Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (9): 1450-1455.doi: 10.3969/j.issn.2095-4344.2017.09.025
Previous Articles Next Articles
Allogeneic hematopoietic stem cell transplantation for intermediate cytogenetic risk acute myeloid leukemia
Zhang Wen-hui1, Chi Kai-kai2, Chen Yu-qing1, Yang Jing1, Zhu Zun-min1, Sun Kai1, Zhang Yin1
- 1Henan Provincial People’s Hospital, Zhengzhou 450002, Henan Province, China; 2Department of Kidney Transplantation, First Affiliated Hospital of Henan University of TCM, Zhengzhou 450000, Henan Province, China
-
Online:2017-03-28Published:2017-03-31 -
Contact:Chen Yu-qing, Master, Chief physician, Henan Provincial People’s Hospital, Zhengzhou 450002, Henan Province, China -
About author:Zhang Wen-hui, Master, Attending physician, Henan Provincial People’s Hospital, Zhengzhou 450002, Henan Province, China -
Supported by:the National Natural Science Foundation of China, No. 81273259
CLC Number:
Cite this article
Zhang Wen-hui, Chi Kai-kai, Chen Yu-qing, Yang Jing, Zhu Zun-min, Sun Kai, Zhang Yin . Allogeneic hematopoietic stem cell transplantation for intermediate cytogenetic risk acute myeloid leukemia[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(9): 1450-1455.
share this article
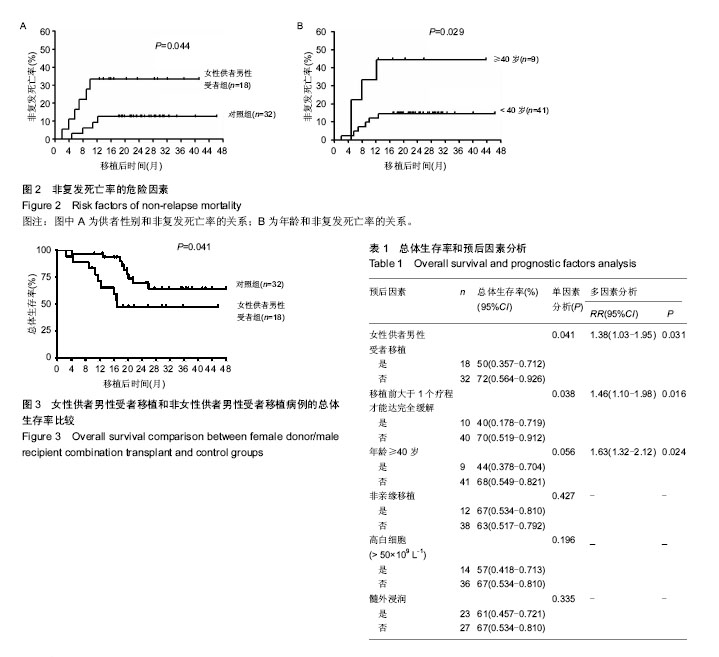
2.2 造血重建 50例患者均获得造血重建。中性粒细胞重建时间为13(10-25) d,血小板重建时间为14(9-40) d。移植后30-40 d进行植活证据指标检测提示异体造血干细胞在受者体内完全植活。 2.3 移植物抗宿主病发生率 13例(26%)患者移植后出现急性移植物抗宿主病,其中4例(8%)患者发生重度急性移植物抗宿主病;21例(42%)患者发生慢性移植物抗宿主病。 2.4 移植后复发、移植相关死亡、生存率及死亡原因 50例移植患者中共有9例(18%)复发,其中骨髓复发8例,髓外复发1例,中位复发时间为12(2-40)个月,随访期末,只有1例骨髓复发患者带病存活,复发死亡8例。 50例移植患者中共10例(20%)死于非白血病复发移植相关并发症,其中包括急性移植物抗宿主病2例、巨细胞病毒感染1例、出血性膀胱炎2例、肺部真菌感染2例、移植物抗宿主病相关性间质性肺炎1例、卡氏肺孢子虫肺炎1例、急性呼吸窘迫综合征1例。 随访期末,共有32例患者存活,4年总体生存率为64%。对移植相关非复发死亡率危险因素的分析发现,女性供者男性受者配对患者移植相关非复发死亡率明显高于非女性供者男性受者配对患者(分别为33%和12%,P=0.044)、年龄≥40岁的患者移植相关非复发死亡率明显高于年龄< 40岁的患者(分别为44%和15%,P=0.029),见图2。未发现非亲缘移植、移植前大于1个疗程才能达完全缓解、高白细胞(诊断时白细计数> 50×109 L-1)和髓外浸润与移植相关非复发死亡率相关(P均> 0.05)。作者又进一步分析了与复发相关的危险因素,未发现上述因素与疾病复发率的相关性(P均> 0.05)。 2.5 预后因素分析 作者分析了与移植预后相关的危险因素,包括年龄≥40岁,女性供者男性受者配对移植、非亲缘移植、移植前大于1个疗程才能达完全缓解、高白细胞和髓外浸润。单因素分析发现,女性供者男性受者配对移植、移植前大于1个疗程才能达完全缓解、年龄≥40岁是预后不良的危险因素。女性供者男性受者配对移植病例(n=18)和非女性供者男性受者配对移植病例(n=32),4年总体生存率分别为50%和72%(P=0.041,图3)。移植前大于1个疗程才能达完全缓解的病例(n=10)和1个疗程达到完全缓解的病例(n=40),4年总体生存率分别为40%和70%(P=0.038)。年龄≥40岁的病例(n=9)和年龄< 40岁的病例(n=41),4年总体生存率分别为44%和68%(P=0.056)。非亲缘移植、高白细胞和髓外浸润对总体生存率的影响差异无显著性意义(P均> 0.1,表1)。 将单因素分析中P < 0.10的预后危险因素纳入了多因素分析。结果显示女性供者男性受者配对移植、移植前大于1个疗程才能达完全缓解、年龄≥40岁均为预后不良的独立危险因素,其相对危险度(RR)分别为1.52(95%CI 1.03-1.95,P=0.031)、1.91(95%CI 1.36-2.41,P=0.016)及1.63(95%CI 1.17-2.06,P=0.024),见表1。"
| [1] Cornelissen JJ, van Putten WL, Verdonck LF, et al. Results of a HOVON/SAKK donor versus no-donor analysis of myeloablative HLA-identical sibling stem cell transplantation in first remission acute myeloid leukemia in young and middle-aged adults: benefits for whom. Blood. 2007;109(9): 3658-3666.[2] Koreth J, Schlenk R, Kopecky KJ, et al. Allogeneic stem cell transplantation for acute myeloid leukemia in first complete remission: systematic review and meta-analysis of prospective clinical trials. JAMA. 2009;301(22):2349-2361.