Chinese Journal of Tissue Engineering Research
Previous Articles Next Articles
Influencing factors of fixation strength of pedicle screws
Yin Jian-xin
- Third Department of Orthopedics, Xinwen Mining Industry Group Central Hospital, Taian 271219, Shandong Province, China
-
Received:2013-06-20Revised:2013-08-17Online:2013-10-22Published:2013-11-02 -
About author:Yin Jian-xin, Associate chief physician, Third Department of Orthopedics, Xinwen Mining Industry Group Central Hospital, Taian 271219, Shandong Province, China xinwenyjx@126.com
CLC Number:
Cite this article
Yin Jian-xin. Influencing factors of fixation strength of pedicle screws[J]. Chinese Journal of Tissue Engineering Research, doi: 10.3969/j.issn.2095-4344.2013.43.022.
share this article
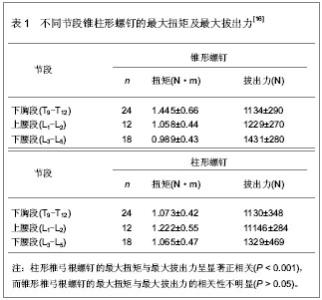
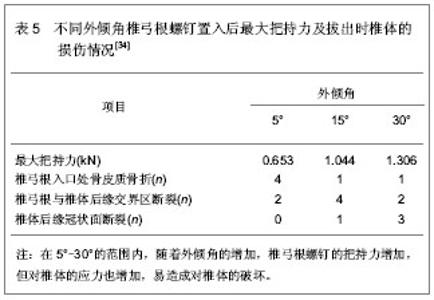
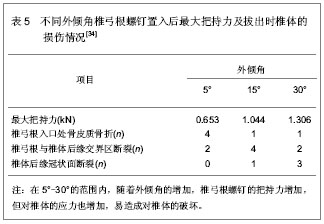
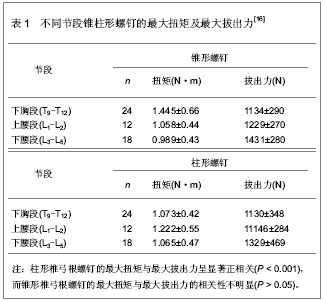
2 影响椎弓根螺钉固定强度的相关因素 Influencing factors of fixation strength of pedicle screws 2.1 椎弓根螺钉的自身设计对固定强度的影响 2.1.1 椎弓根螺钉的形状 李超等[16]比较了锥形与柱形椎弓根螺钉在下胸段及腰段的生物力学差异性及影响因素。将6具成人新鲜T9-L5脊柱标本分解为54个椎体标本,随机选取一侧按标准方法放置特制试验用直径5.5 mm锥形螺钉,然后在MTS力学试验机上先后测量其最大扭矩及最大拔出力,在对侧以同样的方法进行5.5 mm柱形螺钉的实验,为了便于比较,实验所采用的两种椎弓根螺钉为等直径、等长度、等螺距,而且每次进钉的长度相等,结果见表1。"
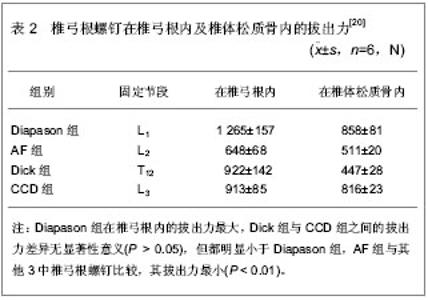
杨惠林等[17]在分析504例弓根内固定治疗胸腰椎骨折中的失误和并发症的基础上,对螺钉进行改进,螺钉外直径不变,内直径为锥形,使整个钉部的强度从钉尖钉钉肩部呈均匀增加,经生物力学实验研究和临床应用,证明这种设计具有良好的复位作用、椎管间接减压作用和足够的抗压抗扭强度,从而克服了原有螺钉在螺纹与螺轴交界处强度突变而致应力集中易发生断钉的弱点。谭映军等[18]对内锥及外锥形椎弓根螺钉的生物力学进行了比较,结果显示外锥形椎弓根螺钉在正常椎弓根内的最大拨出力为(996.17±54.69) N,内锥形椎弓根螺钉在正常椎弓根内的最大拔出力为(667.17±24.74) N,差异有显著性意义,因此,椎弓根螺钉设计成外锥形可提高螺钉的拔出力。2.1.2 椎弓根螺钉的螺纹设计 椎弓根螺钉的松动和拔出直接影响内固定器的固定效果,这与椎弓根螺钉的螺纹形状有一定的关系。从物理学上讲,单位面积上压力越大,其压强也越大,因此,螺钉的螺纹与骨的接触面越大,相应的压强就越小,要使骨-螺钉的界面破坏,所需的压力就越大。Inceoglu等[19]研究发现不对称螺纹的圆锥形椎弓根螺钉较V形螺纹的圆锥形椎弓根螺钉具有更显著的旋入力矩,可能会提供更强的固定强度。潘显明等[20]为了解不同形状螺纹的椎弓根螺钉在椎弓根内的拔出力的大小,给临床应用不同类型的经椎弓根内固定器提供实验依据,方法采用4种形状螺纹的椎弓根螺钉,4种螺钉长45 mm,螺纹长40 mm:Diapason的螺高2 mm,尖端外径6 mm,尾端外径7 mm,螺纹深0.5 mm;AF的螺高2 mm,外径6 mm,尖端螺纹深0.7 mm;Dick的螺高2 mm,外径6 mm,螺纹深0.5 mm;CCD的螺高3 mm,外径6 mm,螺纹深1 mm,分别在椎弓根内及椎体松质骨中进行拔出试验,观察其拔出力的大小情况,结果见表2。"
