Chinese Journal of Tissue Engineering Research ›› 2023, Vol. 27 ›› Issue (13): 2044-2050.doi: 10.12307/2023.292
Previous Articles Next Articles
Deep vein thrombosis distribution and risk factors after total knee arthroplasty during enhanced recovery after surgery
Wu Qian, Liu Lingfeng, Li Lisong, Lu Yingjie, Zhou Liyu, Xu Wu, Huang Lixin, Jiang Dinghua
- Department of Orthopedics, First Affiliated Hospital of Soochow University, Suzhou 215006, Jiangsu Province, China
-
Received:2022-04-12Accepted:2022-05-23Online:2023-05-08Published:2022-08-20 -
Contact:Jiang Dinghua, Master, Associate chief physician, Department of Orthopedics, First Affiliated Hospital of Soochow University, Suzhou 215006, Jiangsu Province, China Huang Lixin, Associate professor, Doctoral supervisor, Chief physician, Department of Orthopedics, First Affiliated Hospital of Soochow University, Suzhou 215006, Jiangsu Province, China -
About author:Wu Qian, Master, Physician, Department of Orthopedics, First Affiliated Hospital of Soochow University, Suzhou 215006, Jiangsu Province, China -
Supported by:the National Natural Science Foundation of China (Youth Program), No. 8160922 (to LLS); Suzhou Key Clinical Diseases Diagnosis and Treatment Fund Project, No. LCZX201901 (to HLX); the Extracurricular Academic Research Fund of Soochow University, No. KY20201019B (to WQ)
CLC Number:
Cite this article
Wu Qian, Liu Lingfeng, Li Lisong, Lu Yingjie, Zhou Liyu, Xu Wu, Huang Lixin, Jiang Dinghua. Deep vein thrombosis distribution and risk factors after total knee arthroplasty during enhanced recovery after surgery[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(13): 2044-2050.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
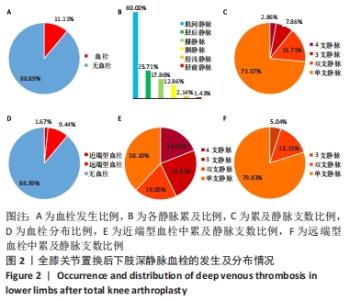
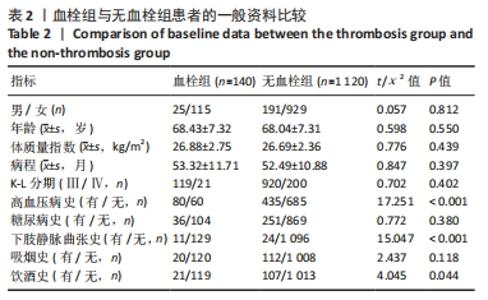
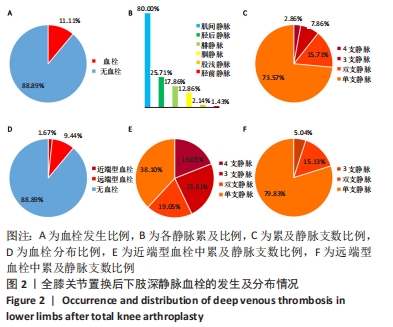
2.1 全膝关节置换后血栓发生情况 全膝关节置换后血栓发生情况,见图2A。此次研究纳入的1 260例患者中,140例患者术后经双下肢静脉彩超诊断为深静脉血栓,总体血栓发生率为11.11%(140/1 260)。 全膝关节置换后140例血栓组患者中各静脉累及情况,见图2B。各静脉累及比例从高到低依次为:肌间静脉80.00%(112/140)、胫后静脉25.71%(36/140)、腓静脉17.86%(25/140)、腘静脉12.86%(18/140)、股浅静脉2.14% (3/140)、胫前静脉1.43%(2/140)。 全膝关节置换后累及静脉支数的频率情况,见图2C。140例术后发生血栓的患者中,103例患者术后血栓单纯累及单支静脉,占比73.57%(103/140);22例患者术后血栓累及双支静脉,占比15.71%(22/140);11例患者术后血栓累及3支静脉,占比7.86%(11/140);4例患者术后血栓累及4支静脉,占比2.86%(4/140)。 根据血栓累及部位,以腘静脉平面为界,若累及腘静脉及以上静脉则分组为近端型血栓组,包括腘静脉、股浅静脉、股深静脉、股总静脉、髂外静脉。若单纯累及腘静脉以下静脉则分组为远端型血栓组,包括肌间静脉、胫前静脉、胫后静脉及腓静脉。全膝关节置换后血栓分布情况,见图2D。140例术后发生血栓的患者中,21例形成了近端型血栓,发生率为1.67%(21/1 260);119例形成了远端型血栓,发生率为9.44%(119/1 260)。 全膝关节置换后21例近端型血栓累及静脉支数频率情况,见图2E。8例单纯累及单支静脉,占比38.10%(8/21),包括腘静脉6例、股浅静脉2例。4例累及双支静脉,占比19.05%(4/21),包括腘静脉+肌间静脉1例、腘静脉+胫后静脉2例、股浅静脉+胫后静脉1例。5例累及3支静脉,占比23.81%(5/21),包括腘静脉+胫后静脉+肌间静脉1例、腘静脉+腓静脉+肌间静脉2例、腘静脉+胫后静脉+腓静脉1例、腘静脉+胫前静脉+腓静脉1例。4例累及4支静脉,占比19.05%(4/21),均为腘静脉+胫后静脉+腓静脉+肌间静脉。 全膝关节置换后119例远端型血栓中累及静脉支数频率情况,见图2F。 95例单纯累及单支静脉,占比79.83%(95/119),包括单纯累及肌间静脉84例、胫后静脉6例、腓静脉5例。18例累及双支静脉,占比15.13%(18/119),包括腓静脉+肌间静脉2例、胫前静脉+肌间静脉1例、胫后静脉+肌间静脉11例、胫后静脉+腓静脉4例。6例累及三支静脉,占比5.04%(6/119),均为胫后静脉+腓静脉+肌间静脉。 "