[3] Gupta T, Kannan S, Dantkale V, et al. Cyclophosphamide plus total body irradiation compared with busulfan plus cyclophosphamide as a conditioning regimen prior to hematopoietic stem cell transplantation in patients with leukemia: a systematic review and meta-analysis. Hematol Oncol Stem Cell Ther. 2011;4(1):17-29.[4] Glucksberg H, Storb R, Fefer A, et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation. 1974; 18(4):295-304.[5] Lanino E, Rondelli R, Locatelli F, et al. Early (day -7) versus conventional (day -1) inception of cyclosporine-A for graft-versus-host disease prophylaxis after unrelated donor hematopoietic stem cell transplantation in children. Long-term results of an AIEOP prospective, randomized study. Biol Blood Marrow Transplant. 2009;15(6):741-748.[6] Bautista F, Moreno L, Fernández-Navarro JM, et al. Evaluation of chimerism by quantitative PCR analysis of DNA polymorphism after allogeneic hematopoietic stem cell transplantation in a pediatric population with malignancies. Pediatr Transplant. 2011;15(1):81-87.[7] Grimwade D, Walker H, Oliver F, et al. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children's Leukaemia Working Parties. Blood. 1998;92(7):2322-2333.[8] Ringdén O, Pavletic SZ, Anasetti C, et al. The graft-versus-leukemia effect using matched unrelated donors is not superior to HLA-identical siblings for hematopoietic stem cell transplantation. Blood. 2009;113(13):3110-3118.[9] Döhner H, Estey EH, Amadori S, et al. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood. 2010;115(3):453-474.[10] Suciu S, Mandelli F, de Witte T, et al. Allogeneic compared with autologous stem cell transplantation in the treatment of patients younger than 46 years with acute myeloid leukemia (AML) in first complete remission (CR1): an intention-to-treat analysis of the EORTC/GIMEMAAML-10 trial. Blood. 2003; 102(4):1232-1240.[11] Imahashi N, Suzuki R, Fukuda T, et al. Allogeneic hematopoietic stem cell transplantation for intermediate cytogenetic risk AML in first CR. Bone Marrow Transplant. 2013n;48(1):56-62.[12] Lee SJ, Klein J, Haagenson M, et al. High-resolution donor-recipient HLA matching contributes to the success of unrelated donor marrow transplantation. Blood. 2007;110(13): 4576-4583.[13] Randolph SS, Gooley TA, Warren EH, et al. Female donors contribute to a selective graft-versus-leukemia effect in male recipients of HLA-matched, related hematopoietic stem cell transplants. Blood. 2004;103(1):347-352.[14] Moore J, Nivison-Smith I, Goh K, et al. Equivalent survival for sibling and unrelated donor allogeneic stem cell transplantation for acute myelogenous leukemia.Biol Blood Marrow Transplant. 2007;13(5):601-607.[15] Cho BS, Kim JH, Yoon JH, et al. Superior transplantation outcomes of 8/8-matched unrelated donors as well as matched siblings to autologous transplantation for acute myeloid leukemia with intermediate cytogenetics in first remission. Eur J Haematol. 2013;90(5):365-374.[16] Hsieh YY, Hong YC, Hsiao LT, et al. Effect of allogeneic hematopoietic stem cell transplantation from matched siblings or unrelated donors during the first complete remission in patients with cytogenetically normal acute myeloid leukemia. Eur J Haematol. 