Chinese Journal of Tissue Engineering Research ›› 2018, Vol. 22 ›› Issue (33): 5356-5361.doi: 10.3969/j.issn.2095-4344.0671
Previous Articles Next Articles
Three kinds of mesenchymal stem cells: differentiating into neuron-like cells
Yang Ying, Xu Qian, Wang Hui-ling, Yao Min-xiu
- Department of Endocrinology, Second Affiliated Hospital of Qingdao University Medical School, Qingdao 266042, Shandong Province, China
-
Online:2018-11-28Published:2018-11-28 -
Contact:Yao Min-xiu, Master, Chief physician, Department of Endocrinology, Second Affiliated Hospital of Qingdao University Medical School, Qingdao 266042, Shandong Province, China -
About author:Yang Ying, Department of Endocrinology, Second Affiliated Hospital of Qingdao University Medical School, Qingdao 266042, Shandong Province, China
CLC Number:
Cite this article
Yang Ying, Xu Qian, Wang Hui-ling, Yao Min-xiu. Three kinds of mesenchymal stem cells: differentiating into neuron-like cells[J]. Chinese Journal of Tissue Engineering Research, 2018, 22(33): 5356-5361.
share this article
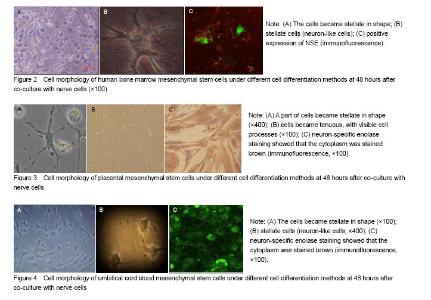
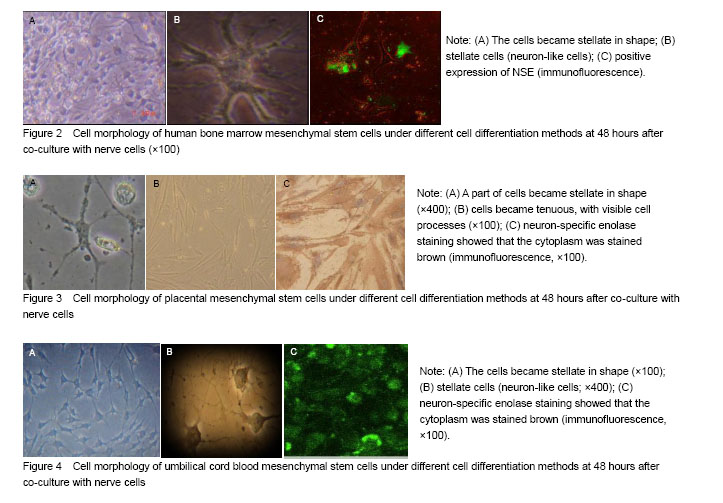
Morphological changes of hBMSCs At 48 hours of co-culture withnerve cells, hBMSCs gradually became stellate in shape (Figure 2A, B). After 4-5 days, the number of stellate cells increased gradually and the cells were interconnected with other. Immunofluorescence results showed that the cells were positive for NSE (Figure 2C), and had performance characteristics of neurons, while in the control group, BMSCs were still flat and negative for NSE, with no neuron-like morphology. Morphological changes of hPMSCs At 48 hours after co-culture with nerve cells, we observed that some hPMSCs gradually became stellate in shape (Figure 3A, B). After 4 days, the number of stellate cells increased gradually and interconnected cells were observed. Immunofluorescence results showed that the cells positively expressed NSE (Figure 3C), and had performance characteristics of neurons, while in the control group, hPMSCs were still flat in shape and negative for NSE, with no neuron-like morphology. Morphological changes of UC-MSCs At 48 hours after co-culture with nerve cells, we observed that some UC-MSCs gradually became stellate in shape (Figure 4A, B). After 4 days the number of stellate cells increased gradually and the cells were positive for NSE. Interconnected cells were observed (Figure 4C), and had performance characteristics of neurons, while in the control group, UC-MSCs were still flat in shape and negative for NSE, with no neuron-like morphology."
