Chinese Journal of Tissue Engineering Research ›› 2020, Vol. 24 ›› Issue (27): 4398-4405.doi: 10.3969/j.issn.2095-4344.2797
Previous Articles Next Articles
A network meta-analysis of different surgical methods in the treatment of lumbar disc herniation
Xiang Xi1, Si Qunchao1, Cheng Weiyi2, Cao Ping1, Zheng Jinpeng1, Hu Bing1
- 1Department of Orthopedics, Tianyou Hospital Affiliated to Wuhan University of Science and Technology, Wuhan 430000, Hubei Province, China; 2Maternal and Child Health Care Hospital of Hubei Province, Wuhan 430000, Hubei Province, China
-
Received:2019-12-24Revised:2019-12-27Accepted:2020-01-22Online:2020-09-28Published:2020-09-10 -
Contact:Hu Bing, Chief physician, Associate professor, Department of Orthopedics, Tianyou Hospital Affiliated to Wuhan University of Science and Technology, Wuhan 430000, Hubei Province, China -
About author:Xiang Xi, Master candidate, Department of Orthopedics, Tianyou Hospital Affiliated to Wuhan University of Science and Technology, Wuhan 430000, Hubei Province, China
CLC Number:
Cite this article
Xiang Xi, Si Qunchao, Cheng Weiyi, Cao Ping, Zheng Jinpeng, Hu Bing. A network meta-analysis of different surgical methods in the treatment of lumbar disc herniation[J]. Chinese Journal of Tissue Engineering Research, 2020, 24(27): 4398-4405.
share this article
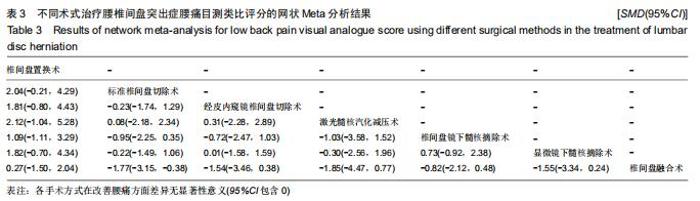
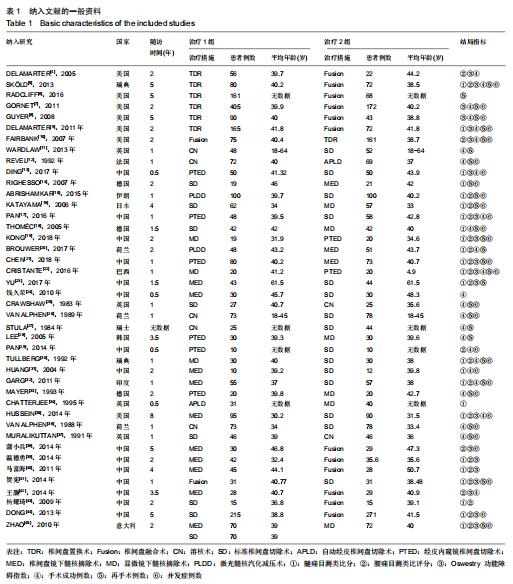
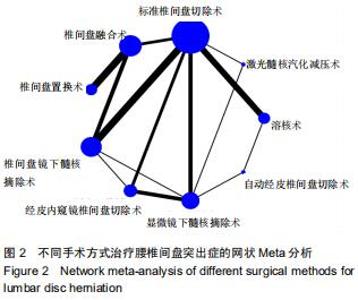