2011;86(3):237-245.[17] Koreth J, Schlenk R, Kopecky KJ, et al. Allogeneic stem cell transplantation for acute myeloid leukemia in first complete remission: systematic review and meta-analysis of prospective clinical trials. JAMA. 2009;301(22):2349-2361.[18] Spierings E, Kim YH, Hendriks M, et al. Multicenter analyses demonstrate significant clinical effects of minor histocompatibility antigens on GvHD and GvL after HLA-matched related and unrelated hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2013;19(8):1244-1253.[19] Li S, Kawata H, Katsuyama Y, et al. Association of polymorphic MHC microsatellites with GVHD, survival, and leukemia relapse in unrelated hematopoietic stem cell transplant donor/recipient pairs matched at five HLA loci. Tissue Antigens. 2004;63(4):362-368.[20] Ayuk F, Diyachenko G, Zabelina T, et al. Anti-thymocyte globulin overcomes the negative impact of HLA mismatching in transplantation from unrelated donors. Exp Hematol. 2008; 36(8):1047-1054.[21] Gahrton G. Risk assessment in haematopoietic stem cell transplantation: impact of donor-recipient sex combination in allogeneic transplantation. Best Pract Res Clin Haematol. 2007;20(2):219-229.[22] Martin PJ. Increased disparity for minor histocompatibility antigens as a potential cause of increased GVHD risk in marrow transplantation from unrelated donors compared with related donors. Bone Marrow Transplant. 1991;8(3):217-223.[23] Kollman C, Spellman SR, Zhang MJ, et al. The effect of donor characteristics on survival after unrelated donor transplantation for hematologic malignancy. Blood. 2016;127(2):260-267.[24] Kongtim P, Di Stasi A, Rondon G, et al. Can a female donor for a male recipient decrease the relapse rate for patients with acute myeloid leukemia treated with allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2015; 21(4):713-719.[25] Gao L, Wen Q, Chen X, et al. Effects of priming with recombinant human granulocyte colony-stimulating factor on conditioning regimen for high-risk acute myeloid leukemia patients undergoing human leukocyte antigen-haploidentical hematopoietic stem cell transplantation: a multicenter randomized controlled study in southwest China. Biol Blood Marrow Transplant. 2014;20(12):1932-1939.[26] Bejanyan N, Weisdorf DJ, Logan BR, et al. Survival of patients with acute myeloid leukemia relapsing after allogeneic hematopoietic cell transplantation: a center for international blood and marrow transplant research study. Biol Blood Marrow Transplant. 2015;21(3):454-459.[27] Stern M, Brand R, de Witte T, et al. Female-versus-male alloreactivity as a model for minor histocompatibility antigens in hematopoietic stem cell transplantation. Am J Transplant. 2008;8(10):2149-2157.[28] Nannya Y, Kataoka K, Hangaishi A, et al. The negative impact of female donor/male recipient combination in allogeneic hematopoietic stem cell transplantation depends on disease risk. Transpl Int. 2011;24(5):469-476.[29] Kurosawa S, Yamaguchi T, Uchida N, et al. Comparison of allogeneic hematopoietic cell transplantation and chemotherapy in elderly patients with non-M3 acute myelogenous leukemia in first complete remission. Biol Blood Marrow Transplant. 2011;17(3):401-411.[30] de Lima M, Couriel D, Thall PF, et al. Once-daily intravenous busulfan and fludarabine: clinical and pharmacokinetic results of a myeloablative, reduced-toxicity conditioning regimen for allogeneic stem cell transplantation in AML and MDS. Blood. 2004;104(3):857-864. |
