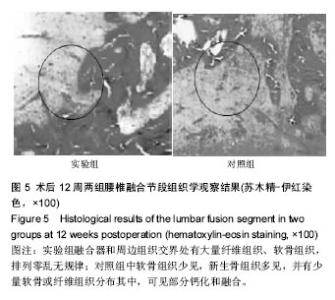
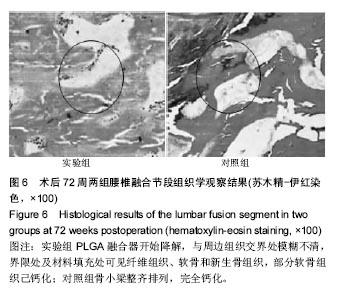
| [1]Barz T, Melloh M, Lord SJ,et al. A conceptual model of compensation/decompensation in lumbar segmental instability. Med Hypotheses. 2014;83(3):312-316.[2]费琦,赵凡,杨雍,等.腰椎后路融合手术对失稳模型节段稳定性及相邻节段力学的影响[J].中华医学杂志, 2015,95(45): 3681-3686.[3]Chen Y, Wang X, Chen D, et al. Posterior hybrid technique for ossification of the posterior longitudinal ligament associated with segmental instability in the cervical spine. J Spinal Disord Tech. 2014;27(4):240-244.[4]于文浩,王志强,李鑫平,等.经椎间孔腰椎融合术在腰椎翻修手术中应用的临床疗效[J].现代生物医学进展, 2015,15(24): 4690-4692,4667.[5]杨博,欧云生,蒋电明,等.纳米羟基磷灰石/聚酰胺66椎间融合器用于腰椎退行性疾病手术治疗的初期临床疗效[J].生物医学工程学杂志,2014,31(5):1102-1106.[6]姚豹,李开南,聂海,等.可生物降解聚乳酸-乙醇酸共聚物腰椎横突间融合器的体内生物力学[J].中国组织工程研究, 2014, 18(52):8426-8432.[7]宋成哲,金红旭.碳纤维椎间融合器与钛网椎间融合器修复腰椎退行性变:生物相容性比较[J].中国组织工程研究, 2015,19(12): 1909-1913.[8]李亮,江美林,赵敦旭.腰椎L4/5棘突间椎间融合器的生物力学特性及生物相容性[J].中国组织工程研究,2015,19(38): 6109-6113.[9]马龙冰,贾云兵,宋跃明,等.聚氨基酸/纳米羟基磷灰石/硫酸钙椎间融合器在腰椎融合术中的初步应用[J].中国修复重建外科杂志,2016,30(3):328-335.[10]Fu YC, Fu TF, Wang HJ, et al. Aspartic acid-based modified PLGA-PEG nanoparticles for bone targeting: in vitro and in vivo evaluation. Acta Biomater. 2014;10(11):4583-4596.[11]Byvaltsev VA, Kalinin AA, Belykh EG, et al. Optimization of segmental lumbar spine instability treatment using minimally invasive spinal fusion technique. Zh Vopr Neirokhir Im N N Burdenko. 2015;79(3):45-54.[12]Yoshiiwa T, Miyazaki M, Kawano M, et al. Analysis of the Relationship between Hypertrophy of the Ligamentum Flavum and Lumbar Segmental Motion with Aging Process. Asian Spine J. 2016;10(3):528-535.[13]牛伟民,于德水,李名武,等.椎体间纤维性融合重建兔脊柱稳定性的初步探索[J].中国脊柱脊髓杂志,2012,22(12):1108-1112.[14]Facchinello Y, Brailovski V, Petit Y, et al. Biomechanical assessment of the stabilization capacity of monolithic spinal rods with different flexural stiffness and anchoring arrangement. Clin Biomech (Bristol, Avon). 2015;30(10): 1026-1035.[15]嘉士健,黄翠华,雷行华,等.针刀配合脊椎平衡手法康复训练治疗下颈椎不稳症临床观察[J].中国中医急症,2015,24(10): 1829-1831.[16]魏建军,杨永江,颜世昌,等.“脊柱损伤控制”在不稳定性胸腰椎骨折的多发伤患者中的应用[J].检验医学与临床, 2015,12(z2): 136-138.[17]Fry RW, Alamin TF, Voronov LI, et al. Compressive preload reduces segmental flexion instability after progressive destabilization of the lumbar spine. Spine (Phila Pa 1976). 2014;39(2):E74-81.[18]何磊,戎利民,董健文,等.极外侧椎体间融合术治疗腰椎退行性疾病的近期疗效及安全性评价[J].中华骨科杂志, 2014,34(1): 48-55.[19]胡巍,陈水连,柯宝毅,等.后路钉棒系统在经寰枢椎椎弓根治疗可复性寰枢椎不稳定中的应用[J].中国现代医学杂志, 2014, 24(31): 103-106.[20]侯煜,田少辉,卜宏建,等.后正中入路Dynesys置入对腰椎全椎板减压术后生理性稳定性的作用[J].临床神经外科杂志, 2015,12(1):51-53,57.