Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (24): 3858-3863.doi: 10.3969/j.issn.2095-4344.2017.24.015
Previous Articles Next Articles
Establishment of a rat osteoporotic model by ovariectomy combined with glucocorticoid exposure
Zhang Yu-zhuo1, Shen Geng-yang1, Zhang Zhi-da1, Zhao Wen-hua1, Huang Jin-jing1, Yu Xiang1, Qiu Ting1, Lu Yong-qiang1, Zhan Mei-qi1, Yang Zhi-dong2, Yao Zhen-song2, Liang De2
- 1Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China; 2the First Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China
-
Revised:2017-07-26Online:2017-08-28Published:2017-08-30 -
Contact:Liang De, Master, Professor, the First Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China -
About author:Zhang Yu-zhuo, Studying for master’s degree, Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China -
Supported by:the National Natural Science Foundation of China, No. 81503591 and 81674000; the Natural Science Foundation of Guangdong Province, No. 2014A030310082; the Research Project of Guangdong Provincial Department of Science and Technology-Guangdong Academy of Chinese Medicine, No. 2016A030313645 and 2014A020221021; the Excellent Doctoral Dissertation Training Project of the First Clinical Medical School of Guangzhou University of Chinese Medicine, No. YB201501 and YB201602; the Innovation and Hospital Improvement Project of the First Affiliated Hospital of Guangzhou University of Chinese Medicine, No. 2015QN03
CLC Number:
Cite this article
Zhang Yu-zhuo, Shen Geng-yang, Zhang Zhi-da, Zhao Wen-hua, Huang Jin-jing, Yu Xiang, Qiu Ting, Lu Yong-qiang, Zhan Mei-qi, Yang Zhi-dong, Yao Zhen-song, Liang De. Establishment of a rat osteoporotic model by ovariectomy combined with glucocorticoid exposure[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(24): 3858-3863.
share this article

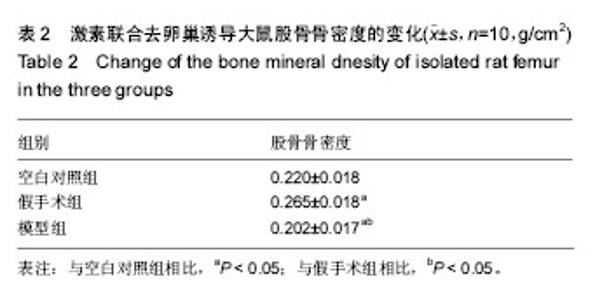
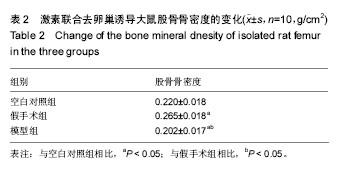
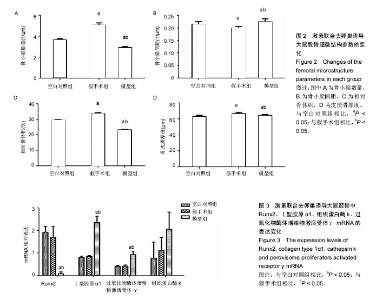
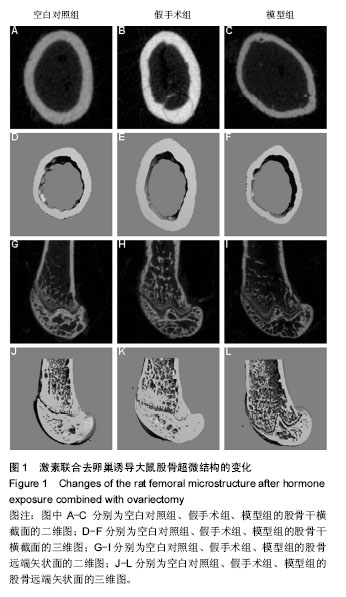
2.3 骨微细结构 Micro-CT扫描显示,与空白对照组相比,假手术组造模后4周股骨骨小梁排列更致密,骨皮质更厚,但骨小梁结构略有受损,骨小梁数量、相对骨体积、骨皮质厚度显著增加,骨小梁间距下降(P < 0.05);与空白对照组及假手术组相比,模型组大鼠骨小梁间距增宽,且结构受损,骨皮质变薄,骨小梁数量、相对骨体积降低,骨小梁间距提高(P < 0.01),且模型组骨皮质厚度较假手术组降低(P < 0.05;图1,2)。 2.4 Runx2、Ⅰ型胶原α1、组织蛋白酶k、过氧化物酶体增殖物激活受体γ的mRNA表达水平 造模后4周,模型组大鼠骨组织Runx2 mRNA表达较空白对照组及假手术组显著下调,Ⅰ型胶原α1、过氧化物酶体增殖物激活受体γ mRNA表达均较空白对照组及假手术组明显升高(P < 0.05),但组织蛋白酶kmRNA表达水平与空白对照组及假手术组接近(P > 0.05;图3)。"
| [1] Wang J, Wang Y, Liu WD, et al. Hip fractures in Hefei, China: the Hefei osteoporosis project. J Bone Miner Metab. 2014; 32(2):206-214. [2] 黄燕兴,朱弼堃,张红.髋部骨折住院治疗费用统计和分析(1998-2003年)[J].中国骨质疏松杂志,2005,11(2):195-198.[3] 刘媛,王永福,刘忠厚.糖皮质激素和骨质疏松关系的研究进展[J].中国骨质疏松杂志,2010,16(9):713-718.[4] Baccaro LF, Conde DM, Costa-Paiva L, et al. The epidemiology and management of postmenopausal osteoporosis: a viewpoint from Brazil. Clin Interv Aging. 2015;10:583-591.[5] Whittier X, Saag KG. Glucocorticoid-induced Osteoporosis. Rheum Dis Clin North Am. 2016;42(1):177-189, x. [6] Grossman JM, Gordon R, Ranganath VK, et al. American College of Rheumatology 2010 recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res (Hoboken). 2010;62(11): 1515-1526. [7] Overman RA, Toliver JC, Yeh JY, et al. United States adults meeting 2010 American College of Rheumatology criteria for treatment and prevention of glucocorticoid-induced osteoporosis. Arthritis Care Res (Hoboken). 