| [1] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [2] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [3] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [4] | He Yunying, Li Lingjie, Zhang Shuqi, Li Yuzhou, Yang Sheng, Ji Ping. Method of constructing cell spheroids based on agarose and polyacrylic molds [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 553-559. |
| [5] | He Guanyu, Xu Baoshan, Du Lilong, Zhang Tongxing, Huo Zhenxin, Shen Li. Biomimetic orientated microchannel annulus fibrosus scaffold constructed by silk fibroin [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 560-566. |
| [6] | Chen Xiaoxu, Luo Yaxin, Bi Haoran, Yang Kun. Preparation and application of acellular scaffold in tissue engineering and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 591-596. |
| [7] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [8] | Shen Jiahua, Fu Yong. Application of graphene-based nanomaterials in stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 604-609. |
| [9] | Zhang Tong, Cai Jinchi, Yuan Zhifa, Zhao Haiyan, Han Xingwen, Wang Wenji. Hyaluronic acid-based composite hydrogel in cartilage injury caused by osteoarthritis: application and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 617-625. |
| [10] | Li Hui, Chen Lianglong. Application and characteristics of bone graft materials in the treatment of spinal tuberculosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 626-630. |
| [11] | Gao Cangjian, Yang Zhen, Liu Shuyun, Li Hao, Fu Liwei, Zhao Tianyuan, Chen Wei, Liao Zhiyao, Li Pinxue, Sui Xiang, Guo Quanyi. Electrospinning for rotator cuff repair [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 637-642. |
| [12] | Guan Jian, Jia Yanfei, Zhang Baoxin , Zhao Guozhong. Application of 4D bioprinting in tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 446-455. |
| [13] | Liu Jiali, Suo Hairui, Yang Han, Wang Ling, Xu Mingen. Influence of lay-down angles on mechanical properties of three-dimensional printed polycaprolactone scaffolds [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2612-2617. |
| [14] | Huang Bo, Chen Mingxue, Peng Liqing, Luo Xujiang, Li Huo, Wang Hao, Tian Qinyu, Lu Xiaobo, Liu Shuyun, Guo Quanyi . Fabrication and biocompatibility of injectable gelatin-methacryloyl/cartilage-derived matrix particles composite hydrogel scaffold [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2600-2606. |
| [15] | Fang Xiaoyang, Tang Tian, Wang Nan, Qian Yuzhang, Xie Lin. Repair and regenerative therapies of the annulus fibrosus [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(10): 1582-1587. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||