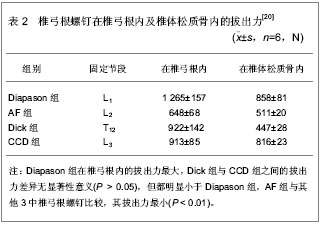

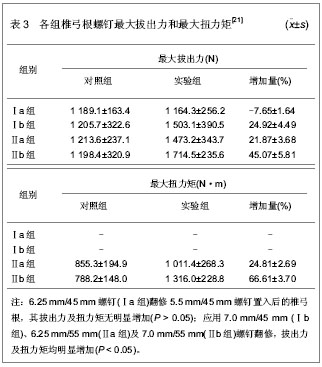
实验结果显示,在椎弓根内,Diapason的拔出力最大,CCD及Dick次之,AF的拔出力最小,而在松质骨内,Diapason及CCD则无差别,AF其次,Dick拔出力最小,说明外锥螺纹式的螺钉Diapason可在各种不同类型的骨折中使用。同时也说明,椎弓根螺钉在皮质骨中较松质骨中有更大的抗拔出力,如骨螺钉界面的皮质骨较多,其抗拔出力较大,螺纹切入骨皮质的多少与螺钉的直径相关,直径越粗,切除的则越多,因此为了消除椎弓根螺钉在椎弓根的骨皮质中切入不均而造成的误差,实验中设计了再椎体松质骨中的拔出试验。2.1.3 椎弓根螺钉的直径 研究者多用轴向拔出力评价椎弓根螺钉固定强度,因为轴向拔出力主要由螺钉和其周围的骨组织之间的剪切应力所决定,可以较好地反映骨-螺钉界面结合的初始强度。椎弓根螺钉的轴向拔出力受许多因素影响,包括:螺钉的自身结构、骨密度及置钉方法等。丁宇等[21]探讨不同直径与长度螺钉翻修及骨水泥强化后椎弓根固定的强度,评价其生物力学效果。采用10具新鲜成人尸体T10-L5节段共80个椎体标本,首先置入5.5 mm/45 mm椎弓根螺钉作为对照组,再将脊椎标本随机平分为Ⅰ、Ⅱ两大组。Ⅰ组中40个椎体各随机选择一侧椎弓根应用6.25 mm/45 mm螺钉翻修(Ⅰa组),另一侧椎弓根应用7.0 mm/45 mm螺钉翻修(Ⅰb组);Ⅱ组中40个椎体各随机选择一侧椎弓根应用6.25 mm/55 mm螺钉翻修(Ⅱa组),另一侧椎弓根应用7.0 mm/55 mm螺钉翻修(Ⅱb组)。在美国产858Mini-MTS生物力学实验机上测试最大拔出力及最大扭力矩,并进行统计分析,结果见表3。"
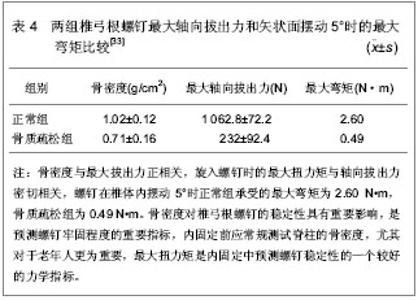
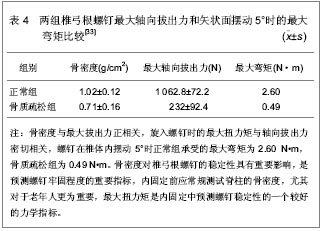
2.1.4 椎弓根螺钉的长度 王正等[22]探讨胸腰椎骨折采用椎弓根螺钉内固定,其疗效与螺钉固定的长度因素的相关性,为此进行生物力学分析,为临床手术提供依据。McKinley等[23]通过研究发现相对于40 mm和45 mm长的椎弓根螺钉,35 mm长的椎弓根螺钉在椎体内所承受的弯曲力矩增加16%,因此,建议临床上应尽量使用400 mm以上的螺钉,椎弓根螺钉进入椎体足够深度,不但可以获得与骨组织的牢固结合,而且可以有效的握持整个椎体。治疗中应注意椎弓根螺钉固定相关因素,这对提高预后质量,减少并发症起着重要作用。 Krag等[24]研究发现椎弓根螺钉植入深度增加骨-螺钉结合强度,椎弓根螺钉在腰椎椎体内5 mm长度的差异就可以产生螺钉固定效果的差异。需要注意的是螺钉长度越长越容易破坏椎体前柱,有引起内脏及血管损伤的风险。Brantley等[25]研究发现在骨质疏松骨质中,加入螺钉截面积占椎弓根截面积70%以上时,增加螺钉长度能有效的提高骨质疏松性骨折的固定强度。但增加螺钉长度,相应增加固定深度是受椎体大小及椎弓根长度限制的。Polly等[26]认为增加椎弓根螺钉长度不能明显增加固定强度,椎弓根螺钉直径增加1 mm并不能显著增加其与骨界面的切合,若同时增加直径和长度,则可增加螺钉置入的最大扭矩,因此,两者会发生协同作用增加固定强度。 2.1.5 椎弓根螺钉的材料 Eulenberger等[27]通过动物实验表明钛合金螺钉能够较多的与骨结合,比不锈钢螺钉具有更大的拔出力。目前市场上有很多类型的椎弓根螺钉装置出现,相对不锈钢而言,行钛合金椎弓根螺钉装置进内固定后进行CT和磁共振成像检查时对其图像产生的干扰和假象较小,有利于植骨块和神经方面的随访和评估。 孙常太[28]从组织学和力学上比较钛合金与不锈钢椎弓根螺钉的骨-螺钉介面的区别。实验结果表明,钛合金比不锈钢椎弓根螺钉具有较高的扭转扭矩、硬度,骨与螺钉表面直接接触在钛合金组占43.8%,而不锈钢组仅仅29.4%,两者具有明显差别(P < 0.05),两种材料的螺钉表面都有骨的直接结合,但钛合金具有更多的骨结合,这种结合不是分子或化学键之间的结合,而是由于钛合金本身的硬度和特有的金属表面性质决定的。 2.2 椎弓根解剖因素对固定强度的影响 2.2.1 椎弓根结构特点 Hirano等[29]通过对椎弓根骨质结构的研究认为椎弓根皮质下骨质密度较骨小梁高,椎弓根螺钉固定纵向负载强度的80%,拔出强度的60%取决于椎弓根而不是椎体,认为螺钉的螺纹应完全啮合于椎弓根内外侧皮质下骨质才能达到最大固定强度。Zdeblick等[30]研究了椎弓根宽度与拔出力量的关系,在螺钉直径不变时,椎弓根宽度与螺钉的拔出力量呈负相关。 2.2.2 椎弓根椎体的骨密度 椎体骨密度对椎弓根螺钉固定的强度具有重要影响,是预测螺钉固定的稳定性的重要指标。Okuyama等[31]通过测量标准的骨密度,研究与拔出强度的关系,认为骨密度每降低10 mg/cm3,其拔出力量大约减少60 N。Yamagata等[32]研究中也发现骨密度与拔出力相关,在骨质疏松的病例中,固定强度明显降低。 李增春等[33]探讨骨密度、对椎弓根螺钉系统固定的影响。采用6具新鲜腰段脊柱标本,测试每个椎体的骨密度,并游离成单个完整椎体标本,按骨密度 0.9 g/cm2为正常值的最低限。将标本分为正常组和骨质疏松组。按标准操作安置椎弓根螺钉,应用生物力学方法,测试螺钉最大轴向拔出力和矢状面摆动1°-5°时的弯矩,结果见表4。"
