Chinese Journal of Tissue Engineering Research ›› 2015, Vol. 19 ›› Issue (51): 8247-8252.doi: 10.3969/j.issn.2095-4344.2015.51.009
Previous Articles Next Articles
Autologous chondrocyte transplantation for knee joint cartilage repair: MRI assessment of biomechanical changes
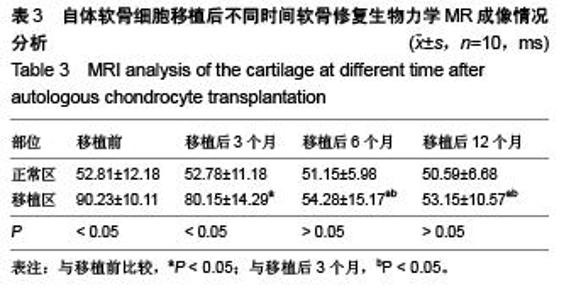
Guo Hong-bin1, Guo Ying-xin2, Yu Wei1, Ding Chun-ping3, Cai Li-zhong4, Li Min-yang5
- 1Department of Radiology, First Affiliated Hospital of Nanyang Medical College, Nanyang 473000, Henan Province, China; 2Department of Neurology, People’s Hospital of Sheqi County, Nanyang 473000, Henan Province, China; 3Department of Orthopedics, Third Affiliated Hospital of Nanyang Medical College, Nanyang 473000, Henan Province, China; 4Department of Thoracic Surgery, First Affiliated Hospital of Nanyang Medical College, Nanyang 473000, Henan Province, China; 5Department of Orthopedics, First Affiliated Hospital of Zhengzhou University, Zhengzhou 450001, Henan Province, China
-
Online:2015-12-10Published:2015-12-10 -
Contact:Li Min-yang, Associate chief physician, Associate professor, Department of Orthopedics, First Affiliated Hospital of Zhengzhou University, Zhengzhou 450001, Henan Province, China -
About author:Guo Hong-bin, Associate chief physician, Department of Radiology, First Affiliated Hospital of Nanyang Medical College, Nanyang 473000, Henan Province, China
CLC Number:
Cite this article
Guo Hong-bin, Guo Ying-xin, Yu Wei, Ding Chun-ping, Cai Li-zhong, Li Min-yang. Autologous chondrocyte transplantation for knee joint cartilage repair: MRI assessment of biomechanical changes[J]. Chinese Journal of Tissue Engineering Research, 2015, 19(51): 8247-8252.
share this article
| [1] 陈敏,徐贤,韩邵军,等.磁共振T2mapping成像对移植软骨的评估价值[J].中国医学科学院学报,2014,36(1):86-91.
[2] 张君,徐贤,李雪,等.基质诱导的自体软骨移植术后3T磁共振T2 mapping成像对移植软骨的分层定量评价[J].南方医科大学学报, 2015,35(1):141-145.
[3] Scheibel M, Bartl C, Magosch P, et al.Osteochondral autologous transplantation for the treatment of full-thickness cartilage defects of the shoulder: results at nine years. J Bone Joint Surg Br.2004;86(7):991-997.
[4] 张仲文,侯世科,杨造成,等.基质诱导的自体软骨细胞移植术修复膝关节软骨缺损10例术后2年的随访[J].中华关节外科杂志:电子版,2010,4(6):734-741.
[5] 李敏,刘阳,梁朝阳,等.延迟增强MRI评估基质诱导自体膝关节软骨移植术效果[J].中国医学影像学杂志,2014,22(5): 340-345, 349.
[6] 邓霞.关节软骨修复的3.0T磁共振成像研究[D].上海交通大学,2008.
[7] 陈加荣.组织工程关节软骨再生修复的在体无创监测方法研究[D].第三军医大学,2013.
[8] 钟心,张仲文,王宏,等.MRI随访观察膝关节基质诱导的自体软骨细胞移植术后2年[J].中国医学影像技术,2012,28(6): 1199-1203.
[9] Gudas R,Simonaityte R,Cekanauskas E,et al.A prospective, randomized clinical study of osteochondral autologous transplantation versus microfracture for the treatment of osteochondritis dissecans in the knee joint in children. J Pediatr Orthop.2009;29(7):741-748.
[10] 徐广春,程立明.软骨延迟增强磁共振成像在关节疾病中的应用[J].中国矫形外科杂志,2014,22(21):1974-1977.
[11] 朱国华.新鲜同种异体骨软骨移植并生长因子修复软骨缺损的实验研究[D].东南大学,2004.
[12] 崔延安,刘钊,刘红霞,等.骨髓间充质干细胞移植膝类风湿关节炎兔:关节滑膜体积和软骨厚度的MRI评价[J].中国组织工程研究与临床康复,2011,15(6):1024-1029.
