Chinese Journal of Tissue Engineering Research ›› 2020, Vol. 24 ›› Issue (9): 1353-1358.doi: 10.3969/j.issn.2095-4344.2215
Previous Articles Next Articles
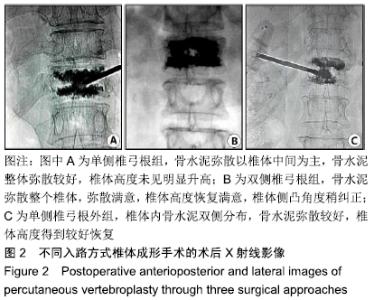
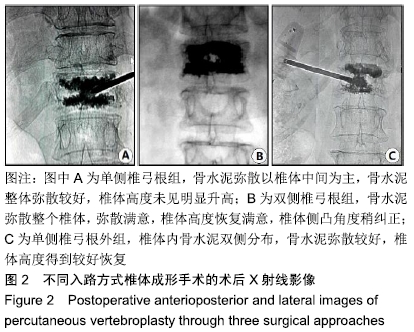
Percutaneous vertebroplasty through unilateral and bilateral pedicle approaches and unilateral pedicle extrapedicle approach for the treatment of thoracolumbar vertebral compression fractures: bone cement perfusion volume and cement leakage rate
Zhang Zhiwei, Li Li, Huang Ziyu, Wu Duoyi, Gan Farong, Ye Baofei, Zhang Yan, Zhang Taibiao, Hu Wanjun
- Department of Orthopedics, Hainan Provincial Hospital of Traditional Chinese Medicine, Haikou 570203, Hainan Province, China
-
Received:2019-05-27Revised:2019-05-29Accepted:2019-06-29Online:2020-03-28Published:2020-02-12 -
About author:Zhang Zhiwei, Master, Attending physician of traditional Chinese medicine, Department of Orthopedics, Hainan Provincial Hospital of Traditional Chinese Medicine, Haikou 570203, Hainan Province, China
CLC Number:
Cite this article
Zhang Zhiwei, Li Li, Huang Ziyu, Wu Duoyi, Gan Farong, Ye Baofei, Zhang Yan, Zhang Taibiao, Hu Wanjun. Percutaneous vertebroplasty through unilateral and bilateral pedicle approaches and unilateral pedicle extrapedicle approach for the treatment of thoracolumbar vertebral compression fractures: bone cement perfusion volume and cement leakage rate [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(9): 1353-1358.
share this article
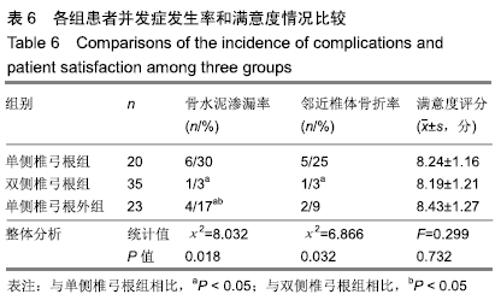
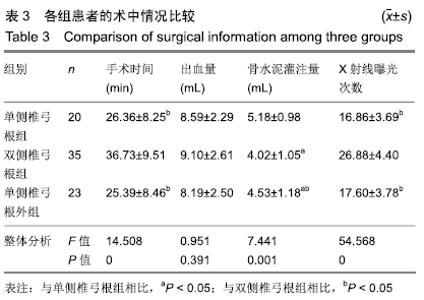
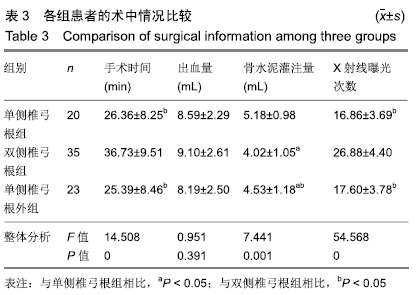
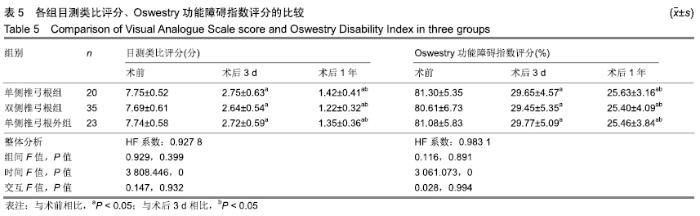
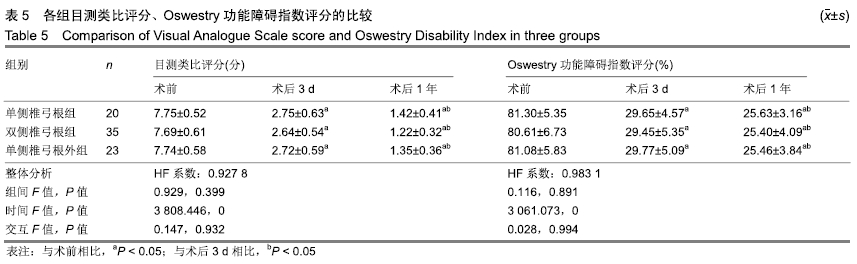
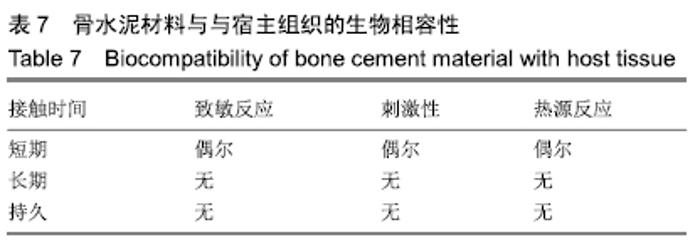
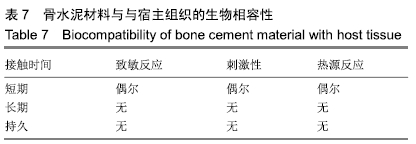
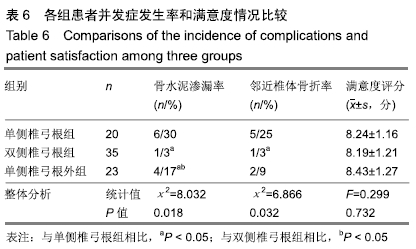
2.6 各组并发症发生情况及患者满意度 单侧椎弓根组发生并发症11例,6例骨水泥渗漏(2例椎旁软组织渗,3例穿刺针道渗漏,1例椎管内渗漏),随访1年中有5例发生邻近椎体骨折;双侧椎弓根组发生并发症2例,1例椎管内骨水泥渗漏,随访1年中有1例发生邻近椎体骨折;单侧椎弓根外组发生并发症6例,即4例骨水泥渗漏(2例椎旁软组织渗,1例穿刺针道渗漏,1例椎旁静脉丛渗漏),随访1年中有2例发生邻近椎体骨折。 单因素方差分析结果显示,3组术后骨水泥渗漏率、邻近椎体骨折发生率比较差异有显著性意义(P < 0.05),3组患者满意度评分比较差异均无显著性意义(P > 0.05);多重比较并结合主要数据分析显示,单侧椎弓根组、单侧椎弓根外组、双侧椎弓根组骨水泥渗漏率依次降低(P < 0.05);双侧椎弓根组邻近椎体骨折率低于单侧椎弓根组(P < 0.05),见表6。 "
| [1] ZHIYONG C, YUN T, HUI F, et al. Unilateral Versus Bilateral Balloon Kyphoplasty for Osteoporotic Vertebral Compression Fractures:A Systematic Review of Overlapping Meta-analyses.Pain Physician. 