| [1] TALMO CT, AGHAZADEH M, BONO JV. Perioperative complications following total joint replacement. Clin Geriatr Med. 2012;28(3):471-487. [2] KURTZ S, ONG K, LAU E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780-785. [3] TANG X, WANG S, ZHAN S, et al. The Prevalence of Symptomatic Knee Osteoarthritis in China: Results From the China Health and Retirement Longitudinal Study. Arthritis Rheumatol. 2016;68(3):648-653. [4] LONGO UG, CIUFFREDA M, MANNERING N, et al. Outcomes of Posterior-Stabilized Compared with Cruciate-Retaining Total Knee Arthroplasty. J Knee Surg. 2018;31(4):321-340. [5] SALAFFI F, DI CARLO M, CAROTTI M, et al. Frailty prevalence according to the Survey of Health, Ageing and Retirement in Europe-Frailty Instrument (SHARE-FI) definition, and its variables associated, in patients with symptomatic knee osteoarthritis: findings from a cross-sectional study. Aging Clin Exp Res. 2021;33(6):1519-1527. [6] MADALENO FO, SANTOS BA, ARAÚJO VL, et al. Prevalence of knee osteoarthritis in former athletes: a systematic review with meta-analysis. Braz J Phys Ther. 2018;22(6):437-451. [7] BOURNE RB, CHESWORTH BM, DAVIS AM, et al. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57-63. [8] DAI W L, LIN ZM, SHI ZJ, et al. Venous Thromboembolic Events after Total Knee Arthroplasty: Which Patients Are at a High Risk? J Knee Surg. 2020;33(10):947-957. [9] ZHANG S, HTET KS, TAN XY, et al. Short-duration chemoprophylaxis might reduce incidence of deep vein thrombosis in Asian patients undergoing total knee arthroplasty. Knee Surg Relat Res. 2020;32(1): 58. [10] GEERTS WH, PINEO GF, HEIT JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126(3 Suppl):338-400. [11] KLATSKY AL, ARMSTRONG MA, POGGI J. Risk of pulmonary embolism and/or deep venous thrombosis in Asian-Americans. Am J Cardiol. 2000;85(11):1334-1337. [12] PIOVELLA F, WANG CJ, LU H, et al. Deep-vein thrombosis rates after major orthopedic surgery in Asia. An epidemiological study based on postoperative screening with centrally adjudicated bilateral venography. J Thromb Haemost. 2005;3(12):2664-2670. [13] WANG S, LU H, LI S. Prevention of deep venous thrombosis in patients undergoing knee arthroplasty by intermittent pneumatic compression apparatus. Am J Transl Res. 2021;13(9):10765-10770. [14] MENG B, MA J, LIU Z, et al. Efficacy and Safety of Tranexamic Acid Combined with Rivaroxaban in Primary Total Knee Arthroplasty: A Meta-Analysis of Randomized Controlled Trials. J Invest Surg. 2021; 34(7):728-737. [15] 吴乾,郝跃峰,刘毅,等.全髋关节置换术后快速康复的研究进展[J].医学综述,2018,24(15):3023-3028. [16] LIN HY, LIN CY, HUANG YC, et al. Deep vein thrombosis after major orthopedic surgery in Taiwan: A prospective cross-sectional study and literature review. J Formos Med Assoc. 2022;6646(21):594-595. [17] LEE JK, LEE KB, KIM JI, et al. Risk factors for deep vein thrombosis even using low-molecular-weight heparin after total knee arthroplasty. Knee Surg Relat Res. 2021;33(1):29. [18] DENG W, HUO L, YUAN Q, et al. Risk factors for venous thromboembolism in patients with diabetes undergoing joint arthroplasty. BMC Musculoskelet Disord. 2021;22(1):608. [19] 中华医学会骨科分会关节外科学组,吴阶平医学基金会骨科学专家委员会.膝骨关节炎阶梯治疗专家共识(2018年版)[J].中华关节外科杂志(电子版),2019,13(1):124-130. [20] OWENS WD, FELTS JA, SPITZNAGEL JR EL. ASA physical status classifications: a study of consistency of ratings. Anesthesiology. 