2014;66(11): 1644-1652. [8] 张智海,刘忠厚,李娜,等.中国人骨质疏松症诊断标准专家共识(第三稿•2014版)[J].中国骨质疏松杂志,2014,20(9):1007-1010.[9] 郭鱼波,马如风,王丽丽,等.骨质疏松动物模型及其评价方法的研究进展[J].中国骨质疏松杂志,2015,21(9):1149-1154.[10] 张春丽,李忠海,周颖,等.构建骨质疏松动物模型建模方法的改进及评价[J].中国组织工程研究,2016,20(5):754-759.[11] Kalpakcioglu BB, Engelke K, Genant HK. Advanced imaging assessment of bone fragility in glucocorticoid-induced osteoporosis. Bone. 2011;48(6):1221-1231.[12] Wu WJ, Lee HY, Lee GH, et al. The antiosteoporotic effects of Cheonggukjang containing vitamin k2 (menaquinone-7) in ovariectomized rats. J Med Food. 2014;17(12):1298-1305. [13] Govindarajan P, Khassawna T, Kampschulte M, et al. Implications of combined ovariectomy and glucocorticoid (dexamethasone) treatment on mineral, microarchitectural, biomechanical and matrix properties of rat bone. Int J Exp Pathol. 2013;94(6):387-398. [14] Böcker W, El Khassawna T, Bauer N, et al. Short-term glucocorticoid treatment causes spinal osteoporosis in ovariectomized rats. Eur Spine J. 2014;23(11):2437-2448. [15] Baofeng L, Zhi Y, Bei C, et al. Characterization of a rabbit osteoporosis model induced by ovariectomy and glucocorticoid. Acta Orthop. 2010;81(3):396-401. [16] Jackson RD, Mysiw WJ. Insights into the epidemiology of postmenopausal osteoporosis: the Women's Health Initiative. Semin Reprod Med. 2014;32(6):454-462. [17] Liu X, Lei W, Wu Z, et al. Effects of glucocorticoid on BMD, micro-architecture and biomechanics of cancellous and cortical bone mass in OVX rabbits. Med Eng Phys. 2012; 34(1):2-8. [18] 段瑞平,吴凌,林云锋,等.不同成骨诱导作用下骨髓间充质干细胞的基因表达模式[J].四川大学学报(医学版),2006,37(6): 856-859.[19] 代志鹏,许伟华,杨述华,等.人骨髓间充质干细胞的生物学特性及成骨诱导分化的研究[J].中国矫形外科杂志,2014,22(15): 1402-1407.[20] 余炜,朱超,茅伟伟,等.神经肽P物质通过诱导RUNX2表达对小鼠成骨细胞增殖能力的影响[J].上海交通大学学报(医学版),2017, 37(1):15-20.[21] 唐欢,许海甲,侯煜东,等.Runx2基因对骨代谢调控的研究进展[J].中国骨质疏松杂志,2014,20(12):1501-1505.[22] Martin A, Xiong J, Koromila T, et al. Estrogens antagonize RUNX2-mediated osteoblast-driven osteoclastogenesis through regulating RANKL membrane association. Bone. 2015;75:96-104. [23] 宋纯理,党耕町.髓腔内脂肪细胞与骨质疏松[J].中国骨质疏松杂志,2002,8(3):266-269.[24] Ding ST, Schinckel AP, Weber TE, et al. Expression of porcine transcription factors and genes related to fatty acid metabolism in different tissues and genetic populations. J Anim Sci. 2000;78(8):2127-2134.[25] 黄成校,余化龙,高超,等.骨髓间充质干细胞复合Ⅰ型胶原修饰的聚乳酸聚乙醇酸对骨质疏松大鼠骨缺损的影响[J].安徽医药, 2017,21(4):618-622.[26] Kurt-Sirin O, Yilmaz-Aydogan H, Uyar M, et al. Combined effects of collagen type I alpha1 (COL1A1) Sp1 polymorphism and osteoporosis risk factors on bone mineral density in Turkish postmenopausal women. Gene. 2014;540(2): 226-231. [27] 宗强,李立军,姜竹岩, 等.Ⅰ型胶原α1 Sp1多态性与骨密度和骨折关联性的Meta分析[J].中国组织工程研究,2015,19(33): 5395-5401.[28] 何进卫,章振林.上海绝经后妇女Ⅰ型胶原α1基因多态性与骨密度关系的研究[J].中国全科医学,2007,10(7):531-532,535.[29] Hu M, Ou-Yang HF, Wu CG, et al. Notch signaling regulates col1α1 and col1α2 expression in airway fibroblasts. Exp Biol Med (Maywood). 2014;239(12):1589-1596. [30] Wang ZF, Guo X, Bai GL, et al. Detection of serum PICP and PINP and COL1alpha1 DNA sequence analysis in patients with arsenic poisoning in Dazhuyuan Town, Ankang area in southern Shaanxi Province. Nan Fang Yi Ke Da Xue Xue Bao. 2008;28(7):1141-1144. [31] Liu S, Liao G, Li G. Regulatory effects of COL1A1 on apoptosis induced by radiation in cervical cancer cells. Cancer Cell Int. 2017;17:73. [32] Seto T, Yamamoto T, Shimojima K, et al. A novel COL1A1 mutation in a family with osteogenesis imperfecta associated with phenotypic variabilities. Hum Genome Var. 2017;4: 17007.