2019;22(1):15-28. [2] BOOTH A, HMA I, NORTHGRAVES M, et al. Effectiveness of surgical fixation for lateral compression type one (LC-1) fragility fractures of the pelvis: a systematic review.BMJ Open.2019;9(5): e024737. [3] WANG P, LI J, SONG Z, et al.Utilization of the directional balloon technique to improve the effectiveness of percutaneous kyphoplasty in the treatment of osteoporotic vertebral compression fractures and reduction of bone cement leakage. Medicine (Baltimore).2019;98(19):e15272. [4] TAN G, LI F, ZHOU D, et al.Unilateral versus bilateral percutaneous balloon kyphoplasty for osteoporotic vertebral compression fractures: A systematic review of overlapping meta-analyses. Medicine (Baltimore).2018;97(33):e11968. [5] ZHANG L, LI J, YANG H, et al. Histological evaluation of bone biopsy results during PVP or PKP of vertebral compression fractures.Oncol Lett.2013;5(1):135-138. [6] YANG S, CHEN C, WANG H, et al. A systematic review of unilateral versus bilateral percutaneous vertebroplasty/percutaneous kyphoplasty for osteoporotic vertebral compression fractures.Acta Orthop Traumatol Turc.2017;51(4):290-297. [7] VERONA M, MARONGIU G, CARDONI G, et al.Arthroscopically assisted reduction and internal fixation (ARIF) versus open reduction and internal fixation (ORIF) for lateral tibial plateau fractures: a comparative retrospective study.J Orthop Surg Res.2019;14(1):155. [8] TANNAST M, KEEL MJB, SIEBENROCK KA, et al.Open Reduction and Internal Fixation of Acetabular Fractures Using the Modified Stoppa Approach.JBJS Essent Surg Tech.2019;9(1):e3. [9] LIU L, CHENG S, WANG Q, et al.An anatomical study on lumbar arteries related to the extrapedicular approach applied during lumbar PVP (PKP).PLoS One.2019;14(3):e0213164. [10] YAO X, XU Z, DU X.PKP/PVP combine chemotherapy in the treatment of multiple myeloma patients with vertebral pathological fractures: minimum 3-year follow-up of 108 cases.J Orthop Surg Res. 2019;14(1):42. [11] 贾川,黎俊,赵洪,等.单侧经横突-椎弓根入路与双侧经椎弓根入路经皮椎体成形术治疗重度骨质疏松性椎体压缩性骨折合并脊柱侧弯的比较研究[J].中医正骨,2018,30(12):23-29. [12] 罗建军,王冰.经皮椎体成形术治疗老年骨质疏松性胸腰椎压缩骨折的效果评价[J].颈腰痛杂志, 2016,37(3):200-203. [13] ENDER SA, GRADL G, ENDER M, et al.Osseofix® system for percutaneous stabilization of osteoporotic and tumorous vertebral compression fractures-clinical and radiological results after 12 months.Rofo.2014;186(4):380-387. [14] CHIAROTTO A, MAXWELL LJ, OSTELO RW, et al.Measurement Properties of Visual Analogue Scale, Numeric Rating Scale, and Pain Severity Subscale of the Brief Pain Inventory in Patients With Low Back Pain: A Systematic Review.J Pain.2019;20(3):245-263. [15] RUIZ FK, BOHL DD, WEBB ML, et al.Oswestry Disability Index is a better indicator of lumbar motion than the Visual Analogue Scale. Spine J.2014;14(9):1860-1865. [16] 孙志峰,何斌,蒋建新.单侧与双侧PVP治疗骨质疏松性胸腰椎压缩骨折的比较[J].中国骨与关节损伤杂志,2018,33(7):722-723. [17] 张禄梅.对行经皮椎体成形术的老年胸腰椎压缩性骨折患者进行优质护理的效果观察[J].