[13] 杨小红,陈鸿辉,廖鹰扬,等.Ⅱ型胶原海绵修复兔膝关节软骨缺损的MRI与组织学对比分析[J].中华创伤杂志,2011,27(9): 827-833.
[14] 陈佳,王君瑞,施培华,等.MRI 在膝关节自体软骨细胞移植术后的评估价值[J].浙江医学,2012,37(15):1261-1263.
[15] 李忠.可注射性壳聚糖/磷酸甘油复合间充质干细胞修复猪关节软骨缺损的可行性研究[D].第三军医大学,2007.
[16] 宋玲玲.MR软骨生理成像技术在膝关节的临床应用研究[D].中山大学,2009.
[17] 金旭红.磁标记骨髓间充质干细胞构建组织工程软骨MRI活体示踪技术研究[D].第三军医大学,2008.
[18] Pinker K,Szomolanyi P,Welsch GC, et al.Longitudinal evaluation of cartilage composition of matrix-associated autologous chondrocyte transplants with 3-T delayed gadolinium-enhanced MRI of cartilage.AJR Am J Roentgenol. 2008;191(5):1391-1396.
[19] Gudas R,Kalesinskas RJ,Kimtys V, et al.A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy. 2005;21(9):1066-1075.
[20] Carey RE, Zheng L, Aiyangar AK, et al.Subject-Specific Finite Element Modeling of the Tibiofemoral Joint Based on CT, Magnetic Resonance Imaging and Dynamic Stereo-Radiography Data in Vivo.J Biomech Eng. 2014; 136(4).10.1115/1.4026228.
[21] Apprich S, Trattnig S, Welsch GH, et al.Assessment of articular cartilage repair tissue after matrix-associated autologous chondrocyte transplantation or the microfracture technique in the ankle joint using diffusion-weighted imaging at 3 Tesla. Osteoarthritis Cartilage.2012;20(7):703-711.
[22] 朱国华,王建伟,田小武,等.骨软骨移植联合rhBMP -2/bFGF修复软骨缺损[J].中国矫形外科杂志,2011,19(21):1815-1819.
[23] 孙英彩,崔建岭.MRI显示关节软骨研究进展[J].河北医科大学学报,2003,24(4):251-253.
[24] 王旭东,杨驰,范新东,等.自体耳廓软骨瓣置换或重建颞下颌关节盘MRI评价[J].口腔颌面外科杂志,2000,10(3):195-197.
[25] 李祥全,宋科荣,王黎明,等.膝关节软骨缺损的治疗现状及研究进展[J].中国骨伤,2015,28(5):482-486.
[26] Quirbach S,Trattnig S,Marlovits S, et al.Initial results of in vivo high-resolution morphological and biochemical cartilage imaging of patients after matrix-associated autologous chondrocyte transplantation (MACT) of the ankle.Skeletal radiology.2009;38(8):751-760.
[27] 王志学.自体软骨细胞膜片移植技术治疗膝关节软骨缺损术后早期随访分析[D].大连医科大学,2014.
[28] 张仲文,David Wood,钟心,等.对修复人膝关节软骨损伤的疗效研究[C].2014:158-168.
[29] Gudas R, Gudaite A, Pocius A, et al.Ten-year follow-up of a prospective, randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint of athletes. Am J Sports Med.2012; 40(11):2499-2508.
[30] 朱如里,郑闽前,马永平,等.自体软骨细胞移植修复关节软骨缺损的基础及临床应用研究[J].南通大学学报:医学版,2012, 32(6):458-460.
[31] 陈敏.磁共振成像对膝关节移植软骨生物力学指标的前瞻性研究[D].中国人民解放军医学院,2014.
[32] Welsch GH,Zak L,Mamisch TC, et al.Three-dimensional magnetic resonance observation of cartilage repair tissue (MOCART) score assessed with an isotropic three-dimensional true fast imaging with steady-state precession sequence at 3.0 Tesla.Investigative radiology.2009;44(9):603-612.
[33] Brown DS, Durkan MG, Foss EW,et al.Temporal in vivo assessment of fresh osteochondral allograft transplants to the distal aspect of the femur by dGEMRIC (delayed gadolinium-enhanced MRI of cartilage) and zonal T2 mapping MRI.J Bone Joint Surg Am. 2014;96(7):564-572.
[34] 陈淑莹,齐伟力.磁共振成像评估软骨移植修复术疗效研究进展[J].广东医学,2010,31(2):254-257.
[35] 谭勇海,姜苗苗,于海勇,等.关节镜清理联合自体骨髓间充质干细胞移植治疗膝骨关节炎的疗效观察[J].中医正骨, 2013, 25(10):35-38.
[36] 张德洲,罗飞,谈伟,等.低场MRI在膝关节损伤微创术后评估中的应用[J].四川医学,2015,(2):226-227.
