Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (10): 1611-1616.doi: 10.3969/j.issn.2095-4344.2017.10.022
Previous Articles Next Articles
Tissue-engineered scaffold preparation using three-dimensional printing technology: a retrospective study on bone repair
Jin Can, Chen Zhen-qi
- Department of Orthodontics, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong
University School of Medicine, Shanghai Key Laboratory of Stomatology, Shanghai 200011, China
-
Received:2016-12-13Online:2017-04-08Published:2017-05-08 -
Contact:Chen Zhen-qi, Professor, Department of Orthodontics, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai Key Laboratory of Stomatology, Shanghai 200011, China -
About author:Jin Can, Studying for master’s degree, Department of Orthodontics, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai Key Laboratory of Stomatology, Shanghai 200011, China -
Supported by:the Scientific Research Program of the Shanghai Science and Technology Committee, No. 124119b0103
CLC Number:
Cite this article
Jin Can, Chen Zhen-qi. Tissue-engineered scaffold preparation using three-dimensional printing technology: a retrospective study on bone repair[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(10): 1611-1616.
share this article
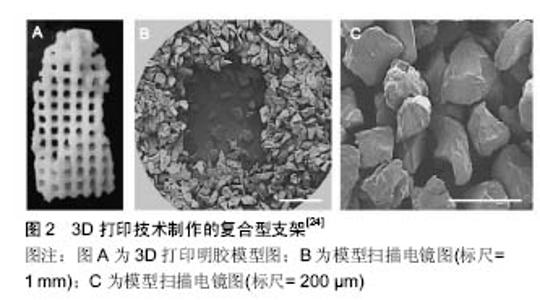
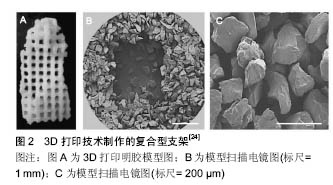
将种子细胞从组织中分离出来,体外扩增后与支架混合形成细胞-材料复合物,将复合物植入机体,随着材料逐渐被降解吸收,细胞体内增殖,最终形成相应的组织或者器官,这样的技术被称为组织工程技术。在整个技术中,支架形成了三维结构用以支持细胞的生长,也通过孔隙为细胞提供营养以及排泄代谢废物,最终植入体内也需要适宜的支架形态处理,以利于植入物更好地发挥各项性能,故支架的材质、制作工艺以及形态的设计是组织工程研究的重点所在。文章将从孔隙的设计、制作工艺的不同、材料的复合方式以及表面促生长因子涂层的应用4个方面来阐述近几年来对于支架的研究进展以及未来的展望。 2.1 孔隙设计 支架中必要的孔隙给种子细胞的沉积提供了更大的表面积,并且可以为新生组织的长入提供引导,相互连通的通道还可以促进营养物质的传递和代谢物的排泄。早在2004年,Seitz等[16]便利用改良的羟基磷灰石粉末材料,通过3D打印技术制作出了多孔生物陶瓷支架,该支架可以具备直径45 μm的通道且通道间壁厚仅为330 μm,机械强度可达到22 MPa。然而单一的孔隙并不能发挥出最大的作用,通道直径大小和通道排列方式的不同对于成骨的影响尚无定论。 Simon等[17]为了研究这方面,在2008年用同样的材料通过3D打印制作陶瓷多孔支架。实验设计分为2组:组一:直径500 μm的通道与支架长轴平行,以及组二:直径800 μm的通道且每层通道互相垂直,MicroCT分析长入孔隙的新骨生成量,结果表明组一在初期(8周)新骨长入孔隙的容积百分比显著大于组二,但是在16周时,组二新骨长入孔隙的容积百分比有所提升,相反的组一则减少了28%-45%,故最终结果表明组二的孔隙设计在16周的时候表现出较好的成骨特性。 2011年Khoda等[18]利用3D打印可控性强的特点,制作出了孔隙大小和孔隙率根据组织需求呈现不同梯度的支架,来满足同一组织中可能需要不同机械性能和生物性能的要求,这种支架具有更优秀的结构完整性,提高了氧扩散的能力,可以顺利引导组织再生,最重要的是形成了一个恒定的孔隙规格、相互联系的复合孔隙通道系统,从而更准确地规划了细胞沉积和生长路径。 同年 Fedorovich等[19]运用水凝胶材料,研究得出3D打印的多孔水凝胶支架对干细胞的成血管和成骨有促进作用,以及干细胞在低氧环境下新陈代谢和成骨分化的作用增强,说明孔隙的引进也显著提高了水凝胶支架的传导性能和成骨祖细胞的功能发挥。 2.2 制作工艺 经过多年的实践探索,组织工程支架,包括3D打印技术制作的支架与传统制作手法和工艺比较有了一定的发展。