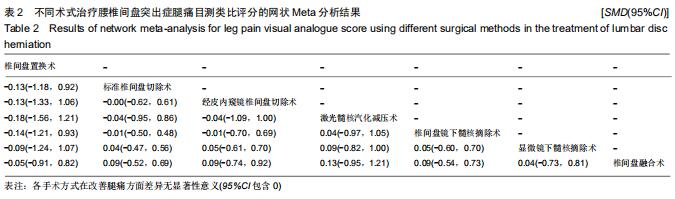
2.3.2 腰痛目测类比评分 纳入的42个研究中有23个报告了患者术后腰痛的随访目测类比评分[4-5,10,15-17,19-23,29-30,32,35,38-45]。纳入患者2 719例,其中腰椎间盘置换术297例、椎间盘融合术612例、标准椎间盘切除术552例、椎间盘镜下髓核摘除术426例、显微镜下髓核摘除术291例、经皮内窥镜腰椎间盘切除术178例及经皮激光椎间盘减压术148例。各手术方式结果比较差异无显著性意义,见表3,其中标准椎间盘切除术vs.椎间盘融合术比较差异有显著性意义,缓解腰痛疗效排序为腰椎间盘置换术>腰椎间盘融合术>椎间盘镜下髓核摘除术>经皮内窥镜腰椎间盘切除术>显微镜下髓核摘除术>经皮激光椎间盘减压术>标准椎间盘切除术。 "

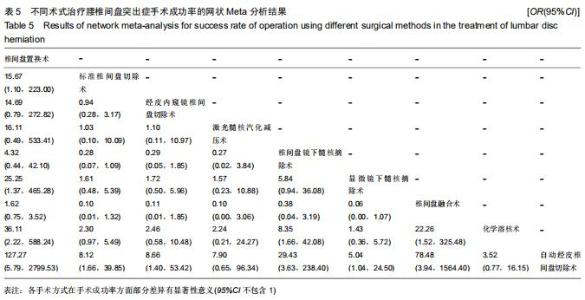
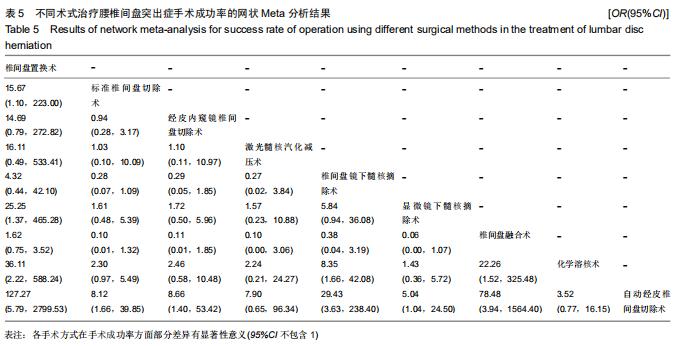
2.3.4 手术成功率 纳入的42个研究中有28个报告了患者术后随访的手术成功率[4-5,7-13,17-18,20,22,24-37,42]。纳入患者3 259例,其中腰椎间盘置换术940例、椎间盘融合术480例、标准椎间盘切除术703例、椎间盘镜下髓核摘除术218例、显微镜下髓核摘除术233例、经皮内窥镜腰椎间盘切除术178例、经皮激光椎间盘减压术48例、化学溶核术359例及自动经皮腰椎间盘切除术100例。各手术方式结果比较部分差异有显著性意义,见表5,手术成功率方面排序为腰椎间盘置换术>腰椎间盘融合术>椎间盘镜下髓核摘除术>经皮内窥镜腰椎间盘切除术>标准椎间盘切除术>经皮激光椎间盘减压术>显微镜下髓核摘除术>化学溶核术>自动经皮腰椎间盘切除术。 "
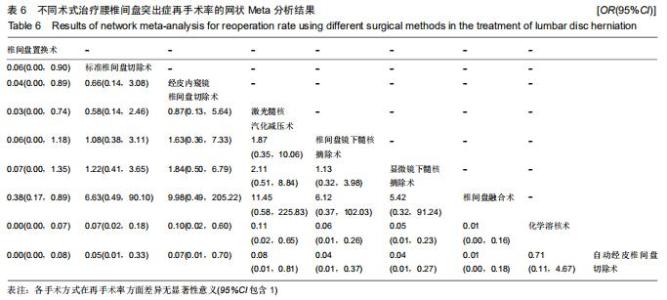
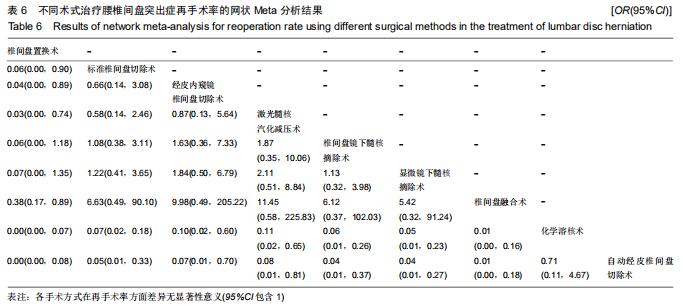
2.3.5 再手术率 纳入的42个研究中有29个报告了患者术后随访的再手术率[5-12,14-16,18-23,25-28,30,32-33,36-37,41,45]。纳入患者4 461例,其中腰椎间盘置换术1 062例、椎间盘融合术801例、标准椎间盘切除术1 080例、椎间盘镜下髓核摘除术357例、显微镜下髓核摘除术381例、经皮内窥镜腰椎间盘切除术170例、经皮激光椎间盘减压术148例、化学溶核术362例及自动经皮腰椎间盘切除术100例。各手术方式结果比较差异无显著性意义,见表6,再次手术率方面排序为腰椎间盘置换术>腰椎间盘融合术>显微镜下髓核摘除术>椎间盘镜下髓核摘除术>标准椎间盘切除术>经皮内窥镜腰椎间盘切除术>经皮激光椎间盘减压术>化学溶核术>自动经皮腰椎间盘切除术。 "
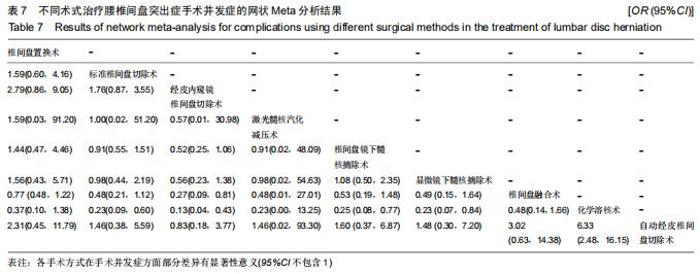
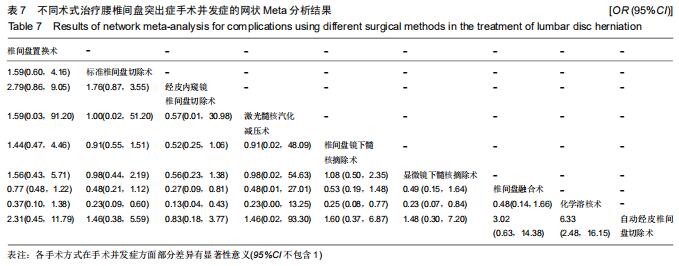