[21]魏富鑫,钟锐,潘希敏,等.腰椎融合/非融合技术治疗L4/5退变性疾病的疗效及对相邻节段退变的影响[J].中国脊柱脊髓杂志, 2014,24(10):892-899.[22]宗倩颖,叶霖,张爱英,等.聚醚醚酮及其复合材料在生物医用领域的应用[J].合成树脂及塑料,2016,33(3):93-96.[23]郝建学,周斐,钟娜,等.椎间植骨量对腰椎椎间融合内固定术后融合效果的研究[J].实用骨科杂志,2016,22(3):205-208,245.[24]Du BL, Zeng CG, Zhang W, et al. A comparative study of gelatin sponge scaffolds and PLGA scaffolds transplanted to completely transected spinal cord of rat. J Biomed Mater Res A. 2014;102(6):1715-1725.[25]Kim YC, Kim YH, Kim JW, et al. Transplantation of Mesenchymal Stem Cells for Acute Spinal Cord Injury in Rats: Comparative Study between Intralesional Injection and Scaffold Based Transplantation. J Korean Med Sci. 2016; 31(9):1373-1382.[26]Zhang Y, Mao H, Gao C, et al. Designed Stem Cell Aggregates: Enhanced Biological Functions of Human Mesenchymal Stem-Cell Aggregates Incorporating E-Cadherin-Modified PLGA Microparticles (Adv. Healthcare Mater. 15/2016). Adv Healthc Mater. 2016;5(15):1992.[27]赵金柱,袁伟,徐卫东.脊柱关节炎动物模型的研究现状[J].中华骨与关节外科杂志,2015,8(2):173-176.[28]钟锐,刘少喻.腰椎间盘退变动物模型构建的研究进展[J].中华实验外科杂志,2015,32(7):1760-1762.[29]任磊,沈生军,高德东,等.基于有限元的椎弓根螺钉结合两种材质椎间融合器治疗腰椎滑脱症的生物力学特性研究[J].中国现代医学杂志,2015,25(33):27-31.[30]汤嘉军,杨宇超,陈国荣,等.一种兔腰椎间融合模型的建立及效果评价[J].中国临床解剖学杂志,2015,33(3):325-330.[31]Lee S, Zhang X, Shen J, et al. Brief Report: Human Perivascular Stem Cells and Nel-Like Protein-1 Synergistically Enhance Spinal Fusion in Osteoporotic Rats. Stem Cells. 2015;33(10):3158-3163.[32]Chen L, Liu HL, Gu Y, et al. Lumbar interbody fusion with porous biphasic calcium phosphate enhanced by recombinant bone morphogenetic protein-2/silk fibroin sustained-released microsphere: an experimental study on sheep model. J Mater Sci Mater Med. 2015;26(3):126.[33]杨泽雨,杨欣建,陈扬,等.新型3D打印多孔钛人工椎体在猪脊柱模型置换前后的生物力学测试研究[J].生物骨科材料与临床研究,2016,13(1):7-9.[34]Solano MA, Fitzpatrick N, Bertran J. Cervical Distraction-Stabilization Using an Intervertebral Spacer Screw and String-of Pearl (SOP™) Plates in 16 Dogs With Disc-Associated Wobbler Syndrome.Vet Surg. 2015l;44(5): 627-641.[35]Anasetti F, Galbusera F, Aziz HN, et al. Spine stability after implantation of an interspinous device: an in vitro and finite element biomechanical study. J Neurosurg Spine. 2010;13(5): 568-575.[36]张春霖,王若愚,李莹,等.腰椎失稳症患者腰椎间隙X线解剖分型及其临床意义[J].中华解剖与临床杂志,2015,20(6):488-493.[37]张海龙,贺石生,顾广飞,等.通道辅助下多节段腰椎管狭窄症的微创治疗[J].中国微创外科杂志,2014,14(3):238-242.[38]杨洋,黎庆初,朱召银,等.双节段前路颈椎自锁式融合器融合术后矢状位影像学参数的变化[J].中国脊柱脊髓杂志,2016,26(2): 116-123.[39]谭海涛,孟志斌,黄涛,等.三点稳定式脊柱融合技术效果的动物实验研究[J].临床医学工程,2014,21(3):278-280.[40]曹师锋,谢宁,王登山,等.富血小板血浆促纤维多孔钛颈椎椎间融合器中骨长入作用[J].脊柱外科杂志,2016,14(2):96-100. |