1978; 49:239-243. [21] SHIMOYAMA Y, SAWAI T, TATSUMI S, et al. Perioperative risk factors for deep vein thrombosis after total hip arthroplasty or total knee arthroplasty. J Clin Anesth. 2012;24(7):531-536. [22] WAKABAYASHI H, HASEGAWA M, NIIMI R, et al. The risk factor of preoperative deep vein thrombosis in patients undergoing total knee arthroplasty. J Orthop Sci. 2017;22(4):698-702. [23] ZHANG H, MAO P, WANG C, et al. Incidence and risk factors of deep vein thrombosis (DVT) after total hip or knee arthroplasty: a retrospective study with routinely applied venography. Blood Coagul Fibrinolysis. 2017;28(2):126-133. [24] 姚尧,张成绩,戴小宇,等.关节置换术后下肢深静脉血栓形成的解剖分布[J].中华骨科杂志,2013,33(9):912-916. [25] 邓立庆,冯品,甘彦峰,等.藏族人群关节置换术后下肢深静脉血栓发生率及解剖分布[J].中国矫形外科杂志,2019,27(16):1446-1450. [26] CHAN WS, SPENCER FA, GINSBERG JS. Anatomic distribution of deep vein thrombosis in pregnancy. CMAJ. 2010;182(7):657-660. [27] SASAKI K, MIURA H, TAKASUGI S, et al. Venous hemodynamic alterations in lower limbs undergoing total joint arthroplasty. Am J Orthop (Belle Mead NJ). 2009;38(8):137-140. [28] FLEVAS DA, MEGALOIKONOMOS PD, DIMOPOULOS L, et al. Thromboembolism prophylaxis in orthopaedics: an update. EFORT Open Rev. 2018;3(4):136-148. [29] ZÖLLER B, JI J, SUNDQUIST J, et al. Alcohol use disorders are associated with venous thromboembolism. J Thromb Thrombolysis. 2015;40(2): 167-173. [30] FALL AO, PROULLE V, SALL A, et al. Risk factors for thrombosis in an african population. Clin Med Insights Blood Disord. 2014;7:1-6. [31] ANDERSON FA JR, SPENCER FA. Risk factors for venous thromboembolism. Circulation. 2003;107(23 Suppl 1):9-16. [32] BALA A, OLADEJI K, AMANATULLAH DF. Effect of Comorbidity Burden on the Risk of Venous Thromboembolic Events After Total Knee Arthroplasty. Geriatr Orthop Surg Rehabil. 2021;12: 21514593211043998. [33] JIANG T, YAO Y, XU X, et al. Prevalence and Risk Factors of Preoperative Deep Vein Thrombosis in Patients with End-Stage Knee Osteoarthritis. Ann Vasc Sur. 2020;64:175-180. [34] 刘其飞,钱玉英,张在清,等.全髋关节置换术后血清同型半胱氨酸、C反应蛋白、甘油三酯水平与深静脉血栓形成的相关性[J].海南医学,2020,31(12):1542-1544. [35] 刘仁德,蔡广荣,张恒,等.术前D-二聚体升高对全膝关节置换术后深静脉血栓形成的影响[J].中国矫形外科杂志,2019,27(1):22-26. [36] DAI X, DING W, LI H, et al. Associations of Serum Lipids and Deep Venous Thrombosis Risk After Total Knee Arthroplasty in Patients With Primary Knee Osteoarthritis. Int J Low Extrem Wounds. 2020;19(1):51-56. |
| [1] | Li Xiaomin, Tian Xiangdong, Tan Yetong, Zhu Guangyu, Wang Rongtian, Wang Jian, Xue Zhipeng, Ma Sheng, Hu Yuanyi, Huang Ye, Ding Tiansong. Changes of lower limb force line and knee function after high tibial osteotomy in osteoporotic medial ventricular knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1325-1329. |
| [2] | Zhang Lichuang, Gao Huali, Wang Jingchao, Lin Huijun, Wu Chonggui, Ma Yinghui, Huang Yunfei, Fang Xue, Zhai Weitao. Effect of tendon manipulation with equal emphasis on muscles and bones on accelerating the functional rehabilitation of quadriceps femoris after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1383-1389. |