| [1] Otsuka T, Imura T, Nakagawa K, et al. Simulated microgravity culture enhances the neuroprotective effects of human cranial bone-derived mesenchymal stem cells in traumatic brain injury. Stem Cells Dev. 2018. doi: 10.1089/scd.2017.0299.[2] Monfrini M, Ravasi M, Maggioni D, et al. Comparing the different response of PNS and CNS injured neurons to mesenchymal stem cell treatment. Mol Cell Neurosci. 2018;86:16-24. [3] Tsui YP, Mung AK, Chan YS, et al. Hypoxic preconditioning of marrow-derived progenitor cells as a source for the generation of mature Schwann cells. J Vis Exp. 2017(124). [4] Ali EHA, Ahmed-Farid OA, Osman AAE. Bone marrow-derived mesenchymal stem cells ameliorate sodium nitrite-induced hypoxic brain injury in a rat model. Neural Regen Res. 2017;12(12):1990-1999.[5] Sakai K, Shimba K, Kotani K et al. A co-culture microtunnel technique demonstrating a significant contribution of unmyelinated Schwann cells to the acceleration of axonal conduction in Schwann cell-regulated peripheral nerve development. Integr Biol (Camb). 2017;9(8):678-686. [6] Li G, Yu F, Lei T,et al.Bone marrow mesenchymal stem cell therapy in ischemic stroke: mechanisms of action and treatment optimization strategies. Neural Regen Res. 2016;11(6):1015-1024.[7] Bonilla-Porras AR, Velez-Pardo C, Jimenez-Del-Rio M. Fast transdifferentiation of human Wharton's jelly mesenchymal stem cells into neurospheres and nerve-like cells. J Neurosci Methods. 2017;282:52-60. [8] Enomoto M.The future of bone marrow stromal cell transplantation for the treatment of spinal cord injury. Neural Regen Res. 2015;10(3):383-384.[9] Qian JY, Chopp M, Liu Z. Mesenchymal stromal cells promote axonal outgrowth alone and synergistically with astrocytes via tPA. PLoS One. 2016;11(12):e0168345.[10] Park HJ, Oh SH, Kim HN, et al. Mesenchymal stem cells enhance α-synuclein clearance via M2 microglia polarization in experimental and human parkinsonian disorder. Acta Neuropathol. 2016;132(5):685-701.[11] Kong D, Zhu J, Liu Q, et al. Mesenchymal stem cells protect neurons against hypoxic-ischemic injury via inhibiting parthanatos, necroptosis, and apoptosis, but not autophagy. Cell Mol Neurobiol. 2017;37(2):303-313.[12] Lopez-Verrilli MA, Caviedes A, Cabrera A, et al. Mesenchymal stem cell-derived exosomes from different sources selectively promote neuritic outgrowth. Neuroscience. 2016;320:129-139.[13] Gu Y, Zhang Y, Bi Y, et al. Mesenchymal stem cells suppress neuronal apoptosis and decrease IL-10 release via the TLR2/NFκB pathway in rats with hypoxic-ischemic brain damage. Mol Brain. 2015;8(1):65. [14] Okolicsanyi RK, Camilleri ET, Oikari LE, et al. Human mesenchymal stem cells retain multilineage differentiation capacity including neural marker expression after extended in vitro expansion. PLoS One. 2015;10(9):e0137255.[15] Stucky EC, Schloss RS, Yarmush ML, et al. Alginate micro-encapsulation of mesenchymal stromal cells enhances modulation of the neuro-inflammatory response. Cytotherapy. 2015;17(10):1353-1364. [16] Redondo J, Hares K, Wilkins A, et al. Reductions in kinesin expression are associated with nitric oxide-induced axonal damage. J Neurosci Res. 2015;93(6):882-892. [17] Donega V, Nijboer CH, Braccioli L, et al. Intranasal administration of human MSC for ischemic brain injury in the mouse: in vitro and in vivo neuroregenerative functions. PLoS One. 2014;9(11):e112339. [18] Donega V, Nijboer CH, van Tilborg G, et al. Intranasally administered mesenchymal stem cells promote a regenerative niche for repair of neonatal ischemic brain injury. Exp Neurol. 2014;261:53-64. [19] Cui X, Liu J, Bai L, et al. Interleukin-6 induces malignant transformation of rat mesenchymal stem cells in association with enhanced signaling of signal transducer and activator of transcription 3. Cancer Sci. 2014;105(1): 64-71.