2.3.6 并发症发生率 纳入的42个研究中有29个报告了术后随访的并发症发生率[5,7-10,12-19,21-22,25-26,29-33,35-38,41,44-45]。纳入患者4 153例,其中腰椎间盘置换术901例、椎间盘融合术762例、标准椎间盘切除术1 122例、椎间盘镜下髓核摘除术354例、显微镜下髓核摘除术260例、经皮内窥镜腰椎间盘切除术248例、经皮激光椎间盘减压术100例、化学溶核术337例及自动经皮腰椎间盘切除术69例。各手术方式结果比较部分差异有显著性意义,见表7,并发症发生率方面排序为经皮内窥镜腰椎间盘切除术>自动经皮腰椎间盘切除术>标准椎间盘切除术>显微镜下髓核摘除术>经皮激光椎间盘减压术>椎间盘镜下髓核摘除术>腰椎间盘置换术>腰椎间盘融合术>化学溶核术。 "
|
[1] 易军飞,陈通,刘友军.腰椎间盘突出手术治疗的进展[J].现代医学与健康研究电子杂志,2017,1(9):135-137.
[2] 冯帆,蔡毅,李颖波,等.腰椎间盘突出症7种手术修复方式差异的网络Meta分析[J].中国组织工程研究,2020,24(3):453-459.
[3] 刘国伟,于莉莉,贾洪霞,等.系统评价中的间接比较与网状Meta分析方法研究进展[J].中国循证医学杂志,2014,14(10):1276-1280.
[4] DELAMARTER RB, BAE HW, PRADHAN BB. Clinical results of ProDisc-II lumbar total disc replacement: Report from the United States clinical trial.Orthop Clin North Am.2005;36(3):301-313.
[5] SKÖLD C, TROPP H, BERG S. Five-year follow-up of total disc replacement compared to fusion: A randomized controlled trial.Eur Spine J.2013;22(10):2288-2295.
[6] RADCLIFF K, SPIVAK J, DARDEN B, et al. Five-Year Reoperation Rates of 2-Level Lumbar Total Disk Replacement Versus Fusion.Clin Spine Surg.2018;31(1):37-42.
[7] GORNET MF, BURKUS JK, DRYER RF, et al. Lumbar disc arthroplasty with MAVERICK disc versus stand-alone interbody fusion: A prospective, randomized, controlled, multicenter investigational device exemption trial.Spine.2011;36(25):E1600-E1611.
[8] GUYER RD, MCAFEE PC, BANCO RJ, et al.Prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of lumbar total disc replacement with the CHARITÉ artificial disc versus lumbar fusion: Five-year follow-up.Spine J. 2009;9(5):374-386.