当代医药论丛,2016,14(11):60-61. [18] LIANG L, CHEN X, JIANG W, et al.Balloon kyphoplasty or percutaneous vertebroplasty for osteoporotic vertebral compression fracture? An updated systematic review and meta-analysis. Ann Saudi Med.2016;36(3):165-174. [19] 王开荣.经皮椎体成形术、经皮椎体后凸成形术治疗老年腰椎压缩性骨折的疗效比较[J].中国继续医学教育,2016,8(23): 110-111. [20] LUTHER E, URAKOV T, VANNI S.Percutaneous Instrumentation of a Complex Lumbar Spine Fracture with Bilateral Pedicle Dissociation: Case Report and Technical Note.J Neurol Surg A Cent Eur Neurosurg.2018;79(5):416-423. [21] 周瑞华,顾邦林,张亮,等.单侧PVP与双侧PVP治疗骨质疏松性胸腰椎骨折的近期疗效对比[J]. 实用临床医药杂志,2016,20(19):48-50,54. [22] 赵小龙.单侧椎弓根入路经皮椎体后凸成形术对骨质疏松性椎体压缩性骨折患者术后VAS评分及生活质量的影响[J].现代诊断与治疗, 2018,29(4):578-580. [23] 吴溢峰,钟姣红,吴焯鹏,等. 3种不同入路经皮椎体成形术治疗胸腰段椎体压缩性骨折的疗效比较[J]. 中国微创外科杂志,2018,18(7):611-615. [24] FOTI G, BELTRAMELLO A, CATANIA M, et al.Diagnostic accuracy of dual-energy CT and virtual non-calcium techniques to evaluate bone marrow edema in vertebral compression fractures.Radiol Med.2019;124(6):487-494. [25] LI YB, ZHENG X, WANG R, et al.SPECT-CT versus MRI in localizing active lesions in patients with osteoporotic vertebral compression fractures.Nucl Med Commun.2018;39(7):610-617. [26] CHENG J, MUHEREMU A, ZENG X, et al.Percutaneous vertebroplasty vs balloon kyphoplasty in the treatment of newly onset osteoporotic vertebral compression fractures: A retrospective cohort study. Medicine (Baltimore). 2019;98(10):e14793. [27] LIS E, LAUFER I, BARZILAI O, et al.Change in the cross- sectional area of the thecal sac following balloon kyphoplasty for pathological vertebral compression fractures prior to spine stereotactic radiosurgery.J Neurosurg Spine.2018;30(1):111-118. [28] ALPANTAKI K, DOHM M, KOROVESSIS P, et al.Surgical options for osteoporotic vertebral compression fractures complicated with spinal deformity and neurologic deficit.Injury.2018;49(2):261-271. [29] ZHU J, ZHANG K, LUO K, et al.Mineralized Collagen Modified Polymethyl Methacrylate Bone Cement for Osteoporotic Compression Vertebral Fracture at 1-Year Follow-up.Spine (Phila Pa 1976). 2019; 44(12):827-838. [30] 邵明星,王峰,石晶,等.马骨续筋胶囊结合经皮椎体成形术治疗老年骨质疏松性胸腰椎骨折的早期疗效分析[J].临床和实验医学杂志, 2016,15(9):894-896,897. [31] 王延涛,陈怡,潘美均,等.单侧与双侧椎弓根入路注入骨水泥治疗骨质疏松性椎体压缩骨折有效和安全性的Meta分析[J].中国组织工程研究,2019,23(10):1633-1640. [32] 李清.微创单侧入路双侧减压治疗退变性腰椎管狭窄症的疗效[J].中国药物与临床,2019,19(5):815-817. [33] RAPAN S, KRNIĆ K, Rapan V, et al.Application of high viscosity bone cement in vertebroplasty for treatment of painful vertebral body fracture[J]. Med Glas (Zenica), 2016,13(2):148-153. [34] 雷雷,郑瑞芝,王月霞,等.阿托伐他汀联合阿仑膦酸钠治疗老年性骨质疏松的临床疗效及安全性[J].中国骨质疏松杂志, 2016,22(8):1031-1034. [35] 胡永军,霍理,岑万春,等.经皮椎体成形术治疗骨质疏松性椎体压缩性骨折200例的疗效分析[J].