| [3] | Huang Linke, Wei Linhua, Jiang Jie, Liu Qian, Chen Weiwei. Effects of estrogen combined with treadmill exercise on bone mass and articular cartilage in ovariectomized mice [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1166-1171. |
| [4] | Shen Lianwei, Zhu Hongliu, Wang Wei. Risk factor analysis of metabolic syndrome and construction of a nomogram prediction model in middle-aged and elderly people [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(5): 657-662. |
| [5] | Li Long, Li Guangdi, Shi Hao, Deng Keqi. Circular RNA as a competing endogenous RNA is involved in the regulation of osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(5): 751-757. |
| [6] | Yuan Changshen, Guan Yanbing, Li Zhe, Rong Weiming, Liao Shuning, Chen Lewei, Mei Qijie, Duan Kan. Screening and verification of key genes of necroptosis in osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(5): 695-700. |
| [7] | Liu Guangluan, Guo Zonglei, Ge Jin, Huang Dong, Wang Yehua. Anatomic risk factors for medial meniscus posterior root tears combined with anterior cruciate ligament injuries [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(5): 663-668. |
| [8] | Wei Bo, Yao Qingqiang, Tang Cheng, Li Xuxiang, Xu Yan, Wang Liming. Advantage of medial pivot prosthesis in total knee arthroplasty via medial subvastus approach [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 552-557. |
| [9] | Wan Guoli, Shi Chenhui, Wang Weishan, Li Ang, Shi Xunda, Cai Yi. Retrospective analysis of the influencing factors of chronic pain after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 558-564. |
| [10] | Gu Mingxi, Wang Bo, Tian Fengde, An Ning, Hao Ruihu, Wang Changcheng, Guo Lin. Comparison of early efficacy and safety of simultaneous and staged bilateral total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 565-571. |
| [11] | Zhang Jinbiao, Li Xiaoming, Xing Wanlin, Ma Fei, Yu Qiaoya, Dai Rongqin. Early warning efficacy of thrombus molecular markers after total knee arthroplasty in patients complicated with venous thromboembolism [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 572-577. |
| [12] | Yu He, Zheng Jiafa, Song Xiufeng, Guan Shengyi. Tibiotalocalcaneal arthrodesis with blood supplied fibular flap combined with hollow screw in the treatment of end-stage ankle osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 588-593. |
| [13] | Guo Yingqi, Gong Xianxu, Zhang Yan, Xiao Han, Wang Ye, Gu Wenguang. Meniscus extrusion and patellofemoral joint cartilage injury and bone marrow lesions: MRI semi-quantitative score [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 600-605. |
| [14] | Xu Xiangjun, Wang Chao, Song Qunshan, Li Bingyan, Zhang Jichao, Wang Guodong, Dong Yuefu. Optimal angle for prosthesis implantation in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 612-618. |
| [15] | Yu Jiaan, Liu Xinwei, Lian Hongyu, Liu Kexin, Li Zitao. Medial open-wedge tibial osteotomy versus lateral closed-wedge tibial osteotomy for unicompartmental knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 632-639. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||