[9] DELAMARTER R, ZIGLER JE, BALDERSTON RA, et al. Prospective, randomized, multicenter food and drug administration investigational device exemption study of the ProDisc-L total disc replacement compared with circumferential arthrodesis for the treatment of two-level lumbar degenerative disc disease: Results at twenty-four months.J Bone Joint Surg Am.2011;93(8):705-715.
[10] ZIGLER J, DELAMARTER R, SPIVAK JM, et al. Results of the prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of the ProDisc-L total disc replacement versus circumferential fusion for the treatment of 1-level degenerative disc disease.Spine.2007;32:1155-1162.
[11] WARDLAW D, RITHCHIE IK, SABBOUBEH AF, et al. Prospective randomized trial of chemonucleolysis compared with surgery for soft disc herniation with 1-year, intermediate, and long-term outcome: part I: the clinical outcome.Spine (Phila Pa 1976).2013;38(17):E1051-1057.
[12] REVEL M, PAYAN C, VALLEE C, et al.Automated percutaneous lumbar discectomy versus chemonucleolysis in the treatment of sciatica.A randomized multicenter trial.Spine (Phila Pa 1976).1993;18(1):1-7.
[13] DING ZM, TAO YQ. Clinical outcomes of percutaneous transforaminal endoscopic discectomy versus fenestration discectomy in patients with lumbar disc herniation. J Transl Med.2017;5(1):29-33.
[14] RIGHESSO O, FALAVIGNA A, AVANZI O. Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery. 2007;61(3):545-549; discussion 549.
[15] ABRISHAMKAR S, KOUCHAKZADEH M, MIRHOSSEINI A, et al. Comparison of open surgical discectomy versus plasma-laser nucleoplasty in patients with single lumbar disc herniation. J Res Med Sci.2015;20(12):1133-1137.
[16] KATAYAMA Y, MATSUYAMA Y, YOSHIHARA H, et al. Comparison of surgical outcomes between macro discectomy and micro discectomy for lumbar disc herniation: a prospective randomized study with surgery performed by the same spine surgeon.J Spinal Disord Tech. 2006;19(5):344-347.
[17] PAN Z, HA Y, YI S, et al. Efficacy of Transforaminal Endoscopic Spine System (TESSYS) Technique in Treating Lumbar Disc Herniation.Med Sci Monit.2016;22:530-539.
[18] THOMÉC, BARTH M, SCHARF J, et al. Outcome after lumbar sequestrectomy compared with microdiscectomy: a prospective randomized study.J Neurosurg Spine.2005;2(3):271-278.
[19] KONG L, SHANG XF, ZHANG WZ, et al. Percutaneous endoscopic lumbar discectomy and microsurgical laminotomy : a prospective, randomized controlled trial of patients with lumbar disc herniation and lateral recess stenosis.Orthopade.2019;48(2):157-164.
[20] BROUWER PA, BRAND R, VAN DEN AKKER-VAN MARLE ME, et al. Percutaneous laser disc decompression versus conventional microdiscectomy for patients with sciatica: Two-year results of a randomised controlled trial.Interv Neuroradiol.2017;23(3):313-324.
[21] CHEN Z, ZHANG L, DONG J, et al. Percutaneous transforaminal endoscopic discectomy compared with microendoscopic discectomy for lumbar disc herniation: 1-year results of an ongoing randomized controlled trial.J Neurosurg Spine.2018;28(3):300-310.
[22] CRISTANTE AF, ROCHA ID, MARTUSMARCON R, et al.Randomized clinical trial comparing lumbar percutaneous hydrodiscectomy with lumbar open microdiscectomy for the treatment of lumbar disc protrusions and herniations.Clinics(Sao Paulo).2016;71(5):276-280.
[23] YU D, WANG G, WEI Y, et al. The effect of posterior microendoscopy discectomy and open surgery on lumbar disc herniation.BIOMED RES-INDIA.2017;28(20):8874-8877.
[24] 钱久荣,华锦明,钱忠来,等.微创与椎板开窗技术治疗腰椎间盘突出症临床疗效比较[J].中国全科医学,2010,13(30):3431-3433.
[25] CRAWSHAW C, FRAZER AM, MERRIAM WF. A comparison of surgery and chemonucleolysis in the treatment of sciatica. A prospective randomized trial.Spine.1984;9(2):195-198.
[26] VAN ALPHEN HAM, BRAAKMAN R, BEZEMER PD, et al. Chemonucleolysis versus discectomy: a randomized multicenter trial.J Neurosurg.1989;70(6):869-875.