传统的制作流程为:粉末在高分子粘结剂的作用下分层沉积,制作出生胚后清除多余的粉末,在1 250 ℃的高温下烧结,高分子粘接剂被分解,从而支架成形。 胶原-羟磷灰石复合支架是一种常见的复合支架,这种复合支架的常规制作方法是通过冷冻组分中的水分散体,而后冷冻干燥法干燥形成泡沫状基质,然而因其不良好的营养和氧流通以及代谢物的排出不便,不适合细胞群落的生长。 2008年Sachlos等[20]利用液态二氧化碳,通过3D打印技术和临界点干燥法,在无细胞毒性和不改变羟磷灰石以及胶原成分基本结构基础的前提下,制造出了更适宜细胞附着及生长的支架形态。而传统工艺中,基于粉末材料的3D打印技术作为常规技术被广泛应用,但随后因不易清除成型的支架结构上面所有的松散粉末,而游离粉末对支架的性能有一定影响,因而无粉技术应运而生。 2013年Butscher[21]设计出可以俘获松散粉末的带窗笼状结构,研究包括2种形态的装置:沙漏状和柱状,实验按照装置与支架主体的关系不同分为可移动组和与支架主体结合组,结果表明可移动组能够更好的实现无粉操作,显著提高了支架的各种性能。 除了对制作工艺宏观的调控,微观上对支架材料内部性状的改变也可以促进支架作用的发挥。软骨损伤会导致关节退行性变,2012年Fedorovich等[22]应用3D纤维沉积技术制作负载细胞的多相带孔水凝胶支架,通过改变纤维的位置和角度来做出不同孔隙率和弹性模量的支架,从而更有利于修复软骨损伤。通常,营养流体动力学是决定了体内和体外细胞环境的重要因素。针对细胞外环境,同年Rath等[23]为了获得可比较的体外结果,应用生物反应器给3D打印支架提供了一个可控的流体环境,提高了细胞的存活率。实验表明,无生物反应器的静态培养环境下细胞数量明显减少。有趣的是,生物反应器制造的动态培养环境不仅可以减缓细胞数量的减少,还可以显著提高细胞分化能力。 2.3 复合材料 单一材料制作的支架已经无法满足组织工程结构的各种性能要求,复合材料必定是今后研究的重点。在2013年Korpela等[24]意识到3D打印熔融沉积成型法可以使用热塑性高分子聚合物来制作支架,但是其材料的应用范围还没有完全被明确,于是针对两种复合支架进行了实验:聚已内酯/生物玻璃(PCL/BAG)和丙交酯/己内酯(PLC)共聚物,结果表明细胞在2种支架上均有显著生存和发育能力,但是成纤维细胞在后者的沉积能力显著高于前者。而由于直接3D打印技术对于材料的选择有限制,Lee等[25]利用间接3D打印技术,在通过明胶制作所需形状的模型,利用聚乙酸内酯和壳聚糖的复合材料,最终形成复合型支架(图2)。结果表明该类支架性能较单一材料支架有显著提升,且生物活性磷灰石因其具有骨诱导特性而作为涂层材料,加速了细胞的增殖和转移。 除了主要组分材料的复合以外,在辅料的配比上的研究也可以优化支架的各项性能。在2014年,Inzana[26]通过低温3D打印技术制作磷酸三钙支架,在磷酸粘结剂溶液为8.75%的配比且加入吐温80的条件下3D打印,使细胞相容性和机械强度最大化。实验为了获得更好的性能,胶原被融入粘结剂中来形成胶原-磷酸钙成分,并分别通过生理温度和吐温80处理,减少粘度和表面张力。结果表明补充1.0%-2.0%的胶原可以最大化地提高弹性形能和细胞存活率。 复合材料不仅指两种材料的复合,3种或者更多的材料的复合也可以使材料性能更加多元化。2015年Goncalves[27]研究出一种三相支架,成分包括:纳米晶体羟磷灰石、碳纳米管和高分子聚乙酸内酯。碳纳米管含量从0到10%,混于50%的聚己内酯基质中,羟基磷灰石作为平衡成分,结果表明含有2%的碳纳米管的实验组拥有最好的综合性能包括机械性能和导电性,且具有良好的细胞附着和传播性能,预示这种新的合成材料良好的应用前景。 2.4 表面涂层处理 复合材料的应用很大程度上提高了支架的各项性能,而随着研究的深入,支架表面涂层也逐渐成了研究的重点。 人骨中常见的微量元素有硅、锌、锶、镁等,这些微量元素具有促进成骨和成血管的功能。比如硅元素参与骨的钙化作用,在钙化初始阶段起作用,食物中的硅能增加钙化的速度,尤其当钙摄入量低时效果更为明显;锶可调节MSCs(骨髓间充质干细胞)向成骨细胞分化,并促进骨基质蛋白的合成和沉淀;锌和镁均为人体维持正常生理功能所必需的微量元素。 早在2013年Fielding等[28]就研究得出,在β-磷酸三钙表面涂层氧化硅和氧化锌,结果表明涂层促进了成骨和成血管的作用,而且新血管形成量是单纯磷酸三钙支架组的3倍。Tarafder等[29]一直致力于3D打印磷酸三钙支架的性能研究,在2013年的前期研究中表明微波烧结技术可以有效增强磷酸三钙多孔支架的机械性能,又因为磷酸三钙支架中阿仑膦酸钠的释放代表了磷酸三钙的降解,他们于2014年研究得出在磷酸三钙支架表面加上聚乙酸内酯涂层[30],对控制和维持阿仑膦酸钠释放有作用。研究表明磷酸三钙+阿仑膦酸钠+聚己内酯支架组最大化地促进新骨生成,跟单纯磷酸三钙组和聚己内酯涂层的磷酸三钙组相比,所有包含阿仑膦酸钠组分的支架组均显示较高的新骨生成和较少的破骨细胞反应,这说明体内阿仑膦酸钠从聚己内酯涂层的磷酸三钙支架上释放可以诱导早期成骨增加。在此基础上,Tarafder等于2015年研究出[31]在3D打印且微波烧结而制作的(磷酸三钙)支架表面增加氧化锶和氧化镁涂层,并对大鼠股骨远中端的缺损进行修复,跟单纯磷酸三钙支架相比较,含氧化锶和氧化镁涂层的支架可以更快地诱导矿化骨钙蛋白和一型胶原的生成,结果显示涂层组可以通过加速成骨和成血管来早期修复骨缺损。 除了微量元素,一些蛋白也对成骨有促进作用,已知骨形成蛋白家族成员约有43种,而骨形态发生蛋白2是其中成骨活性最强的一种。 Shim[32]于2014年研究出一个重组人骨形态发生蛋白2慢传递系统,分别利用胶原和明胶包裹重组人骨形态发生蛋白2,前者长效传递,时间长达28 d,后者短效传递,时间为7 d左右。