[20] Ravasi M, Scuteri A, Pasini S, et al. Undifferentiated MSCs are able to myelinate DRG neuron processes through p75. Exp Cell Res. 2013;319(19):2989-2999. [21] Xu X, Chen C, Akiyama K, et al. Gingivae contain neural-crest- and mesoderm-derived mesenchymal stem cells. J Dent Res. 2013;92(9):825-832. [22] Xin H, Chopp M, Shen LH, et al. Multipotent mesenchymal stromal cells decrease transforming growth factor β1 expression in microglia/macrophages and down-regulate plasminogen activator inhibitor 1 expression in astrocytes after stroke. Neurosci Lett. 2013;542:81-86. [23] Mukhamedshina YO, Rizvanov AA.Genetically modified human umbilical cord blood cells as a promising strategy for treatment of spinal cord injury.Neural Regen Res. 2016;11(9):1420-1421.[24] Phetfong J, Tawonsawatruk T, Seenprachawong K, et al. Re-using blood products as an alternative supplement in the optimisation of clinical-grade adipose-derived mesenchymal stem cell culture. Bone Joint Res. 2017;6(7):414-422. [25] Ordóñez-Vásquez A, Jaramillo-Gómez L, Duran-Correa C, et al. A reliable and reproducible model for assessing the effect of different concentrations of α-solanine on rat bone marrow mesenchymal stem cells. Bone Marrow Res. 2017;2017:2170306.[26] Monfrini M, Ravasi M, Maggioni D, et al. Comparing the different response of PNS and CNS injured neurons to mesenchymal stem cell treatment. Mol Cell Neurosci. 2018;86:16-24. [27] Namestnikova D, Gubskiy I, Kholodenko I, et al. Methodological aspects of MRI of transplanted superparamagnetic iron oxide-labeled mesenchymal stem cells in live rat brain. PLoS One. 2017;12(10):e0186717. [28] Namestnikova D, Gubskiy I, Kholodenko I, et al. Methodological aspects of MRI of transplanted superparamagnetic iron oxide-labeled mesenchymal stem cells in live rat brain. PLoS One. 2017;12(10):e0186717. [29] Fu Q, Liu Y, Liu X, et al. Engrafted peripheral blood-derived mesenchymal stem cells promote locomotive recovery in adult rats after spinal cord injury. Am J Transl Res. 2017; 9(9):3950-3966.[30] Dahbour S, Jamali F, Alhattab D, et al. Mesenchymal stem cells and conditioned media in the treatment of multiple sclerosis patients: Clinical, ophthalmological and radiological assessments of safety and efficacy. CNS Neurosci Ther. 2017;23(11):866-874.[31] WenBo W, Fei Z, YiHeng D, et al. Human umbilical cord mesenchymal stem cells overexpressing nerve growth factor ameliorate diabetic cystopathy in rats. Neurochem Res. 2017;42(12):3537-3547. [32] Centeno C, Markle J, Dodson E, et al. Treatment of lumbar degenerative disc disease-associated radicular pain with culture-expanded autologous mesenchymal stem cells: a pilot study on safety and efficacy. J Transl Med. 2017;15(1): 197. [33] Walsh DP, Heise A, O'Brien FJ, et al. An efficient, non-viral dendritic vector for gene delivery in tissue engineering. Gene Ther. 2017;24(11):681-691. [34] Kim HS, Lee NK, Yoo D, et al. Lowering the concentration affects the migration and viability of intracerebroventricular-delivered human mesenchymal stem cells. Biochem Biophys Res Commun. 2017;493(1): 751-757. [35] Shwartz A, Betzer O, Kronfeld N, et al. Therapeutic effect of astroglia-like mesenchymal stem cells expressing glutamate transporter in a genetic rat model of depression. Theranostics. 2017;7(10):2690-2703. [36] Ravanidis S, Bogie JFJ, Donders R, et al. Crosstalk with inflammatory macrophages shapes the regulatory properties of multipotent adult progenitor cells. Stem Cells Int. 2017;2017:2353240.[37] Chen X, Wang S, Cao W. Mesenchymal stem cell-mediated immunomodulation in cell therapy of neurodegenerative diseases. Cell Immunol. 2018;326:8-14.[38] Vanacker J, Viswanath A, De Berdt P, et al. Hypoxia modulates the differentiation potential of stem cells of the apical papilla. J Endod. 2014;40(9):1410-1418. [39] Lupatov AY, Poltavtseva RA, Bystrykh OA, et al. Neural stem/progenitor cells maintained in vitro under different culture conditions alter differentiation capacity of monocytes to generate dendritic cells. J Stem Cells Regen Med. 2017;13(2):54-61. |