[33] Ackermann AM, Levine MA. Compound heterozygous mutations in COL1A1 associated with an atypical form of type I osteogenesis imperfecta. Am J Med Genet A. 2017. in press.[34] Andersson K, Dahllöf G, Lindahl K, et al. Mutations in COL1A1 and COL1A2 and dental aberrations in children and adolescents with osteogenesis imperfecta - A retrospective cohort study. PLoS One. 2017;12(5):e0176466.[35] Legendre F, Ollitrault D, Gomez-Leduc T, et al. Enhanced chondrogenesis of bone marrow-derived stem cells by using a combinatory cell therapy strategy with BMP-2/TGF-β1, hypoxia, and COL1A1/HtrA1 siRNAs. Sci Rep. 2017;7(1): 3406.[36] Lee JS, Seo J, Cho A, et al. Severe hypotonia and postnatal growth impairment in a girl with a missense mutation in COL1A1: Implication of expanded phenotypic spectrum of type I collagenopathy. Brain Dev. 2017. in press.[37] Bai GP, Yan GH, Wang GJ, et al. Effects of lentiviral vector?mediated shRNA silencing of TGFβ1 on the expression of Col1a1 in rat hepatic stellate cells. Mol Med Rep. 2017;16(3): 2785-2790.[38] Selinger CI, Day CJ, Morrison NA. Optimized transfection of diced siRNA into mature primary human osteoclasts: inhibition of cathepsin K mediated bone resorption by siRNA. J Cell Biochem. 2005;96(5):996-1002.[39] Wilson SR, Peters C, Saftig P, et al. Cathepsin K activity-dependent regulation of osteoclast actin ring formation and bone resorption. J Biol Chem. 2009;284(4): 2584-2592. [40] Kozloff KM, Quinti L, Tung C, et al. Non-invasive imaging of osteoclast activity via near-infrared cathepsin-K activatable optical probe. J Musculoskelet Neuronal Interact. 2006; 6(4):353.[41] Chen W, Yang S, Abe Y, et al. Novel pycnodysostosis mouse model uncovers cathepsin K function as a potential regulator of osteoclast apoptosis and senescence. Hum Mol Genet. 2007;16(4):410-423.[42] Kozloff KM, Quinti L, Patntirapong S, et al. Non-invasive optical detection of cathepsin K-mediated fluorescence reveals osteoclast activity in vitro and in vivo. Bone. 2009; 44(2):190-198. [43] Motyckova G, Fisher DE. Pycnodysostosis: role and regulation of cathepsin K in osteoclast function and human disease. Curr Mol Med. 2002;2(5):407-421.[44] Kim MK, Kim HD, Park JH, et al. An orally active cathepsin K inhibitor, furan-2-carboxylic acid, 1-{1-[4-fluoro-2-(2-oxo-pyrrolidin-1-yl)-phenyl]-3-oxo-piperidin-4-ylcarbamoyl}-cyclohexyl)-amide (OST-4077), inhibits osteoclast activity in vitro and bone loss in ovariectomized rats. J Pharmacol Exp Ther. 2006;318(2):555-562.[45] 王东,顾建红,刘宗平.组织蛋白酶K在骨吸收中的作用研究进展[J].动物医学进展,2014,35(6):114-116.[46] Zhou J, Li X, Liao Y, et al. Effects of electroacupuncture on bone mass and cathepsin K expression in ovariectomised rats. Acupunct Med. 2014;32(6):478-485. [47] Jacome-Galarza C, Soung do Y, Adapala NS, et al. Altered hematopoietic stem cell and osteoclast precursor frequency in cathepsin K null mice. J Cell Biochem. 2014;115(8): 1449-1457.