[27] STULA D. Chemonucleolysis with chymopapain in intervertebral disc hernia. A randomised comparative study of patients following surgery.Neurochirurgia(Stuttg).1990;33(5):169-172.
[28] LEE SH, CHUNG SE, AHN Y, et al. Comparative radiologic evaluation of percutaneous endoscopic lumbar discectomy and open microdiscectomy: A matched cohort analysis. Mt Sinai J Med. 2006; 73(5):795-801.
[29] PAN L. Comparison of tissue damages caused by endoscopic lumbar discectomy and traditional lumbar discectomy: a randomised controlled trial. Int J Surg.2014;12(5):534-537.
[30] TULLBERG T, ISACSON J, WEIDENHIELM L. Does microscopic removal of lumbar disc herniation lead to better results than the standard procedure? Results of a one-year randomized study.Spine. 1993;18(1):24-27.
[31] HUANG TJ, HSU RWW, LI YY, et al. Less systemic cytokine response in patients following microendoscopic versus open lumbar discectomy. J Orthop Res.2005;23(2):406-411.
[32] GARG B, NAGRAJA UB, JAYASWAL A. Microendoscopic versus open discectomy for lumbar disc herniation: a prospective randomised study. J Orthop Surg (Hong Kong).2011;19(1):30-34.
[33] MAYER HM, BROCK M. Percutaneous endoscopic discectomy: surgical technique and preliminary results compared to microsurgical discectomy.J Neurosurg.1993;78(2):216-225.
[34] CHATTERJEE S, FOY P, FINDLAY G.. Report of a Controlled Clinical Trial Comparing Automated Percutaneous Lumbar Discectomy and Microdiscectomy in the Treatment of Contained Lumbar Disc Herniation. Spine.1995;20(6):734-738.
[35] HUSSEIN M, ABDELDAYEM A, MATTAR MMM. Surgical technique and effectiveness of microendoscopic discectomy for large uncontained lumbar disc herniations: A prospective, randomized, controlled study with 8 years of follow-up.Eur Spine J.2014;23(9):1992-1999.
[36] VAN ALPHEN HA, BRAAKMAN R, BERFELO MW, et al. Chemonucleolysis or discectomy? Results of a randomized multicentre trial in patients with a herniated lumbar intervertebral disc (a preliminary report). Acta Neurochir Suppl(Wien). 1988;43:35-38.
[37] MURALIKUTTAN KP, HAMILTON A, KERNOHAN WG, et al. A prospective randomized trial of chemonucleolysis and conventional disc surgery in single level lumbar disc herniation.Spine (Phila Pa 1976).1992;17(4):381-387.
[38] 蒲小兵,周强,杨双石,等.MED与微创TLIF治疗伴Modic改变的腰椎间盘突出症的对比研究[J].中国骨科临床与基础研究杂志,2014,6(2):79-83.
[39] 温德勇.不同手术方式治疗腰椎间盘突出伴Modic改变的临床疗效研究[J].中国实用医药,2014,9(23):18-19.
[40] 马富海,吴小涛,洪鑫,等.不同术式治疗伴终板Modic改变的腰椎椎间盘突出症的疗效分析[J].脊柱外科杂志,2011,9(2):69-73.
[41] 贺宪,黄东生,梁安靖,等.椎体间融合术与单纯髓核摘除术治疗合并Modic Ⅱ型改变的单节段腰椎间盘突出症的疗效比较[J].中国脊柱脊髓杂志, 2014,24(11):1007-1012.
[42] 王灏.伴终板Modic改变腰椎间盘突出症术式选择及其对疗效的影响研究[J].长治医学院学报,2014,28(3):210-212.
[43] 杨耀琦,曹鹏,潘玉涛,等.伴终板改变的腰椎间盘突出症的手术方式选择[J].中华医学杂志,2009,89(27):1902-1906.
[44] DONG Z, DENG SC, YI M, et al. Surgical options and clinical outcomes in patients of lumbar disc herniation with Modic changes. Zhonghua yi xue za zhi.2013;93(39):3111-3115.
[45] ZHAO D, DENG SC, MA Y, et al. Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy.Eur Spine J.2010;19(3):443-450.
[46] 黄振强,罗玉琛.腰椎间盘突出与下腰痛的关系[J].海南医学,2003,14(8): 12-13.
[47] SHI R, WANG F, HONG X, et al. Comparison of percutaneous endoscopic lumbar discectomy versus microendoscopic discectomy for the treatment of lumbar disc herniation: a meta-analysis.Int Orthop. 2019;43(4):923-937.