对于人骨髓间充质干细胞来说,5 mg/L的重组人骨形态发生蛋白2剂量是无细胞毒性的,体内试验表明在4周和8周时长效释放模式的聚己内酯/PLGA/胶原/重组人骨形态发生蛋白2复合支架显示了良好的修复性能且无组织炎性反应,而短效组则在4周左右的时候发生了大量巨噬细胞反应。 而2015年Dadsetan等[33]将微量元素与骨形成蛋白结合,在多孔聚酯支架表面涂布三种磷酸钙涂层:镁替代β-磷酸三钙(β-TCMP)、碳酸化羟基磷灰石(SBM)和双相磷酸钙(BCP),且分别负载有不同剂量的重组人骨形态发生蛋白2,3组支架都可以有效维持重组人骨形态发生蛋白2的长效释放,组织学结果显示在支架表层骨生长迅速,表明在有涂层的支架组可以观察到良好的骨整合和骨诱导,鉴于重组人骨形态发生蛋白2对新骨生成的促进作用,结果进一步说明支架涂层和重组人骨形态发生蛋白2具有协同作用。 2.5 其它 目前关于3D打印组织工程骨支架的研究重点不仅体现在支架和细胞的相互反应方面,同时涉及其与宿主之间的相互关联。为了研究细胞外基质对生物反应的影响,Kumar等[34]在2016年发表的研究中,制造出模仿天然细胞外基质的成分应用于3D打印烧结的羟基磷灰石支架,细胞外基质利用冻融循环法进行脱细胞处理,结果表明在脱细胞基质中的支架表面,蛋白、肌动蛋白和黏着斑蛋白有显著的高表达,表明基质脱细胞处理后的支架可以提供一个可以促进细胞-细胞以及细胞-支架反应的有利环境,所以对于支架外基质的处理也为3D打印支架更好地修复骨缺损提供新思路。 "
| [1]Cho-Lee GY, García-Díez EM, Nunes RA,et al.Review of secondary alveolar cleft repair.AnnMaxillofac Surg.2013; 3 (1):46-50.[2]Bergland O, Semb G, Abyholm FE. Elimination of the residual alveolar clefts by secondary bone grafting and subsequent orthodontic treatment. Cleft Palate J. 1986; 23(3):175-205.[3]黄迪炎,陈海龙.先天性唇腭裂治疗现状[J].实用医药杂志, 2003, 20(1):68-70.[4]毛萌,朱军.出生缺陷监测研究现状[J].实用儿科临床杂志, 2009, 24(11):801-803.[5]Erverdi N, Usumez S,Solak A, et al. Noncompliance open-bite treatment with zygomatic anchorage.Angle Orthod.2007;77(6):986-990.[6]Umemori M, Sugawara J, Mitani H, et al. Skeletal anchorage system for open-bite correction.Am J OrthodDentofacial Orthop.1999;115(2): 166-174.[7]Kuroda S, Katayama A, Takano -Yamamoto T. Severe anterior open-bite case treated using titanium screw anchorage. Angle Orthod.2004;74(4): 558-567.[8]Langer R, Vacanti JP.Tissue engineering.Science.1993;260(5 110):920-926.[9]曹谊林. 组织工程学理论与实践[M].上海:上海科学技术出版社,2004:3-8.[10]Lee M, Wu BM.Recent advances in 3D printing of tissue engineering scaffolds. Methods Mol Biol.2012;868: 257-267.[11]Ghosh S,Parker ST,Wang X,et al.Direct-write assembly of microperiodic silk fibroin scaffolds for tissue engineering applications. AdvFunct Mater 2008;18:1883-1889.[12]Therriault D, White SR, Lewis JA.Chaotic mixing in three-dimensional microvascular networks fabricated by direct-write assembly. Nat Mater 2003;2:265-271.[13]Wu C, Luo Y, Cuniberti G,et al.Three-dimensional printing of hierarchical and tough mesoporous bioactive glass scaffolds with a controllable pore architecture, excellent mechanical strength and mineralization ability. ActaBiomater.2011;7:2644-2650.[14]Ozbolat IT, Yu Y.Bioprinting toward organ fabrication: challenges and future trends. IEEE Trans Biomed Eng.2013; 60(3):691-699.