[37] 周洁,梁治平.骨髓间充质干细胞修复关节软骨损伤的MRI示踪研究进展[J].实用放射学杂志,2012,28(2):300-303.
[38] 李俊峰,王峻.关节软骨磁共振成像研究进展及临床应用[J].山西医药杂志,2004,33(11):951-954.
[39] 张明彦.踝关节三维有限元模型的建立及三角韧带损伤和重建的踝关节生物力学有限元分析[D].中南大学,2012.
[40] Marlovits S, Singer P, Zeller P,et al.Magnetic resonance observation of cartilage repair tissue (MOCART) for the evaluation of autologous chondrocyte transplantation: determination of interobserver variability and correlation to clinical outcome after 2 years.Eur J Radiol.2006;57(1): 16-23.
|
| [1] | Chen Ziyang, Pu Rui, Deng Shuang, Yuan Lingyan. Regulatory effect of exosomes on exercise-mediated insulin resistance diseases [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 4089-4094. |
| [2] | Chen Yang, Huang Denggao, Gao Yuanhui, Wang Shunlan, Cao Hui, Zheng Linlin, He Haowei, Luo Siqin, Xiao Jingchuan, Zhang Yingai, Zhang Shufang. Low-intensity pulsed ultrasound promotes the proliferation and adhesion of human adipose-derived mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3949-3955. |
| [3] | Yang Junhui, Luo Jinli, Yuan Xiaoping. Effects of human growth hormone on proliferation and osteogenic differentiation of human periodontal ligament stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3956-3961. |
| [4] | Sun Jianwei, Yang Xinming, Zhang Ying. Effect of montelukast combined with bone marrow mesenchymal stem cell transplantation on spinal cord injury in rat models [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3962-3969. |
| [5] | Gao Shan, Huang Dongjing, Hong Haiman, Jia Jingqiao, Meng Fei. Comparison on the curative effect of human placenta-derived mesenchymal stem cells and induced islet-like cells in gestational diabetes mellitus rats [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3981-3987. |
| [6] | Hao Xiaona, Zhang Yingjie, Li Yuyun, Xu Tao. Bone marrow mesenchymal stem cells overexpressing prolyl oligopeptidase on the repair of liver fibrosis in rat models [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3988-3993. |
| [7] | Liu Jianyou, Jia Zhongwei, Niu Jiawei, Cao Xinjie, Zhang Dong, Wei Jie. A new method for measuring the anteversion angle of the femoral neck by constructing the three-dimensional digital model of the femur [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3779-3783. |
| [8] | Meng Lingjie, Qian Hui, Sheng Xiaolei, Lu Jianfeng, Huang Jianping, Qi Liangang, Liu Zongbao. Application of three-dimensional printing technology combined with bone cement in minimally invasive treatment of the collapsed Sanders III type of calcaneal fractures [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3784-3789. |
| [9] | Qian Xuankun, Huang Hefei, Wu Chengcong, Liu Keting, Ou Hua, Zhang Jinpeng, Ren Jing, Wan Jianshan. Computer-assisted navigation combined with minimally invasive transforaminal lumbar interbody fusion for lumbar spondylolisthesis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3790-3795. |
| [10] | Hu Jing, Xiang Yang, Ye Chuan, Han Ziji. Three-dimensional printing assisted screw placement and freehand pedicle screw fixation in the treatment of thoracolumbar fractures: 1-year follow-up [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3804-3809. |
| [11] | Shu Qihang, Liao Yijia, Xue Jingbo, Yan Yiguo, Wang Cheng. Three-dimensional finite element analysis of a new three-dimensional printed porous fusion cage for cervical vertebra [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3810-3815. |
| [12] | Wang Yihan, Li Yang, Zhang Ling, Zhang Rui, Xu Ruida, Han Xiaofeng, Cheng Guangqi, Wang Weil. Application of three-dimensional visualization technology for digital orthopedics in the reduction and fixation of intertrochanteric fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3816-3820. |
| [13] | Sun Maji, Wang Qiuan, Zhang Xingchen, Guo Chong, Yuan Feng, Guo Kaijin. Development and biomechanical analysis of a new anterior cervical pedicle screw fixation system [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3821-3825. |
| [14] | Lin Wang, Wang Yingying, Guo Weizhong, Yuan Cuihua, Xu Shenggui, Zhang Shenshen, Lin Chengshou. Adopting expanded lateral approach to enhance the mechanical stability and knee function for treating posterolateral column fracture of tibial plateau [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3826-3827. |
| [15] | Zhu Yun, Chen Yu, Qiu Hao, Liu Dun, Jin Guorong, Chen Shimou, Weng Zheng. Finite element analysis for treatment of osteoporotic femoral fracture with far cortical locking screw [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3832-3837. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||