[48] Siddiqi MH, Siddiqi MZ, Kang S, et al. Inhibition of Osteoclast Differentiation by Ginsenoside Rg3 in RAW264.7 Cells via RANKL, JNK and p38 MAPK Pathways Through a Modulation of Cathepsin K: An In Silico and In Vitro Study. Phytother Res. 2015. in press. [49] Ren ZY, Machuca-Gayet I, Domenget C, et al. Azanitrile Cathepsin K Inhibitors: Effects on Cell Toxicity, Osteoblast-Induced Mineralization and Osteoclast-Mediated Bone Resorption. PLoS One. 2015;10(7):e0132513. [50] Wilson S, Hashamiyan S, Clarke L, et al. Glycosaminoglycan-mediated loss of cathepsin K collagenolytic activity in MPS I contributes to osteoclast and growth plate abnormalities. Am J Pathol. 2009;175(5): 2053-2062.[51] Lotinun S, Kiviranta R, Matsubara T, et al. Osteoclast-specific cathepsin K deletion stimulates S1P-dependent bone formation. J Clin Invest. 2013;123(2):666-681. [52] Aumiller J. Cathepsin K inhibitor: new therapy approach against osteoporosis. Pharmacological target in the osteoclast. MMW Fortschr Med. 2011;153(19):16. |
| [1] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [2] | Jiang Huanchang, Zhang Zhaofei, Liang De, Jiang Xiaobing, Yang Xiaodong, Liu Zhixiang. Comparison of advantages between unilateral multidirectional curved and straight vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1407-1411. |
| [3] | Zhu Chan, Han Xuke, Yao Chengjiao, Zhou Qian, Zhang Qiang, Chen Qiu. Human salivary components and osteoporosis/osteopenia [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1439-1444. |
| [4] | Li Wei, Zhu Hanmin, Wang Xin, Gao Xue, Cui Jing, Liu Yuxin, Huang Shuming. Effect of Zuogui Wan on bone morphogenetic protein 2 signaling pathway in ovariectomized osteoporosis mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1173-1179. |
| [5] | Xiao Hao, Liu Jing, Zhou Jun. Research progress of pulsed electromagnetic field in the treatment of postmenopausal osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1266-1271. |
| [6] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [7] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [8] | Gao Yujin, Peng Shuanglin, Ma Zhichao, Lu Shi, Cao Huayue, Wang Lang, Xiao Jingang. Osteogenic ability of adipose stem cells in diabetic osteoporosis mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 999-1004. |
| [9] | Peng Kun. Improvement of the treatment effect of osteoporotic fractures: research status and strategy analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 980-984. |
| [10] | Shen Song, Xu Bin. Diffuse distribution of bone cement in percutaneous vertebroplasty reduces the incidence of refracture of adjacent vertebral bodies [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 499-503. |
| [11] | He Yunying, Li Lingjie, Zhang Shuqi, Li Yuzhou, Yang Sheng, Ji Ping. Method of constructing cell spheroids based on agarose and polyacrylic molds [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 553-559. |
| [12] | He Guanyu, Xu Baoshan, Du Lilong, Zhang Tongxing, Huo Zhenxin, Shen Li. Biomimetic orientated microchannel annulus fibrosus scaffold constructed by silk fibroin [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 560-566. |
| [13] | Chen Xiaoxu, Luo Yaxin, Bi Haoran, Yang Kun. Preparation and application of acellular scaffold in tissue engineering and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 591-596. |
| [14] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [15] | Shen Jiahua, Fu Yong. Application of graphene-based nanomaterials in stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 604-609. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||