[15]Arcos D, Izquierdo-Barba I, Vallet-Regi M. Promising trends of bioceramics in the biomaterials field. J Mater Sci Mater Med. 2009;20:447-455.[16]Seitz H, Rieder W, Irsen S,et al. Three-Dimensional Printing of Porous Ceramic Scaffolds for Bone Tissue Engineering. Biomed Mater Res Part B: ApplBiomater 2005;74(2): 782-788.[17]Simon JL, Rekow ED, Thompson VP,et al. MicroCT analysis of hydroxyapatite bone repair scaffolds created via three-dimensional printing for evaluating the effects of scaffold architecture on bone ingrowth. Biomed Mater Res. 2008;85(2): 371-377.[18]Khoda AK, Ozbolat IT, Koc B.A functionally gradient variational porosity architecture for hollowed scaffolds fabrication. Biofabrication 2011;3(3) 034106.[19]Fedorovich NE, Kuipers E, Gawlitta D,et al.Scaffold Porosity and Oxygenation of Printed Hydrogel Constructs Affect Functionality of Embedded Osteogenic Progenitors. Tissue Eng Part A. 2011;17(19-20):2473-2486. [20]Sachlos E, Wahl DA, Triffitt JT, et al.The impact of critical point drying with liquid carbon dioxide on collagen– hydroxyapatite composite scaffolds. Acta Biomater. 2008;4(5): 1322-1331. [21]Butscher A, Bohner M, Doebelin N, et al. Newdepowdering- friendly designs for three-dimensional printing of calcium phosphate bone substitutes.Acta Biomater. 2013;9(11): 9149-9158.[22]Fedorovich NE, Schuurman W, Wijnberg HM,et al. Biofabrication of Osteochondral Tissue Equivalents by Printing Topologically Defined, Cell-Laden Hydrogel Scaffolds. Tissue Eng Part C Methods. 2012;18(1):33-44. [23]Rath SN, Strobel LA, Arkudas A,et al.Osteoinduction and survival of osteoblasts and bone-marrow stromal cells in 3D biphasic calcium phosphate scaffolds under static and dynamic culture conditions. J Cell Mol Med. 2012;16(10): 2350-2361[24]Korpela J, Kokkari A, Korhonen H, et al.Biodegradable and bioactive porous scaffold structures prepared using fused deposition modeling. J Biomed Mater Res B Appl Biomater. 2013;101(4):610-619.[25]Lee JY, Choi B, Wu B, et al.Customized biomimetic scaffolds created by indirect threedimensional printing for tissue engineering. Biofabrication. 2013;5(4):045003.[26]Inzana JA, Olvera D, Fuller SM,et al.3D printing of composite calcium phosphate and collagen scaffolds for bone regeneration. Biomaterials. 2014;35(13):4026-4034.[27]Gonçalves EM, Oliveira FJ, Silva RF, et al.Three-dimensional printed PCL-hydroxyapatite scaffolds filled with CNTs for bone cell growth stimulation. J Biomed Mater Res B Appl Biomater. 