| [1] | Pu Rui, Chen Ziyang, Yuan Lingyan. Characteristics and effects of exosomes from different cell sources in cardioprotection [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(在线): 1-. |
| [2] | Lin Qingfan, Xie Yixin, Chen Wanqing, Ye Zhenzhong, Chen Youfang. Human placenta-derived mesenchymal stem cell conditioned medium can upregulate BeWo cell viability and zonula occludens expression under hypoxia [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(在线): 4970-4975. |
| [3] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [4] | Hou Jingying, Yu Menglei, Guo Tianzhu, Long Huibao, Wu Hao. Hypoxia preconditioning promotes bone marrow mesenchymal stem cells survival and vascularization through the activation of HIF-1α/MALAT1/VEGFA pathway [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 985-990. |
| [5] | Shi Yangyang, Qin Yingfei, Wu Fuling, He Xiao, Zhang Xuejing. Pretreatment of placental mesenchymal stem cells to prevent bronchiolitis in mice [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 991-995. |
| [6] | Liang Xueqi, Guo Lijiao, Chen Hejie, Wu Jie, Sun Yaqi, Xing Zhikun, Zou Hailiang, Chen Xueling, Wu Xiangwei. Alveolar echinococcosis protoscolices inhibits the differentiation of bone marrow mesenchymal stem cells into fibroblasts [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 996-1001. |
| [7] | Fan Quanbao, Luo Huina, Wang Bingyun, Chen Shengfeng, Cui Lianxu, Jiang Wenkang, Zhao Mingming, Wang Jingjing, Luo Dongzhang, Chen Zhisheng, Bai Yinshan, Liu Canying, Zhang Hui. Biological characteristics of canine adipose-derived mesenchymal stem cells cultured in hypoxia [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1002-1007. |
| [8] | Geng Yao, Yin Zhiliang, Li Xingping, Xiao Dongqin, Hou Weiguang. Role of hsa-miRNA-223-3p in regulating osteogenic differentiation of human bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1008-1013. |
| [9] | Lun Zhigang, Jin Jing, Wang Tianyan, Li Aimin. Effect of peroxiredoxin 6 on proliferation and differentiation of bone marrow mesenchymal stem cells into neural lineage in vitro [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1014-1018. |
| [10] | Zhu Xuefen, Huang Cheng, Ding Jian, Dai Yongping, Liu Yuanbing, Le Lixiang, Wang Liangliang, Yang Jiandong. Mechanism of bone marrow mesenchymal stem cells differentiation into functional neurons induced by glial cell line derived neurotrophic factor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1019-1025. |
| [11] | Duan Liyun, Cao Xiaocang. Human placenta mesenchymal stem cells-derived extracellular vesicles regulate collagen deposition in intestinal mucosa of mice with colitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1026-1031. |
| [12] | Pei Lili, Sun Guicai, Wang Di. Salvianolic acid B inhibits oxidative damage of bone marrow mesenchymal stem cells and promotes differentiation into cardiomyocytes [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1032-1036. |
| [13] | Wang Xianyao, Guan Yalin, Liu Zhongshan. Strategies for improving the therapeutic efficacy of mesenchymal stem cells in the treatment of nonhealing wounds [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1081-1087. |
| [14] | Wang Shiqi, Zhang Jinsheng. Effects of Chinese medicine on proliferation, differentiation and aging of bone marrow mesenchymal stem cells regulating ischemia-hypoxia microenvironment [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1129-1134. |
| [15] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||