| [1] Boos N,Webb JK.Pedicle screw fixation in spinal disorders: a European view.Eur Spine J.1997;6(1):2-18. [2] 曹正霖,王波,赵卫东,等.新型寰椎钩棒及椎板钩联合枢椎椎弓根螺钉内固定的生物力学[J].中华创伤骨科杂志,2013,15(6): 514-516. [3] 林华杰,徐荣明,刘观燚.下颈椎后路螺钉固定的生物力学研究进展[J].中国骨伤,2011,24(6):530-533. [4] Barber JW,Boden SD,Ganey T,et al.Biomechanical study of lumbar pedicle screws: does convergence affect axial pullout strength?J Spinal Disord.1998;11(3):215-220. [5] Ruland CM,McAfee PC,Warden KE,et al.iangulation of pedicular instrumentation. A biomechanical analysis.ine (Phila Pa 1976).1991;16(6):270-276. [6] Balabaud L,Gallard E,Skalli W,et al.Biomechanical evaluation of a bipedicular spinal fixation device: three different strength tests.Eur Spine J.2003;12(5):480-486. [7] Roy-Camille R,Saillant G,Mazel C.Internal fixation of the lumbar spine with pedicle screw plating.Clin Orthop Relat Res.1986;(203):7-17. [8] 罗集贤,尹飞,宋世凯,等.椎弓根螺钉不同角度偶联的生物力学研究[J].中国实验诊断学,2013,17(3):575-576. [9] 李现令,李现今,张学军,等.脊柱椎弓根螺钉应用的生物力学特征[J].中国组织工程研究与临床康复,2011,15(30):5640-5645. [10] Steffee AD,Biscup RS,Sitkowski DJ.ental spine plates with pedicle screw fixation. A new internal fixation device for disorders of the lumbar and thoracolumbar spine.Clin Orthop Relat Res.1986;(203):45-53. [11] 严雪港,姜跃国,桂剑英,等.微创经皮椎弓根螺钉内固定治疗腰椎骨折伴骨质疏松失败一例分析[J].中国全科医学,2013,16(2):224-225. [12] 刘瑶瑶,孙东,张泽华,等.用于骨质疏松椎体固定的椎弓根螺钉进展[J].中国矫形外科杂志 ,2011,19(23):1982-1986. [13] 李明,赵颖川,朱晓东,等.后路全椎弓根螺钉系统治疗青少年特发性脊柱侧凸疗效分析[J].中华外科杂志,2010,48(6):410-414. [14] 中国知网.中国学术期刊总库[DB/OL].2013-5-15.https://www.cnki.net [15] SCI数据库.Web of Sciencevia ISI Web of Knowledge[DB/OL].2013-5-15.http://ip-science.thomsonreuters.com/mjl [16] 李超,阮狄克,丁宇,等.锥形与柱形椎弓根螺钉的生物力学研究[J].脊柱外科杂志,2004,2(4):220-223. [17] 杨慧林,唐天驷.胸腰椎骨折经椎弓根内固定治疗中的失误和并发症[J].中华骨科杂志,1996,16(6):356. [18] 谭映军,潘显明,陈乾一,等.