2016;104(6):1210-1219.[28]Fielding G, Bose S.SiO2 and ZnO dopants in three-dimensionally printed tricalcium phosphate bone tissue engineering scaffolds enhance osteogenesis and angiogenesis in vivo. Acta Biomater. 2013;9(11):9137-9148.[29]Tarafder S, Davies NM, Bandyopadhyay A, et al.3D printed tricalcium phosphate scaffolds: Effect of SrO and MgO doping on in vivo osteogenesis in a rat distal femoral defect model.Biomater Sci. 2013 December 1; 1(12): 1250-1259.[30]Tarafder S, Bose S.Polycaprolactone-Coated 3D Printed Tricalcium Phosphate Scaffolds for Bone Tissue Engineering: In Vitro Alendronate Release Behavior and Local Delivery Effect on In Vivo Osteogenesis. ACS Appl Mater Interfaces. 2014;6(13):9955-9965.[31]Tarafder S, Dernell WS, Bandyopadhyay A, et al.SrO- and MgO-doped microwave sintered 3D printed tricalcium phosphate scaffolds: Mechanical properties and in vivo osteogenesis in a rabbit model. J Biomed Mater Res B Appl Biomater. 2015;103(3):679-690.[32]Shim JH, Kim SE, Park JY,Three-Dimensional Printing of rhBMP-2-Loaded Scaffolds with Long-Term Delivery for Enhanced Bone Regeneration in a Rabbit Diaphyseal Defect. Tissue Eng Part A. 2014;20(13-14):1980-1992.[33]Dadsetan M, Guda T, Runge MB, et al.Effect of calcium phosphate coating and rhBMP-2 on bone regeneration in rabbit calvaria using poly(propylene fumarate) scaffolds. Acta Biomater. 2015;18:9-20.[34]Kumar A, Nune KC, Misra RD. Biological functionality of extracellular matrix-ornamented three-dimensional printed hydroxyapatite scaffolds. J Biomed Mater Res A. 2016; 104(6):1343-1351.[35]Vorys GC, Bai H, Chandhanayingyong C,et al. Optimal internal fixation of anatomically shaped synthetic bone grafts for massive segmental defects of long bones. Clin Biomech (Bristol, Avon). 2015;30(10):1114-1118.[36]Vo TN, Ekenseair AK, Spicer PP, et al. In vitro and in vivo evaluation of self-mineralization and biocompatibility of injectable, dual-gelling hydrogels for bone tissue engineering. J Control Release. 2015; 205:25-34.[37]Huang J, Tian B, Chu F, et al. Rapid maxillary expansion in alveolar cleft repaired with a tissue-engineered bone in a canine model. J Mech Behav Biomed Mater. 2015;48:86-99. |
| [1] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [2] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [3] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [4] | He Yunying, Li Lingjie, Zhang Shuqi, Li Yuzhou, Yang Sheng, Ji Ping. Method of constructing cell spheroids based on agarose and polyacrylic molds [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 553-559. |