[48] ZIGLER J, FERKO N, CAMERON C, et al. Comparison of therapies in lumbar degenerative disc disease: A network meta-analysis of randomized controlled trials.J Comp Eff Res.2018;7(3):233-246.
[49] JENNER JR, BUTTLE DJ, DIXON AK. Mechanism of action of intradiscal chymopapain in the treatment of sciatica: A clinical, biochemical, and radiological study.Ann Rheum Dis. 1986;45(6): 441-449. |
| [1] | Lü Zhen, Bai Jinzhu. A prospective study on the application of staged lumbar motion chain rehabilitation based on McKenzie’s technique after lumbar percutaneous transforaminal endoscopic discectomy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1398-1403. |
| [2] | Gao Yan, Zhao Licong, Zhao Hongzeng, Zhu Yuanyuan, Li Jie, Sang Deen. Alteration of low frequency fluctuation amplitude at brain-resting state in patients with chronic discogenic low back pain [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1160-1165. |
| [3] | Xie Zhifeng, Liu Qing, Liu Bing, Zhang Tao, Li Kun, Zhang Chunqiu, Sun Yanfang. Biomechanical characteristics of the lumbar disc after fatigue injury [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 339-343. |
| [4] | Xu Weilong, Zuo Yuan, Xin Daqi, He Chenyang, Zhao Peng, Shi Ming, Zhou Boyuan, Liu Yating, Zhao Yan. Selection of modeling methods for acute compressive spinal cord injury: a network Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(23): 3767-3772. |
| [5] | Zhong Yuanming, He Bingkun, Wu Zhuotan, Wu Sixian, Wan Tong, Zhong Xifeng. An exploration on the mechanism of Shaoyao Gancao Decoction in treating early pain of lumbar disc herniation based on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(20): 3194-3201. |
| [6] | Hou Yulong, Wang Jingshi, Wang Xukai. Potential mechanism of Achyranthes bidentata in the treatment of lumbar disc herniation based on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(17): 2734-2739. |
| [7] | Zhang Chongfeng, Li Xianlin, Peng Weibing, Jia Hongsheng, Cai Lei. Treating lumbar disc herniation of blood stasis type with Chinese herbs, acupuncture, moxibustion, and massage: a Bayesian network Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(17): 2781-2788. |
| [8] | Wu Zijian, Hu Zhaoduan, Zhou Xiaohong, Li Jia, Li Bocun, Cai Guowei, Peng Rui. Tongdu Huoxue Decoction-medicated serum inhibits pyroptosis in annulus fibrosus cells of the intervertebral disc [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(14): 2148-2153. |
| [9] | Qian Yuzhang, Wang Nan, Dong Yuqi, Xie Lin, Kang Ran. Factors for the recurrence of lumbar disc herniation after percutaneous transforaminal endoscopic discectomy: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(36): 5886-5896. |
| [10] |
Wang Qiuan, Yuan Feng, Wu Jibin, Sun Maji, Wu Dongying, Meng Qiang, Guo Kaijin.
Endoscopic unilateral versus bilateral decompression effects on lumbar disc herniation with contralateral symptoms [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(32): 5133-5137. |
| [11] | Feng Fan, Cai Yi, Li Yingbo, Dong Junli, Wu Qun, Fan Yongzhi, Yan Hong. Comparison of seven surgical interventions for lumbar disc herniation: a network meta-analysis#br# [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(3): 453-459. |
| [12] | Wang Wei, Xie Chengxin, Zhou Haonan, Zhang Yu, Wang Chenglong, Yin Dong. A meta-analysis of expandable intramedullary nail versus interlocking intramedullary nail for treatment of femoral shaft fracture [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(3): 477-484. |
| [13] | Wu Cai, Luo Tian, Zeng Qinghu, Peng Chengzhong, Liao Tao, Wang Lele, Zeng Zhao. Modified knee spreader combined with minimally invasive percutaneous plate internal fixation for complex tibial plateau fractures [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(27): 4305-4309. |
| [14] | Shi Yuling, Li Guangyao, Liang Zujian. Various acupuncture therapies for lateral epicondylitis: a Bayesian network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(23): 3756-3763. |
| [15] | Cen Zhuohao, Chen Jiena, Huang Jiahua, Shi Chushuo, Zhou Chi, Wen Junmao, Ling Min. Acupuncture combined with other therapies for osteoporosis: a network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(2): 320-328. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||