内锥及外锥形椎弓根螺钉的生物力学研究[J].骨与关节损伤杂志,2001,16(6):441-443. [19] Inceoglu S,Ferrara L,McLain RF.Pedicle screw fixation strength: pullout versus insertional torque.ine J.2004;4(5):513-518. [20] 潘显明,谭映军,张波,等.椎弓根螺钉的螺纹形状与拔钉生物力学[J].第四军医大学学报,2002,23(5):447-450. [21] 丁宇,阮狄克,李超,等.经椎弓根螺钉内固定翻修术的生物力学研究[J].中国脊柱脊髓杂志,2004,14(7):409-413. [22] 王正,沈国平,陈伟兵,等.椎弓根螺钉内固定稳定性的生物力学分析[J].中国临床康复,2004,8(14):2755-2757. [23] McKinley TO,McLain RF,Yerby SA,et al.Characteristics of pedicle screw loading. Effect of surgical technique on intravertebral and intrapedicular bending moments.Spine (Phila Pa 1976).1999;24(1):18-24. [24] Krag MH,Beynnon BD,Pope MH,et al.Depth of insertion of transpedicular vertebral screws into human vertebrae: effect upon screw-vertebra interface strength.J Spinal Disord.1988;1(4):287-294. [25] Brantley AG,Mayfield JK,Koeneman JB,et al.The effects of pedicle screw fit. An in vitro study.Spine (Phila Pa 1976).1994;19(15):1752-1758. [26] Polly DW Jr,Orchowski JR,Ellenbogen RG.Revision pedicle screws. Bigger, longer shims--what is best?Spine (Phila Pa 1976).1998;23(12):1374-1379. [27] Eulenberger J, Steinemann SG.Removal torques of small screws of steel and titanium with different surfaces.Unfallchirurg.1990;93(3):96-99. [28] 孙常太.钛合金及不锈钢椎弓根螺丝钉骨界面力学及组织学分析[D].北京:中国协和医科大学,1999:1-30. [29] Hirano T,Hasegawa K,Takahashi HE,et al.Structural characteristics of the pedicle and its role in screw stability.Spine (Phila Pa 1976).1997;122(21):2504-2509. [30] Zdeblick TA,Kunz DN,Cooke ME,et al. Pedicle screw pullout strength. Correlation with insertional torque.Spine (Phila Pa 1976).1993;18(12):1673-1676. [31] Okuyama K,Sato K,Abe E,et al.Stability of transpedicle screwing for the osteoporotic spine. An in vitro study of the mechanical stability.Spine (Phila Pa 1976).1993;18(15):2240-2245. [32] Yamagata M,Kitahara H,Minami S,et al.Mechanical stability of the pedicle screw fixation systems for the lumbar spine.Spine (Phila Pa 1976).1992;17(3):51-54. [33] 李增春,志玉,王以进.骨密度对椎弓根螺钉系统固定的影响之生物力学研究[J].中华骨科杂志,1998,18(5):293-297. [34] 陈群,金正帅,曹晓健,等.不同外倾角的脊柱椎弓根螺钉内固定效果的生物力学评价[J].河北医学,2005,11(5):433-435. [35] 付长峰,刘一,张绍昆,等.胸椎旁路法植入椎弓根螺钉的力学实验研究[J].吉林大学学报(医学版),2006,32(2):275-277. [36] Linhardt O,Perlick L,Renkawitz T,et al.lout resistance of conventional pedicle screw implantation in comparison to fluoroscopic computer-assisted technique.lbl Chir.2006;131(5):407-410. |