| [5] | He Guanyu, Xu Baoshan, Du Lilong, Zhang Tongxing, Huo Zhenxin, Shen Li. Biomimetic orientated microchannel annulus fibrosus scaffold constructed by silk fibroin [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 560-566. |
| [6] | Chen Xiaoxu, Luo Yaxin, Bi Haoran, Yang Kun. Preparation and application of acellular scaffold in tissue engineering and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 591-596. |
| [7] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [8] | Shen Jiahua, Fu Yong. Application of graphene-based nanomaterials in stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 604-609. |
| [9] | Zhang Tong, Cai Jinchi, Yuan Zhifa, Zhao Haiyan, Han Xingwen, Wang Wenji. Hyaluronic acid-based composite hydrogel in cartilage injury caused by osteoarthritis: application and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 617-625. |
| [10] | Li Hui, Chen Lianglong. Application and characteristics of bone graft materials in the treatment of spinal tuberculosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 626-630. |
| [11] | Gao Cangjian, Yang Zhen, Liu Shuyun, Li Hao, Fu Liwei, Zhao Tianyuan, Chen Wei, Liao Zhiyao, Li Pinxue, Sui Xiang, Guo Quanyi. Electrospinning for rotator cuff repair [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 637-642. |
| [12] | Guan Jian, Jia Yanfei, Zhang Baoxin , Zhao Guozhong. Application of 4D bioprinting in tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 446-455. |
| [13] | Liu Jiali, Suo Hairui, Yang Han, Wang Ling, Xu Mingen. Influence of lay-down angles on mechanical properties of three-dimensional printed polycaprolactone scaffolds [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2612-2617. |
| [14] | Huang Bo, Chen Mingxue, Peng Liqing, Luo Xujiang, Li Huo, Wang Hao, Tian Qinyu, Lu Xiaobo, Liu Shuyun, Guo Quanyi . Fabrication and biocompatibility of injectable gelatin-methacryloyl/cartilage-derived matrix particles composite hydrogel scaffold [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2600-2606. |
| [15] | Fang Xiaoyang, Tang Tian, Wang Nan, Qian Yuzhang, Xie Lin. Repair and regenerative therapies of the annulus fibrosus [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(10): 1582-1587. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||