重庆医学,2016,45(22):3052-3054. [36] GAO C, ZONG M, WANG WT, et al.Analysis of risk factors causing short-term cement leakages and long-term complications after percutaneous kyphoplasty for osteoporotic vertebral compression fractures.Acta Radiol.2018;59(5):577-585. [37] GUO Z, WANG W, GAO WS, et al.Comparison the clinical outcomes and complications of high-viscosity versus low-viscosity in osteoporotic vertebral compression fractures.Medicine (Baltimore).2017;96(48):e8936. [38] HARTMANN S, KAVAKEBI P, TSCHUGG A, et al.Navigation for Tubular Decompression of the L5 Nerve Root Ganglion after Cement Leakage via a Wiltse Approach.Asian J Neurosurg. 2019; 14(2):565-567. [39] SEOJB, HEO K, YANG JH, et al.Clinical outcomes of dual 3.5-mm locking compression plate fixation for humeral shaft fractures: Comparison with single 4.5-mm locking compression plate fixation.J Orthop Surg (Hong Kong).2019;27(2):2309499019839608. [40] HU KZ, CHEN SC, XU L.Comparison of percutaneous balloon dilation kyphoplasty and percutaneous vertebroplasty in treatment for thoracolumbar vertebral compression fractures.Eur Rev Med Pharmacol Sci.2018;22(1 Suppl):96-102. |
| [1] | Jing Wanli, Zhang Tao, Teng Donghui, Shi Tao, Zhou Qiang. Poor outcomes of bone filling mesh container vertebroplasty for the treatment of osteoporotic vertebral compression fractures with vertebral body wall incompetence [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(10): 1522-1527. |
| [2] | Wang Yiya, Zhang Han, Lan Hai. Digital evaluation of finite element model for percutaneous kyphoplasty with bone cement injection [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(9): 1378-1383. |
| [3] | Li Kaiming, Wang Shangquan, Li Linghui, Zhu Liguo, Zhang Qing, Xie Rui. Bone filling bag vertebroplasty and percutaneous kyphoplasty for the treatment of thoracolumbar osteoporotic compression fractures: a meta-analysis of improving Cobb angle and reducing bone cement leakage [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(4): 650-656. |
| [4] | Pang Jutao, Chen Hong, Liu Bin, Zhang Wei, Sun Jianhua, Zhou Lianjun, Zhang Xinhu. Lateral versus anterior open injectors in the percutaneous vertebroplasty treatment of osteoporotic vertebral compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(16): 2461-2466. |
| [5] | Ren Yide, Zhang Yafeng, Li Feng, Gao Hongwen. Relationship between unilateral percutaneous kyphoplasty for treating Kummell’s disease and the amount of injected bone cement [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(16): 2467-2472. |
| [6] | Jiang Wenkang, Geng Wei, Xu Yingying, Yang Xiaomei, Ren Hangling, Zhang Jingtao, Ma Jinzhu. Application of mineralized collagen modified bone cement in the treatment of osteoporotic vertebral compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(15): 2381-2386. |