| [1] | Wang Jianping, Zhang Xiaohui, Yu Jinwei, Wei Shaoliang, Zhang Xinmin, Xu Xingxin, Qu Haijun. Application of knee joint motion analysis in machanism based on three-dimensional image registration and coordinate transformation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(在线): 1-5. |
| [2] | Zhang Yufang, Lü Meng, Mei Zhao. Construction and verification of a full spine biomechanical model of adolescent scoliosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1351-1356. |
| [3] | Bai Zixing, Cao Xuhan, Sun Chengyi, Yang Yanjun, Chen Si, Wen Jianmin, Lin Xinxiao, Sun Weidong. Construction and biomechanical analysis of ankle joint finite element model in gait cycle [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1362-1366. |
| [4] | Liu Feng, Feng Yi. Finite element analysis of different Kirschner wire tension bands on transverse patella fractures during gait cycle [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1367-1371. |
| [5] | Jiang Huanchang, Zhang Zhaofei, Liang De, Jiang Xiaobing, Yang Xiaodong, Liu Zhixiang. Comparison of advantages between unilateral multidirectional curved and straight vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1407-1411. |
| [6] | Duan Chao, Shang Xiaoqiang, Duan Xianglin, Yang Ping, Tao Shengxiang. Stability of patellar claw versus loop plate combined with patellar claw for the treatment of comminuted fractures of the lower pole of the patella [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 934-937. |
| [7] | Wen Mingtao, Liang Xuezhen, Li Jiacheng, Xu Bo, Li Gang. Mechanical stability of Sanders II type calcaneal fractures fixed by two internal fixation methods [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 838-842. |
