] MARKL I, ZANTOP T, ZEMAN F, et al. The effect of tibial slope in acute ACL-insufficient patients on concurrent meniscal tears. Arch Orthop Trauma Surg. 2015;135:1141-1149. [28] WANG X, JING L, WANG X, et al. Effects of medial meniscal slope and medial posterior tibial slope on the locations of meniscal tears: A retrospective observational study. Medicine (Baltimore). 2020;99: e23351. [29] UNAL M, KOSE O, AKTAN C, et al. Is There a Role of Meniscal Morphology in the Risk of Noncontact Anterior Cruciate Ligament Rupture? A Case-Control Study. J Knee Surg. 2021;34:570-580. [30] BERNHOLT D, DEPHILLIPO NN, AMAN ZS, et al. Increased posterior tibial slope results in increased incidence of posterior lateral meniscal root tears in ACL reconstruction patients. Knee Surg Sports Traumatol Arthrosc. 2021;29:3883-3891. [31] KOLBE R, AYTULUN A, MÜLLER AK, et al. Steep lateral tibial slope and lateral-to-medial slope asymmetry are risk factors for concomitant posterolateral meniscus root tears in anterior cruciate ligament injuries.Knee Surg Sports Traumatol Arthrosc. 2019;27:2585-2591. [32] SLAUTERBECK JR, KOUSA P, CLIFTON BC, et al. Geographic mapping of meniscus and cartilage lesions associated with anterior cruciate ligament injuries. J Bone Joint Surg Am. 2009;9:2094-2103. [33] GRASSI A, MACCHIAROLA L, LUCIDI GA, et al. Anterior Cruciate Ligament Reconstruction and Lateral Plasty in High-Risk Young Adolescents: Revisions, Subjective Evaluation, and the Role of Surgical Timing on Meniscal Preservation. Sports Health. 2022;14:188-196. [34] PRODROMIDIS AD, DROSATOU C, THIVAIOS GC, et al. Timing of Anterior Cruciate Ligament Reconstruction and Relationship With Meniscal Tears: A Systematic Review and Meta-analysis. Am J Sports Med. 2021; 49(9):2551-2562. [35] KAWASHIMA I, TSUKAHARA T, SAKAI T, et al. Delayed anterior cruciate ligament reconstruction increases the incidence of medial meniscal bucket handle tears and medial compartment chondral injuries in patients aged 40 years and older. Arch Orthop Trauma Surg. 2021;141: 971-975. |
| [1] | Du Xueting, Zhang Xiaodong, Chen Yanjun, Wang Mei, Chen Wubiao, Huang Wenhua. Application of compressed sensing technology in two-dimensional magnetic resonance imaging of the ankle joint [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1396-1402. |
| [2] | Guo Yingqi, Gong Xianxu, Zhang Yan, Xiao Han, Wang Ye, Gu Wenguang. Meniscus extrusion and patellofemoral joint cartilage injury and bone marrow lesions: MRI semi-quantitative score [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 600-605. |
| [3] | Liu Hao, Yang Hongsheng, Zeng Zhimou, Wang Liping, Yang Kunhai, Hu Yongrong, Qu Bo. Lumbar MRI vertebral bone quality score to evaluate the severity of osteoporosis in postmenopausal women [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 606-611. |
| [4] | Li Shihao, Li Qi, Li Zhen, Zhang Yuanyuan, Liu Miaomiao, Ouyang Yi, Xu Weiguo. Plantar pressure and gait analysis in patients with anterior cruciate ligament injury and reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 626-631. |
| [5] | Wu Tong, Yin Caiyun, Zhao Mingzhe, Zhu Yishen. Application of functional peptides for biomedical diagnosis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 478-485. |
| [6] | Ma Jiang, Zhang Di, Zhao Tianyu, Liu Xiaoxiao, Wang Ju, Lu Li, Wang Ying, Jin Song. Mechanism and application prospects of motor imagery in spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(36): 5897-5904. |
| [7] | Zhang Jian, Lin Jianping, Zhou Gang, Fang Yehan, Wang Benchao, Wu Yongchang. Semi-quantitative MRI evaluation of cartilage degeneration in early knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 425-429. |
| [8] | Yuan Haoxiang, Xu Jing, Zeng Jinshu, Chen Hao, Yan Yelei, Chen Jiahao, Liu Qingshan, Xu Fei. Sequence of prevention for anterior cruciate ligament injury: screening, intervention and assessment [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(17): 2775-2781. |
| [9] | Min Youjiang, Yao Haihua, Sun Jie, Zhou Xuan, Yu Hang, Sun Qianpu, Hong Ensi. Effect of “three-tong acupuncture” on brain function of patients with spinal cord injury based on magnetic resonance technology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(在线): 1-8. |
| [10] | Min Youjiang, , Yao Haihua, Sun Jie, Zhou Xuan, Yu Hang, Sun Qianpu, Hong Ensi. Effect of “three-tong acupuncture” on brain function of patients with spinal cord injury based on magnetic resonance technology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(29): 4600-4607. |
| [11] | Yi Meizhi, Luo Guanghua, Xiao Yawen, Hu Rong, Chen Xiaolong, Zhao Heng. MRI findings of anatomical variations of the talus [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3888-3893. |
| [12] | Chen Xiaolong, Zhao Heng, Hu Rong, Luo Guanghua, Liu Jincai . Correlation of infrapatellar fat pad edema with trochlear and patellofemoral joint morphology: MRI evaluation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(15): 2410-2415. |
| [13] | Li Ying, Guan Hantian, Zhou Yu. Semantic memory impairment and neuroregulation in patients with mild cognitive impairment [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(32): 5236-5242. |
| [14] | Li Wei, Chu Zhanfei, Yu Zechen, Yu Jinghong, Jia Yanbo, Wang Zongbo. T2-mapping quantitative imaging technique based on sequence optimization in the ankle talus osteochondral injury [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(27): 4333-4337. |
| [15] | Song Yancheng, Kang Liqing, Shen Canghai, Liu Fenghai, Feng Yongjian. Application of task-state fMRI in evaluating disease severity and prognosis of cervical spondylotic myelopathy [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(21): 3341-3346. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||