| [7] | Wu Bin, Bai Fenghua, Lin Mingxia, Lin Jianping. Risk factors of adjacent vertebral collapse after kyphoplasty with cement injection in older adult women [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(12): 1829-1834. |
| [8] | Mo Ling, Liang De, Huang Jinjing, Jiang Xiaobing, Yang Zhidong, Ye Linqiang, Cui Jianchao, Zhang Shuncong, Yao Zhensong, Jin Daxiang. Classification and distribution of fracture areas in fresh osteoporotic vertebral compression fractures based on CT multi-planar reconstruction and MRI [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(11): 1647-1653. |
| [9] | Zhang Shuai, Wang Gaoju, Wang Qing. Relationship between thoracic and lumbar vertebral posterior wall morphology and bone cement leakage into the spinal canal during the percutaneous kyphoplasty [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(10): 1477-1483. |
| [10] | Li Shuyuan, Zhou Qishi, Li Yue, Lin Zhiyi, Zhou Hongliang, Shen Zhen, Hu Cheng, Yang Jiabao. Effects of changes in surface morphology of bone cement spacer on the expression of bone growth factor in induced membrane [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(10): 1502-1507. |
| [11] | Guo Dahua, Wang Yuhui, Ye Qianqu, Liu Wenhao, Yang Bo, Ye Linqiang. Mechanical changes of percutaneous kyphoplasty and percutaneous vertebroplasty in the treatment of thoracolumbar compressive fractures in three-dimensional vertebral models [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(32): 5146-5150. |
| [12] | He Jiangtao, Wang Sanmu, Li Zhongyi. Percutaneous vertebroplasty by bone cement perfusion using the unilateral transverse process-pedicle approach for treatment of thoracolumbar osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(22): 3604-3608. |
| [13] | Yuan Dechao, Wu Chao, Deng Jiayan, Tan Lun, Lin Xu, Wang Xiangyu . Bone cement distribution form and diffusion degree after percutaneous vertebroplasty: an analysis based on Mimics software and its clinical significance [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(10): 1507-1513. |
| [14] | Xu Yong, Guan Zhong, Li Yongxia, Chen Feng. A bone filling mesh container for treating senile osteoporotic vertebral compression fractures combined with intravertebral cleft sign [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(10): 1477-1482. |
| [15] | Wang Yantao, Chen Yi, Pan Meijun, Huang Jiahua, Chen Jinzhao, Liu Dejian, Xian Shuyi, Zhou Chi, Wang Haibin. Efficacy and safety of bone cement injection via unipedicular and bipedicular approaches in the treatment of osteoporotic vertebral compression fractures: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(10): 1633-1640. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||