| [8] | Huang Hao, Hong Song, Wa Qingde. Finite element analysis of the effect of femoral component rotation on patellofemoral joint contact pressure in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 848-852. |
| [9] | Zheng Yongze, Zheng Liqin, He Xingpeng, Chen Xinmin, Li Musheng, Li Pengfei, Lin Ziling. Extended finite element modeling analysis of femoral neck fracture based on ABAQUS software [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 853-857. |
| [10] | Liu Yuhang, Zhou Jianqiang, Xu Xuebin, Qu Xingyue, Li Ziyu, Li Kun, Wang Xing, Li Zhijun, Li Xiaohe, Zhang Shaojie. Establishment and validation of finite element model of lower cervical spine in 6-year-old children [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 870-874. |
| [11] | Baibujiafu·Yelisi, Renaguli·Maihemuti, Aizimaitijiang·Saiyiti, Wang Junxiang, Nijiati·Tuerxun. Stress analysis of maxillary central incisor crown implant restoration in different occlusal modes [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 567-572. |
| [12] | Li Yanting, Chen Jian, Liu Menglan, Ren Manman, Zhong Weihong, Chen Changxing. Three-dimensional finite element analysis of Daogaijinbei manipulation on lumbar intervertebral disc biomechanics [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 340-343. |
| [13] | Chen Jinmin, Chen Suisheng, Ding Jing, Xia Baoquan, Luo Xiaojia, Lu Chenghai. Stability of balloon dilation with injectable calcium sulfate cement for tibial plateau fractures [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 414-418. |
| [14] | Liu Zemin, Lü Xin. Application of intramedullary nailing in the treatment of long tubular bone fractures of the extremities: reaming and non-reaming [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 461-467. |
| [15] | Li Lu, Tang Wen. Screw placement in posterior route pedicle on subaxial cervical spine: how to improve the therapeutic effect with the development of artificial intelligence [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 474-479. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||